NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Rilpivirine is a nonnucleoside reverse transcriptase inhibitor used in combination with other antiretroviral agents in the therapy of human immunodeficiency virus (HIV) infection. Rilpivirine is associated with a low rate of transient serum aminotransferase elevations during therapy and has been implicated in rare cases of clinically apparent acute liver injury.
Background
Rilpivirine (ril" pi vir' een) is an antiretroviral agent that acts by noncompetitive binding to, and inhibition of the HIV reverse transcriptase. Rilpivirine is a nonnucleoside reverse transcriptase inhibitor similar in action to nevirapine, efavirenz, delavirdine and etavirine. In several randomized controlled trials, rilpivirine was found to have similar efficacy to efavirenz when combined with at least two nucleoside analogues (typically tenofovir and emtricitabine). Rilpivirine was the fifth nonnucleoside reverse transcriptase inhibitor approved by the FDA [2011], and current indications are for the treatment of HIV infection in combination with other HIV medications. Rilpivirine is available under the brand name Edurant in tablets of 25 mg. The recommended dose is 25 mg orally once daily with a meal. Rilpivirine is also available in a fixed dose combination (25 mg) once a day tablet with emtricitabine (200 mg) and tenofovir disoproxil fumarate (300 mg) under the brand name Complera [2011] and a similar combination with tenofovir alafenamide fumarate (25 mg) under the brand name Odefsey [2016]. Antiviral resistance can occur and resistance patterns are similar to, and cross react with those due to other nonnucleoside reverse transcription inhibitors. Common side effects include fatigue, dizziness, headache, insomnia, depression and skin rashes.
Hepatotoxicity
Serum aminotransferase elevations occur in 25% or more of patients on rilpivirine therapy, but elevations above 5 times the upper limit of normal are uncommon, occurring in 1% to 4% of patients. The rate of serum aminotransferase elevations during rilpivirine therapy is higher in patients who are coinfected with hepatitis B or C [~10% have values greater than 5 times ULN]. The product label for rilpivirine induces a warning about hepatotoxicity particularly in patients with HBV or HCV coinfection and recommends monitoring for liver test abnormalities. During the first several years of wide spread clinical use of rilpivirine, a single case report of liver injury was published. The case was marked by prominent elevations in serum ALT and AST without jaundice arising within days of starting therapy and resolving rapidly upon stopping (Case 1). There was no rash, eosinophilia or other prominent immunoallergic features which are typical of the liver injury associated with nevirapine and efavirenz. Thus, clinically apparent hepatotoxicity due to rilpivirine may occur but is rare.
Liklihood score: D (possible rare cause of clinically apparent liver injury).
Mechanism of Injury
While hepatotoxicity from rilpivirine may be rare, it is likely due to hypersensitivity. Rilpivirine is extensively metabolized in the liver via the cytochrome P450 system (predominantly CYP 3A4) and production of a toxic or immunogenic intermediate may trigger liver injury.
Outcome and Management
The severity of the liver injury linked to rilpivirine therapy has been mild and self-limited and characterized by serum aminotransferase elevations with no or minimal symptoms and no rash. Recovery has been prompt upon drug discontinuation. Rilpivirine has not been linked to cases of acute liver failure, chronic hepatitis or vanishing bile duct syndrome. There is no information on cross sensitivity to hepatic injury between rilpivirine and other nonnucleoside reverse transcriptase inhibitors, although there may be cross reactivity in occurrence of rash.
Drug Class: Antiviral Agents, Antiretroviral Agents
Other Drugs in the Subclass, Nonnucleoside Reverse Transcriptase Inhibitors: Delavirdine, Doravirine, Efavirenz, Etravirine, Nevirapine
CASE REPORT
Case 1. Mild hepatitis arising within a few days of starting rilpivirine.
[Modified from: Ahmed Y, Siddiqui W, Enoch CB, Albrecht H, Bookstaver PB. Rare case of rilpivirine-induced severe allergic hepatitis. J Antimicrob Chemother 2012 Oct 12. [Epub ahead of print] PubMed Citation]
A 28 year old man with HIV and mycobacterium avium intracellulare complex (MAC) infection on long term antiretroviral therapy developed fatigue, nausea and fever within days of changing his antiviral regimen to include rilpivirine. He had a long history of HIV infection for which he had received various antiretroviral regimens that most recently had included tenofovir, emtricitabine, raltegravir and zidovudine. To simplify his regimen, he was switched to a once daily combination of rilpivirine, tenofovir and emtricitabine. His other medications included azithromycin and ethambutol for MAC infection, atovaquone for Pneumocystis jiroveci prophylaxis, and amlodipine and carvedilol for hypertension, all of which he had taken for more than a year. Within a few days of starting the new regimen, he developed progressive weakness, fatigue, nausea and fever. He had no recent exposures to viral hepatitis and had had normal routine liver tests in the past. He denied excessive alcohol intake. On examination, he was febrile (39.2 oC) and had tachycardia (102 beats/min), but was not jaundiced and had no rash or signs of chronic liver disease. Laboratory testing showed marked elevations in serum aminotransferase levels (ALT 1516 U/L, AST 5931) with mild increases in alkaline phosphatase (239 U/L), normal bilirubin (1.0 mg/dL), mild renal impairment (creatinine 2.5 mg/dL), and no eosinophils (Table). Tests for hepatitis A, B and C were negative as were blood alcohol and acetaminophen levels and a urine toxicology screen. All medications were stopped and he received supportive care and hydration. His liver test abnormalities improved rapidly and were almost normal by hospital day 16. His medications were then restarted, but the antiretroviral regimen was changed to tenofovir, emtricitabine, atazanavir, low dose ritonavir and raltegravir without rilpivirine. In follow up, his liver enzymes were normal.
Key Points
| Medication: | Rilpivirine (25 mg daily) |
| Pattern: | Hepatocellular (R=9.1) |
| Severity: | 1+ (no jaundice) |
| Latency: | 4 days |
| Recovery: | Complete in 4 weeks |
| Other medications: | Tenofovir, emtricitabine, atovaquone, ethambutol, azithromycin, carvedilol and amlodipine (all were later restarted without recurrence) |
Laboratory Values
Comment
A young man with HIV infection and MAC infection developed fever, fatigue and marked serum aminotransferase elevations within 4 days of starting rilpivirine. He was taking several other medications with a potential for hepatotoxicity, but rilpivirine was the only agent that was recently started. The mode of onset and clinical course resembled acute hepatic necrosis with sudden marked increases in ALT and AST, but minimal or no increase in alkaline phosphatase and bilirubin followed by a rapid decline upon stopping the drug. The INR and either LDH or CPK levels would have been helpful, but were not reported. The differential diagnosis for this clinical pattern includes acetaminophen overdose and acute cocaine toxicity, but toxicology screening ruled out these possibilities. Another possible diagnosis was shock, hypoxia or ischemia, but the history did not suggest such an episode (although the patient was clearly dehydrated upon presentation). The published case was described as "severe", but without jaundice or coagulation abnormalities it is more accurate to describe the case as mild or at most moderate in severity. Furthermore, the hepatitis was described as "allergic", but besides fever there were no other allergic features such as rash, facial edema, lymphadenopathy, lymphocytosis or eosinophilia. Immunoallergic hepatitis is typical of the hepatotoxicity of nevirapine and efavirenz, two first generation nonnucleoside reverse transcriptase inhibitors.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Rilpivirine – Edurant®
Rilpivirine, Emtricitabine, Tenofovir – Complera®
DRUG CLASS
Antiviral Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Rilpivirine | 500287-72-9 | C22-H18-N6 |
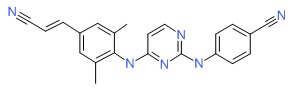 |
ANNOTATED BIBLIOGRAPHY
References updated: 20 February 2017
- Núñez M. Hepatic toxicity of antiviral agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 505-18.(Review of hepatotoxicity of antiviral agents without specifically mentioning rilpivirine).
- Flexner C. Antiretroviral agents and treatment of HIV infection. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1623-64.(Textbook of pharmacology and therapeutics).
- http://aidsinfo.nih.gov/guidelines.(Clinical guidelines on the use of antiretroviral agents in HIV-1 infected adults, adolescents and children).
- Sulkowski MS, Thomas DL, Chaisson RE, Moore RD. Hepatotoxicity associated with antiretroviral therapy in adults infected with human immunodeficiency virus and the role of hepatitis C or B virus infection. JAMA 2000; 283: 74-80. [PubMed: 10632283](Among 298 patients with HIV infection, ALT elevations above 5 times ULN occurred in 10.4% per year during antiretroviral treatment; factors associated with ALT elevations included ritonavir [27.3%] and coinfection with either HCV or HBV; ALT with bilirubin elevations occurred in 3 patients; 2 on indinavir and all 3 with coinfection).
- Dieterich DT, Robinson PA, Love J, Stern JO. Drug-induced liver injury associated with the use of nonnucleoside reverse-transcriptase inhibitors. Clin Infect Dis 2004; 38 Suppl 2: S80-9. [PubMed: 14986279](Review of hepatotoxicity of nonnucleoside reverse transcriptase inhibitors; rate of ALT elevations >5 times ULN is ~6% at 6 weeks, but thereafter is similar in nevirapine and placebo recipients, raising questions regarding the causality of late elevations; in meta analysis of 21 studies, ALT elevations >5 times normal occurred in 10.8% on efavirenz, 8.9% on nevirapine and only 3.6% on delaviridine; about half of elevations associated with symptoms).
- Torti C, Lapadula G, Casari S, Puoti M, Nelson M, Quiros-Roldan E, Bella D, et al.; EPOKA-MASTER Study Group. Incidence and risk factors for liver enzyme elevation during highly active antiretroviral therapy in HIV-HCV co-infected patients: results from the Italian EPOKA-MASTER Cohort. BMC Infect Dis 2005; 5: 58. [PMC free article: PMC1188059] [PubMed: 16018804](Among 1038 HIV-HCV coinfected patients starting antiretroviral therapy, the risk of ALT elevations above 5 times ULN was 17.1% yearly in treatment naï and 8.2% in treatment experienced patients; risk factors being baseline ALT levels and use of nonnucleoside reverse transcriptase inhibitors).
- Labarga P, Soriano V, Vispo ME, Pinilla J, Martin-Carbonero L, Castellares C, Casado R, et al. Hepatotoxicity of antiretroviral drugs is reduced after successful treatment of chronic hepatitis C in HIV-infected patients. J Infect Dis 2007; 196: 670-6. [PubMed: 17674307](Among 133 patients with HIV-HCV coinfection who were treated with interferon or peg interferon, 33% had a sustained response and subsequent yearly rate of hepatic events was higher among nonresponders [12.9%] than responders [3.1%]; also more common with receipt of di-deoxynucleosides).
- Jain MK. Drug-induced liver injury associated with HIV medications. Clin Liver Dis 2007; 11: 615-39, vii-viii. [PubMed: 17723923](Review of hepatotoxicity of antiretroviral medications; ALT elevations occur in 2-18% of patients, but often resolve spontaneously even without dose modification; classes of injury include hypersensitivity [nevirapine, efavirenz, abacavir], mitochondrial injury [stavudine, didanosine, zidovudine], flares of hepatitis B [lamivudine, emtricitabine, tenofovir], flares of hepatitis C [any potent regimen], idiosyncratic injury [ritonavir, nevirapine, efavirenz], cholestatic hepatitis [many agents]).
- Rivero A, Mira JA, Pineda JA. Liver toxicity induced by non-nucleoside reverse transcriptase inhibitors. J Antimicrob Chemother 2007; 59: 342-6. [PubMed: 17255142](Review of liver toxicity of nevirapine and efavirenz, ALT elevations >5 times ULN reported in 1-8% of efavirenz compared to 4-16% of nevirapine recipients; no mention of delavirdine or rilpivirine).
- Soriano V, Puoti M, Garcia-Gascó Rockstroh JK, Benhamou Y, Barreiro P, McGovern B. Antiretroviral drugs and liver injury. AIDS 2008; 22: 1-13. [PubMed: 18090386](Review of hepatotoxicity of antiretroviral drugs with recommendations on management, stopping therapy if symptoms arise, with overt jaundice [direct bilirubin], evidence of mitochondrial toxicity, ALT >10 times ULN, ALT at lower levels if newly marketed agent; important to rule out other causes; problematic agents include didanosine, stavudine and zidovudine; nevirapine and efavirenz, full dose ritonavir and tipranavir).
- Hughes CA, Robinson L, Tseng A, MacArthur RD. New antiretroviral drugs: a review of the efficacy, safety, pharmacokinetics, and resistance profile of tipranavir, darunavir, etravirine, rilpivirine, maraviroc, and raltegravir. Expert Opin Pharmacother 2009; 10: 2445-66. [PubMed: 19678794](Review of new antiretroviral agents including rilpivirine states that grade 3 or 4 adverse events and laboratory abnormalities were similar between rilpivirine and efavirenz treated patients with no specific discussion of hepatotoxicity or ALT elevations).
- Rilpivirine(Edurant).a new drug for HIV infection. Med Lett Drugs Ther 2011; 53 (1371): 67-8. [PubMed: 21860365](Concise review of the safety and efficacy of rilpivirine shortly after its approval in the US; common side effects include depression, insomnia, headache and rash; ALT elevations and hepatotoxicity are not mentioned).
- Molina JM, Cahn P, Grinsztejn B, Lazzarin A, Mills A, Saag M, Supparatpinyo K, et al.; ECHO study group. Rilpivirine versus efavirenz with tenofovir and emtricitabine in treatment-naive adults infected with HIV-1 (ECHO): a phase 3 randomised double-blind active-controlled trial. Lancet 2011; 378 (9787): 238-46. [PubMed: 21763936](Controlled trial of rilpivirine vs efavirenz [combined with tenofovir and emtricitabine] in 690 treatment naï subjects with HIV infection analyzed after 48 weeks; ALT elevations above 5 times ULN occurred in 1% of rilpivirine vs 4% of efavirenz treated patients, no mention of clinically apparent liver injury).
- Cohen CJ, Andrade-Villanueva J, Clotet B, Fourie J, Johnson MA, Ruxrungtham K, Wu H, et al.; THRIVE study group. Rilpivirine versus efavirenz with two background nucleoside or nucleotide reverse transcriptase inhibitors in treatment-naive adults infected with HIV-1 (THRIVE): a phase 3, randomised, non-inferiority trial. Lancet 2011; 378(9787): 229-37. [PubMed: 21763935](Controlled trial of 96 weeks of rilpivirine vs efavirenz [combined with two nucleoside analogues] in 680 subjects with HIV infection showed similar efficacy but fewer side effects with rilpivirine, discontinuations in 4% vs 7%, ALT elevations above 5 times ULN in 2% vs 3%, and no mention of clinically apparent liver injury).
- Sharma M, Saravolatz LD. Rilpivirine: a new non-nucleoside reverse transcriptase inhibitor. J Antimicrob Chemother 2012 Oct 29. [Epub ahead of print] [PubMed: 23099850](Review of pharmacology, efficacy and safety of rilpivirine; no discussion of ALT elevations or hepatotoxicity).
- Ahmed Y, Siddiqui W, Enoch CB, Albrecht H, Bookstaver PB. Rare case of rilpivirine-induced severe allergic hepatitis. J Antimicrob Chemother 2012 Oct 12. [Epub ahead of print] [PubMed: 23065700](28 year old man with HIV infection developed fever and fatigue within days of adding rilpivirine to his antiviral regimen [bilirubin 1.0 mg/dL, ALT 1516 U/L, Alk P 293 U/L], improving rapidly and liver tests being normal within 16 days of stopping; Case 1).
- Patel N, Miller CD. New option for management of HIV-1 infection in treatment-naive patients: once-daily, fixed-dose combination of rilpivirine-emtricitabine-tenofovir. HIV AIDS (Auckl) 2012; 4: 61-71. [PMC free article: PMC3346062] [PubMed: 22570576](Review of safety and efficacy of rilpivirine and its fixed dose combination with tenofovir and emtricitabine as therapy of HIV infection; no discussion of ALT elevations or hepatotoxicity).
- James C, Preininger L, Sweet M. Rilpivirine: a second-generation nonnucleoside reverse transcriptase inhibitor. Am J Health Syst Pharm 2012; 69: 857-61. [PubMed: 22555080](Review of the pharmacology, efficacy and safety of rilpivirine in HIV infection; no discussion of ALT elevations or hepatotoxicity).
- Nelson M, Amaya G, Clumeck N, Arns da Cunha C, Jayaweera D, Junod P, Li T, Tebas P, et al.; ECHO and THRIVE Study Groups. Efficacy and safety of rilpivirine in treatment-naive, HIV-1-infected patients with hepatitis B virus/hepatitis C virus coinfection enrolled in the Phase III randomized, double-blind ECHO and THRIVE trials. J Antimicrob Chemother 201; 67: 2020-8. [PMC free article: PMC4643643] [PubMed: 22532465](Pooled analysis of 2 controlled trials of rilpivirine vs efavirenz for their safety and efficacy in subgrounds of patients with HIV/HBV [n=55] and HIV/HCV [n=57] coinfection; ALT elevations occurred in 11.1% on rilpivirine vs 10.6% on efavirenz in coinfected compared to 1.1% vs 1.9% in noncoinfected patients; there was 1 case of acute hepatitis in each group; discontinuations for hepatic adverse events were reported in 3 rilpivirine vs 9 efavirenz treated subjects).
- Cohen CJ, Molina JM, Cahn P, Clotet B, Fourie J, Grinsztejn B, Wu H, et al.; ECHO Study Group; THRIVE Study Group. Efficacy and safety of rilpivirine (TMC278) versus efavirenz at 48 weeks in treatment-naï HIV-1-infected patients: pooled results from the phase 3 double-blind randomized ECHO and THRIVE Trials. J Acquir Immune Defic Syndr 2012; 60: 33-42. [PubMed: 22343174](Pooled analysis of 3 controlled trials of 48 weeks of rilpivirine [n=686] vs efavirenz [n=682] in HIV infection; efficacy was similar, but adverse events were fewer with rilpivirine, including lower rates of grade 2 ALT elevations [5% vs 8%]; no mention of clinically apparent liver injury).
- Wilkin A, Pozniak AL, Morales-Ramirez J, Lupo SH, Santoscoy M, Grinsztejn B, Ruxrungtham K, et al.; TMC278-C204 Study Group. Long-term efficacy, safety, and tolerability of rilpivirine (RPV, TMC278) in HIV type 1-infected antiretroviral-naive patients: week 192 results from a phase IIb randomized trial. AIDS Res Hum Retroviruses 2012; 28: 437-46. [PubMed: 21902621](Analysis of efficacy and safety of open label, long term, extended therapy [192 weeks] with rilpivirine [n=279] vs efavirenz [n=89] with 2 nucleoside analogues; ALT elevations were reported in 6% of both groups, mostly occurring during the first 48 weeks of therapy; no mention of clinically apparent liver injury).
- Casado JL. Liver toxicity in HIV-infected patients receiving novel second-generation nonnucleoside reverse transcriptase inhibitors etravirine and rilpivirine. AIDS Rev 2013; 15: 139-45. [PubMed: 24002197](Review of the liver toxicity of etravirine and rilpivirine compared to efavirenz and other NNRTIs concludes that both new agents have low rates of liver toxicity and can be used safely in patients with HCV coinfection).
- Surgers L, Lacombe K. Hepatoxicity of new antiretrovirals: a systematic review. Clin Res Hepatol Gastroenterol 2013; 37: 126-33. [PubMed: 23522569](Systematic review of rates of liver injury reported in clinical trials of recently approved antiretroviral agents including rilpivirine).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-1352.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 12 were attributed to antiretroviral agent, but none to rilpivirine).
- Gianotti N, Poli A, Nozza S, Spagnuolo V, Tambussi G, Bossolasco S, Cinque P, et al. Efficacy and safety in clinical practice of a rilpivirine, tenofovir and emtricitabine single-tablet regimen in virologically suppressed HIV-positive patients on stable antiretroviral therapy. J Int AIDS Soc 2015; 18: 20037. [PMC free article: PMC4522018] [PubMed: 26232000](Among 307 patients with HIV infection on antiviral regimens who were switched to the single tablet regimen of rilpivirine, tenofovir and emtricitabine [Complera], virologic failure occurred in only 3 patients [1%] and there were only minor changes in median serum ALT, Alk P and bilirubin levels; no mention of clinically apparent liver injury).
- Neukam K, Espinosa N, Collado A, Delgado-Fernández M, Jiménez-Aguilar P, Rivero-Juárez A, Hontañón-Antoñana V, et al.; hEPAtic Study Group. Hepatic safety of rilpivirine/emtricitabine/tenofovir disoproxil fumarate fixed-dose single-tablet regimen in HIV-infected patients with active hepatitis C virus infection: the hEPAtic Study. PLoS One 2016; 11: e0155842. [PMC free article: PMC4873169] [PubMed: 27195797](Retrospective analysis of 173 patients coinfected with HIV and HCV who started combination therapy with rilpivirine, emtricitabine and tenofovir [RET] and 346 controls found incidence of serum enzyme elevations above 5 times ULN to be only 1.2% with RET and 3.2% in controls on various regimens, while liver related deaths occurred in 0.6% vs 0.2% in controls).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Doravirine.[LiverTox: Clinical and Researc...]Review Doravirine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Rilpivirine: a second-generation nonnucleoside reverse transcriptase inhibitor.[Am J Health Syst Pharm. 2012]Rilpivirine: a second-generation nonnucleoside reverse transcriptase inhibitor.James C, Preininger L, Sweet M. Am J Health Syst Pharm. 2012 May 15; 69(10):857-61.
- Review Delavirdine.[LiverTox: Clinical and Researc...]Review Delavirdine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Cabotegravir.[LiverTox: Clinical and Researc...]Review Cabotegravir.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review The role of rilpivirine in clinical practice: strengths and weaknesses of the new nonnucleoside reverse transcriptase inhibitor for HIV therapy.[AIDS Rev. 2012]Review The role of rilpivirine in clinical practice: strengths and weaknesses of the new nonnucleoside reverse transcriptase inhibitor for HIV therapy.Imaz A, Podzamczer D. AIDS Rev. 2012 Oct-Dec; 14(4):268-78.
- Rilpivirine - LiverToxRilpivirine - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...