NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Nevirapine is a nonnucleoside reverse transcriptase inhibitor used in combination with other agents in the therapy of human immunodeficiency virus (HIV) infection and the acquired immune deficiency syndrome (AIDS). Nevirapine is associated with a high rate of serum aminotransferase elevations during therapy and is a well established cause of acute, clinically apparent liver injury.
Background
Nevirapine (ne vir' a peen) is a nonnucleoside inhibitor of the HIV polymerase enzyme and acts by binding to and disrupting the active catalytic site of the viral polymerase, causing a conformational change in the three dimensional structure of the enzyme. Nevirapine is a potent inhibitor of HIV replication and is a major component of highly reactive antiretroviral therapy (HAART) commonly being given in combination with one or two nucleoside reverse transcriptase inhibitors. Nevirapine was approved for use in HIV infection in the United States in 1996 and is currently used in a high proportion of HAART regimens. Nevirapine is available in generic forms and under the brand name of Viramune in standard tablets of 200 mg and extended release tablets of 400 mg. The usual adult dose is 200 mg once daily for 2 weeks followed by standard 200 mg tablets twice daily or extended release tablets of 400 mg once daily. Nevirapine is used in combination with other antiretroviral agents and is available in combinations with zidovudine and lamivudine. An oral suspension is also available for use in pediatrics. Common side effects include rash (~20%), nausea, fatigue, fever and headache. Uncommon but severe adverse reactions include hepatotoxicity, severe skin reactions, hypersensitivity reactions, immune reconstitution syndrome, and abnormal fat distribution.
Hepatotoxicity
Therapy with nevirapine is associated with significant elevations in ALT levels (above 5 times the upper limit of normal) in 4% to 20% of patients and symptomatic elevations in 1% to 5% of patients. These elevations are usually transient but can be symptomatic and may require discontinuation of nevirapine. Risk factors for ALT elevations include preexisting liver disease due to HCV or HBV, and possibly female gender, CD4 T cell counts above 250/μL, and absence of HIV infection (such as when given for prophylaxis after an acute exposure). In addition, among the more than 20 antiretroviral agents in current use, nevirapine is perhaps the most common cause of serious, clinically apparent acute liver injury. The frequency of clinically apparent liver injury due to nevirapine is as high as 1%, with fatalities occurring in approximately 0.1% of treated patients. The onset of injury is almost always within the first 6 to 8 weeks of therapy (average 3 weeks) and presenting symptoms are typically abdominal pain and fatigue, followed by fever, rash and jaundice. A large proportion of patients have features of immunoallergic hepatitis (nevirapine hypersensitivity syndrome) with rash, fever and eosinophilia (Cases 2 and 3). Autoantibodies are not common. Most instances have cholestatic features, but initial serum enzyme elevations may be hepatocellular in pattern, particularly in severe cases (Case 1). The associated rash can be severe and compatible with toxic epidermal necrosis or Stevens-Johnson syndrome. Some cases of clinically apparent hepatotoxicity due to nevirapine are not associated with signs of hypersensitivity, and these generally present after the first 8 weeks of therapy but can be severe and even fatal.
Likelihood score: A (well known cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism of hepatic injury with nevirapine is believed to be immunoallergic. Hepatic injury is more common among women than men and in patients with higher CD4 T cell counts and has been associated with specific HLA types. However, not all cases of nevirapine hepatotoxicity may be immunoallergic in origin, particularly those with a longer latency period to onset. Nevirapine has extensive hepatic metabolism and is a substrate for CYP 2B6 and 3A4 and a potent inducer of these enzymes, features that favor potential production of a toxic intermediate that might cause liver injury.
Outcome and Management
Nevirapine hepatotoxicity can be severe and fatal instances as well as cases requiring emergency liver transplantation have been described. In large case series, nevirapine is usually listed in the major causes of drug induced acute liver failure. The nevirapine product label includes a boxed warning about hepatotoxicity and recommends regular monitoring for liver test abnormalities before and at least monthly for the first 18 weeks of treatment. Some degree of ALT elevation arises in up to 25% of patients treated with nevirapine-containing antiretroviral regimens which usually resolve even with continuation of therapy. Nevirapine should be promptly discontinued if serum aminotransferase levels rise about 10 times ULN or are persistently above 5 times ULN or if accompanied by bilirubin elevations or symptoms of hepatitis. Patients with nevirapine hepatotoxicity should not be restarted on treatment. There appears to be little if any cross sensitivity to hepatotoxicity among the other antiretroviral agents, including other nonnucleoside reverse transcriptase inhibitors such as efavirenz, etravine, delavirdine and rilpivirine.
Drug Class: Antiviral Agents, Antiretroviral Agents
Other Drugs in the Subclass, Nonnucleoside Reverse Transcriptase Inhibitors: Delavirdine, Doravirine, Efavirenz, Etravirine, Rilpivirine
CASE REPORTS
Case 1. Severe acute hepatitis due to nevirapine.(1)
A 28 year old woman with HIV infection [CD4 count 255 cells/µL; HIV level 100,000 copies/mL] was started on antiretroviral therapy consisting of zidovudine, lamivudine and nevirapine and developed nausea and headache followed by jaundice and pruritus 6 weeks later. On presentation, she was jaundiced without fever or rash. There were marked elevations in serum aminotransferase levels with bilirubin of 11.2 mg/dL, a prothrombin index of 28%, no eosinophilia and mild lactic acidemia (Table). Liver tests had been normal before therapy. Tests for hepatitis A, B, C and E were negative as were auto-antibodies. Serum copper and ceruloplasmin levels were normal. Ultrasonography and CT scans of the abdomen were unremarkable. She had taken acetaminophen [3 g/day] for the 2 days before presentation and acetaminophen levels were 11 mg/L. Nevirapine was stopped and she was given infusions of N-acetylcysteine. Nevertheless, she deteriorated rapidly developing stage 2 encephalopathy. A liver biopsy showed massive necrosis with portal inflammation and bile duct proliferation. There was no microvesicular fat, and no findings of chronic liver disease. Serum aminotransferase levels fell but the prothrombin index worsened and she underwent liver transplantation 3 days after admission. She had an uneventful post-transplant course and was placed on efavirenz, abacavir and lamivudine 15 days later. In follow up 3 months later, her liver tests were normal.
Key Points
| Medication: | Nevirapine (200 mg daily) |
|---|---|
| Pattern: | Hepatocellular (R>100) |
| Severity: | 5+ (liver transplantation) |
| Latency: | 6 weeks |
| Recovery: | None |
| Other medications: | Lamivudine, zidovudine, 2 days of acetaminophen |
Laboratory Values
| Time After Starting | Time After Stopping | ALT (U/L) | GGT (U/L) | Bilirubin (mg/dL) | Other |
|---|---|---|---|---|---|
| Pre | 20 | Normal | |||
| 0 | Pre | Nevirapine, lamivudine and zidovudine started | |||
| 6 weeks | 0 | 12578 | 340 | 11.2 | INR=3.2 |
| 1 day | 1804 | INR=6.3, Encephalopathy | |||
| Emergency liver transplantation done on day 3 of admission | |||||
| 7 weeks | 4 days | 2650 | |||
| 5 months | 3 months | 35 | |||
| Normal Values | <40 | <130 | <1.2 | ||
Comment
A typical timing for onset of nevirapine hepatotoxicity with a hepatocellular pattern of serum enzyme elevations. Unlike many cases, there were no signs or findings of hypersensitivity (rash, fever, lymphadenopathy, facial edema, eosinophilia). Furthermore, she had taken full doses of acetaminophen for two days before presentation and there may have been an element of superimposed acetaminophen hepatotoxicity (explaining the initial, very high ALT levels and marked centrolobular necrosis). In follow up, she was treated with efavirenz (another nonnucleoside reverse transcriptase inhibitor) without evidence of recurrence of hepatic injury.
Case 2. Acute immunoallergic hepatitis due to nevirapine.(2)
A 26 year old pregnant woman with HIV infection developed fever and skin rash 6 weeks after starting antiretroviral therapy with nevirapine, lamivudine and zidovudine. Before therapy, her CD4 count was 614 cells/µL, HIV RNA level was 1642 copies/mL, and liver tests were normal. On admission at 32 weeks gestation, she was febrile and jaundiced and had a diffuse urticarial rash. Laboratory tests showed eosinophilia and a cholestatic pattern of serum enzyme elevation (Table). Tests for hepatitis A, B and C and for EBV and CMV infection were negative, as were autoantibodies. Ultrasound of the liver showed no evidence of obstruction. Nevirapine was stopped and she was given corticosteroids. Over the next few days she continued to worsen and emergency Caesarian section was done. Thereafter, she began to improve and was discharged 4 days after delivery. In follow up, she was asymptomatic, had normal liver test results and the child was well and without evidence of HIV infection.
Key Points
| Medication: | Nevirapine (200→400 mg daily) |
|---|---|
| Pattern: | Cholestatic (R=1.6) |
| Severity: | 4+ (jaundice, hospitalization and features of hepatic failure) |
| Latency: | 6 weeks |
| Recovery: | Complete |
| Other medications: | Lamivudine, zidovudine, 2 days of acetaminophen |
Laboratory Values
| Time After Starting | Time After Stopping | ALT (U/L) | Alk P (U/L) | Bilirubin (mg/dL) | Other |
|---|---|---|---|---|---|
| Pre | 14 | 0.4 | |||
| 2 weeks | 14 | 77 | 0.4 | ||
| 6 weeks | 0 | 235 | 257 | 12.0 | INR 2.4, given betamethasone |
| 2 days | 404 | 175 | 15.3 | INR 3.6, fresh frozen plasma | |
| 4 days | 966 | 201 | 19.4 | Fever, 20% eosinophilia | |
| Emergency Caesarian Section | |||||
| 7 weeks | 6 days | 746 | 239 | 20.2 | Oral prednisone |
| 8 days | 696 | 466 | 16.9 | ||
| 8 weeks | 2 weeks | 509 | 500 | 7.0 | Discharged |
| 6 months | 4 months | 18 | 73 | 0.4 | |
| Normal Values | <61 | <106 | <1.2 | ||
Comment
A very characteristic example of the DRESS syndrome (drug rash with eosinophilia and systemic symptoms) due to nevirapine in a woman with HIV infection and a CD4 count above 250/µL. The associated immunoallergic hepatitis was severe with bilirubin levels reaching 20 mg/dL and prolongation of prothrombin time. While the clinical course was also compatible with pregnancy associated HELPP syndrome, the timing and immunoallergic features suggest that nevirapine was the major cause. Women may be more susceptible to the immunoallergic hepatitis caused by nevirapine, and pregnancy may increase the risk further. Corticosteroids are often used in patients with severe immunoallergic hepatitis and they appear to improve many of the manifestations of hypersensitivity, but their efficacy in altering the ultimate outcome of the liver injury has not been proven.
Case 3. Acute immunoallergic hepatitis due to nevirapine.(3)
A 31 year old man with HIV-HCV coinfection developed a diffuse maculopapular rash within 7 days of switching antiretroviral therapy from zidovudine and didanosine to nevirapine (200 mg daily), lamivudine (150 mg twice daily) and stavudine (40 mg twice daily). All three drugs were stopped and the rash resolved rapidly. Ten days later, all three agents were restarted, but rash and fever (to 39o C) appeared two days later followed by myalgias, dark urine, jaundice and pruritus. Laboratory testing showed eosinophilia, elevations in serum enzymes and hyperbilirubinemia (Table). All three drugs were stopped, and he was monitored carefully. Ultrasound of the abdomen showed no evidence of biliary obstruction. Symptoms resolved and laboratory abnormalities resolved rapidly. Serum ALT levels, which had been minimally elevated before nevirapine therapy, returned to the pretreatment levels. He was restarted on lamivudine, stavudine and indinavir without reappearance of rash or jaundice.
Key Points
| Medication: | Nevirapine (200 mg daily) |
|---|---|
| Pattern: | Cholestatic (R=1.3) |
| Severity: | 3+ (jaundice, hospitalization) |
| Latency: | 20 days from first exposure; 3 days on reexposure |
| Recovery: | Complete by 3 weeks |
| Other medications: | Lamivudine, stavudine |
Laboratory Values
| Time After Starting | Time After Stopping | ALT (U/L) | Alk P (U/L) | Bilirubin (mg/dL) | Other |
|---|---|---|---|---|---|
| 0 | 63 | 75 | 0.3 | Known chronic hepatitis C | |
| 1 week | Rash: Antiretroviral drugs stopped | ||||
| 3 weeks | Nevirapine, lamivudine and stavudine restarted | ||||
| 3 days | 0 | 224 | 501 | 12.7 | Rash, fever, 30% eosinophils |
| 10 days | 7 days | 163 | 263 | 2.9 | |
| 23 days | 20 days | 55 | 85 | 0.2 | |
| Normal Values | <40 | <115 | <1.2 | ||
Comment
A very characteristic example of drug rash with eosinophilia and hepatic injury due to a nevirapine in a patient with HIV and HCV infection. The injury was characterized by a mild cholestatic pattern with rapid recovery with stopping therapy. While a large proportion of patients develop rash with nevirapine therapy (usually within the first 3 weeks of starting), only a proportion (~10 to 20%) develop serum ALT elevations at the time of the rash, and an even smaller proportion (~1 to 5%) develop clinically apparent liver injury and jaundice. Hepatitis C may predispose to clinically apparent liver injury but, in this instance, HCV did not appear to play a role. Persons who develop a rash on nonnucleoside reverse transcriptase inhibitors should be monitored for serum ALT levels; but often can remain on therapy, the rash resolving despite continuing the agent. The presence of marked serum ALT elevations or symptoms should lead to stopping therapy.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Nevirapine – Generic, Viramune®
DRUG CLASS
Antiviral Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Nevirapine | 129618-40-2 | C15-H14-N4-O |
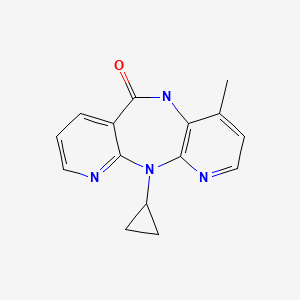
|
CITED REFERENCES
- 1.
- Buyse S, Vibert E, Sebagh M, Antonini T, Ichai P, Castaing D, Samuel D, Duclos-Vallée JC. Liver transplantation for fulminant hepatitis related to nevirapine therapy. Liver Transpl. 2006;12:1880–2. [PubMed: 17133571]
- 2.
- Knudtson E, Para M, Boswell H, Fan-Havard P. Drug rash with eosinophilia and systemic symptoms syndrome and renal toxicity with a nevirapine-containing regimen in a pregnant patient with human immunodeficiency virus. Obstet Gynecol. 2003;101(5 Pt 2):1094–7. [PubMed: 12738113]
- 3.
- Claudio GA, Martin AF, de Dios Perrino S, Velasco AA. DRESS syndrome associated with nevirapine therapy. Arch Intern Med. 2001;161:2501–2. [PubMed: 11700164]
ANNOTATED BIBLIOGRAPHY
References updated: 10 May 2020
- Abbreviations: AIDS, acquired immunodeficiency syndrome; DRESS, drug rash with eosinophilia and systemic symptoms; HIV, human immunodeficiency virus.
- Núñez M. Hepatic toxicity of antiviral agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 505-18.(Review of hepatotoxicity of antiviral agents mentions that nevirapine is the antiretroviral agent that is most commonly implicated in causing liver injury).
- Flexner C. Antiretroviral agents and treatment of HIV infection. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1137-58.(Textbook of pharmacology and therapeutics).
- NIH. HIV Info. https:
//clinicalinfo .hiv.gov/en/guidelines. (Clinical guidelines on the use of antiretroviral agents in HIV-1 infected adults, adolescents and children). - Havlir D, Cheeseman SH, McLaughlin M, Murphy R, Erice A, Spector SA, Greenough TC, et al. High-dose nevirapine: safety, pharmacokinetics, and antiviral effect in patients with human immunodeficiency virus infection. J Infect Dis. 1995;171:537–45. [PubMed: 7533197](Among 21 patients with HIV infection given 400 mg of nevirapine daily for 12 weeks, 48% developed rash, usually within first 3 weeks and not in association with ALT elevations, which arose in 3 patients [14%]).
- Carr A, Vella S, de Jong MD, Sorice F, Imrie A, Boucher CA, Cooper DA., Dutch-Italian-Australian Nevirapine Study Group. A controlled trial of nevirapine plus zidovudine versus zidovudine alone in p24 antigenaemic HIV-infected patients. AIDS. 1996;10:635–41. [PubMed: 8780818](Among 25 patients given nevirapine and zidovudine, 8 developed fever and rash [32%] usually within 28 days; one had ALT elevations above 5 times ULN; all resolved with stopping).
- D’Aquila RT, Hughes MD, Johnson VA, Fischl MA, Sommadossi JP, Liou SH, Timpone J, et al. Nevirapine, zidovudine, and didanosine compared with zidovudine and didanosine in patients with HIV-1 infection. Ann Intern Med. 1996;124:1019–30. [PubMed: 8633815](Trial of zidovudine and didanosine with or without nevirapine for 48 weeks in 398 patients with HIV infection; severe rash occurred in 2% without vs 9% with nevirapine, and AST elevations >5 times normal occurred in 4.5% vs 8%).
- Reiter GS. Hepatitis in an HIV-infected man. AIDS Clin Care. 1997;9:78–81. [PubMed: 11364758](28 year old man developed malaise and fever 3 weeks after starting nevirapine [with stavudine and lamivudine] with subsequent jaundice [bilirubin 11.8 rising to 17.9 mg/dL, ALT 480 U/L, Alk P 133 U/L], ultimately resolving after stopping medications).
- Havlir DV, Lange JM. New antiretrovirals and new combinations. AIDS 1998; 12 Suppl A: S165-74. [PubMed: 9632999](Review of new agents, including nelfinavir, nevirapine, delavirdine, efavirenz and abacavir; most significant toxicities discussed include diarrhea for nelfinavir, rash and hepatitis for nevirapine, rash for delavirdine).
- Warren KJ, Boxwell DE, Kim NY, Drolet BA. Nevirapine-associated Stevens-Johnson syndrome. Lancet. 1998;351:567. [PubMed: 9492778](31 year old man developed severe rash 10 days after starting nevirapine [with lamivudine and zidovudine] with fever, oral and corneal ulcers [6% eosinophilia, normal “chemistries”], mentions that FDA has received 20 reports of hospitalization due to rash caused by nevirapine).
- Montaner JS, Reiss P, Cooper D, Vella S, Harris M, Conway B, Wainberg MA, et al. INCAS Study Group. A randomized double-blind trial comparing combinations of nevirapine, didanosine, and zidovudine for HIV-infected patients. The INCAS Trial. JAMA. 1998;279:930–7. [PubMed: 9544767](Among 151 patients in a randomized controlled trial, rash occurred in 22% on nevirapine [no Stevens Johnson syndrome], 27% had liver test elevations, 5% required stopping, but all ultimately resolved).
- Bourezane Y, Salard D, Hoen B, Vandel S, Drobacheff C, Laurent R. DRESS (drug rash with eosinophilia and systemic symptoms) syndrome associated with nevirapine therapy. Clin Infect Dis. 1998;27:1321–2. [PubMed: 9827291](32 year old man with HIV infection developed rash 15 days and fever 34 days after starting nevirapine, stavudine and indinavir [bilirubin not mentioned, ALT 1072 U/L, Alk P 229 U/L, 18% eosinophils], resolving promptly with stopping nevirapine and corticosteroid therapy).
- Pollard RB, Robinson P, Dransfield K. Safety profile of nevirapine, a nonnucleoside reverse transcriptase inhibitor for the treatment of human immunodeficiency virus infection. Clin Ther. 1998;20:1071–92. [PubMed: 9916603](Experience in 906 adults and 468 children in clinical trials of nevirapine; rash occurred in 16%, which was reduced by starting with lower doses; ALT elevations >250 U/L occurred in 11%; clinical hepatitis in 1% usually in first 5 weeks; no additional cases in long term treatment groups).
- Leitze Z, Nadeem A, Choudhary A, Saul Z, Roberts I, Manthous CA. Nevirapine-induced hepatitis treated with corticosteroids? AIDS. 1998;12:1115–7. [PubMed: 9662216](36 year old with HIV and HCV infection developed fever and rash 4 weeks after starting nevirapine [bilirubin 2.0 mg/L, ALT 1424 U/L, Alk P 777 U/L, 13% eosinophils], responding rapidly to methylprednisolone).
- Ho TTY, Wong KH, Chan KCW, Lee SS. AIDS. 1998;12:2082–3. [PubMed: 9814883](5 of 8 Chinese patients treated with nevirapine developed rash within 8 weeks of starting: 4 had abnormal liver tests [bilirubin 1.3-7.3 mg/dL, ALT 93-266 U/L, Alk P 48-608 U/L], all resolving upon stopping drug).
- Cattelan AM, Erne E, Salatino A, Trevenzoli M, Carretta G, Meneghetti F, Cadrobbi P. Severe hepatic failure related to nevirapine treatment. Clin Infect Dis. 1999;29:455–6. [PubMed: 10476768](61 year old man developed jaundice, fever and rash 2 weeks after starting nevirapine [bilirubin 3.6 mg/dL, ALT 337 U/L, Alk P 237 U/L, protime 35%, eosinophils 46%], developing moderate ascites, but recovering within 2 months of stopping).
- Orenstein R, LeGall-Salmon E. HIV treatment-associated hepatitis. AIDS Read. 1999;9:339–46. [PubMed: 12737123](Review of antiretrovirals and liver injury; nevirapine causes hepatitis in 8-28% of patients, causing >5 fold elevation in ALT in 15% of patients and being cause of withdrawal in 5% in INCAS trial).
- Wetterwald E, Le Cleach I, Michel C, David F, Pevuz J. Nevirapine-induced overlap Stevens-Johnson syndrome/toxic epidermal necrolysis. Br J Dermatol. 1999;140:980–2. [PubMed: 10354056](Two cases of Stevens-Johnson toxic epidermal necrolysis-like syndromes during nevirapine therapy; 35 and 40 year old HIV infected patients developed generalized rash and blisters with oral involvement 13 and 25 days after starting nevirapine; ALT levels >4 times normal in one patient; both recovered and no mention of jaundice).
- Johnson S, Baraboutis JG. Adverse effects associated with use of nevirapine in HIV postexposure prophylaxis for 2 health care workers. JAMA. 2000;284:2722. [PubMed: 11105175](33 year old nurse given lamivudine, zidovudine and nevirapine after needlestick exposure to HIV developed nausea 8 days later with fever, adenopathy and rash, with response to corticosteroids, but relapse after stopping [ALT 215 U/L], responding to second course of prednisone).
- Sha BE, Proia LA, Kessler HA. Adverse effects associated with use of nevirapine in HIV postexposure prophylaxis for 2 health care workers. JAMA. 2000;284:2723. [PubMed: 11105176](43 year old phlebotomist given zidovudine, lamivudine and nevirapine for needlestick exposure to HIV developed liver test abnormalities at day 20 [bilirubin 1.3 mg/dL, ALT 1080 U/L and Alk P 150 U/L], progressing to hepatic failure, coma and liver transplantation at day 35).
- Piroth L, Grappin M, Sgro C, Buisson M, Duong M, Chavanet P. Recurrent NNRTI-induced hepatotoxicity in an HIV-HCV-coinfected patient. Ann Pharmacother. 2000;34:534–5. [PubMed: 10772444](31 year old woman with HIV-HCV coinfection developed enzyme elevations [ALT 772 U/L, GGT 1537 U/L] 5 weeks after starting nevirapine, resolving within 4 weeks of stopping, but recurring within 2 weeks of starting efavirenz [ALT 551 U/L, GT 2800 U/L], ultimately resolving within 2 months of stopping both; no mention of bilirubin or symptoms).
- Sissoko D, Ajana F, de la Tribonniere X, Baclet V, Mouton Y. Manifestations cutanees, hepatiques et hematologiques liees a la nevirapine: DRESS syndrome? Presse Med. 2000;29:1041–2. [PubMed: 10874910](2 women and 1 man, ages 35 to 45 years, developed rash, fever and liver injury 3-5 weeks after starting nevirapine for HIV infection [bilirubin 1.5 and 1.4 mg/dL, ALT 5,100, 1,225 and 172 U/L, Alk P 145, 416 and 220 U/L, eosinophilia in all], resolving rapidly and completely in all with corticosteroid therapy).
- Palacios R, Santos J, González M, Márquez M. Med Clin(Barc). 2000;114:597–8. [Hepatitis and nevirapine] [PubMed: 10846681](Among 163 patients with HIV infection started on nevirapine between 1997 and 1999, 5 developed clinically significant hepatitis after 21-24 days in 4 and after 85 days in 1 [bilirubin 2.5-17 mg/dL, ALT 146-854 U/L, Alk P 167-388 U/L], all resolving within 4 weeks of stopping).
- Sulkowski MS, Thomas DL, Chaisson RE, Moore RD. Hepatotoxicity associated with antiretroviral therapy in adults infected with human immunodeficiency virus and the role of hepatitis C or B virus infection. JAMA. 2000;283:74–80. [PubMed: 10632283](Among 298 patients with HIV infection, ALT elevations above 5 times ULN occurred in 10.4% during antiretroviral treatment; factors associated with ALT elevations included full dose ritonavir therapy and coinfection with either HCV or HBV).
- Velasco M, Guijarro C. Elevated liver enzymes following initiation of antiretroviral therapy. JAMA. 2000;283:2526–7. [PubMed: 10815112](Letter in response to Sulkowski et al. [JAMA 2000] pointing out that antiretroviral therapy can cause immune reconstitution and flares of hepatitis B or C which may be misdiagnosed as hepatotoxicity).
- Sulkowski MS, Thomas DL, Chaisson RE, Moore RD. Elevated liver enzymes following initiation of antiretroviral therapy. JAMA. 2000;283:2526–7. [PubMed: 10815113](Reply to Velasco and Guijarro pointing at that the majority of the ALT elevations described could not be attributed to immune reconstitution).
- Puoti M, Gargiulo F, Roldan EQ, Chiodera A, Palvarini L, Spinetti A, Zaltron S, et al. Liver damage and kinetics of hepatitis C virus and human immunodeficiency virus replication during the early phases of combination antiretroviral treatment. J Infect Dis. 2000;181:2033–6. [PubMed: 10837187](Monitoring viral levels during initiation of antiretroviral therapy with either nevirapine or indinavir combined with lamivudine and stavudine in 12 patients with HIV-HCV coinfection found slight rise in HCV RNA levels during weeks 1-3 of therapy, with no consistent change in ALT).
- Clarke S, Harrington P, Barry M, Mulcahy F. The tolerability of efavirenz after nevirapine-related adverse events. Clin Infect Dis. 2000;31:806–7. [PubMed: 11017835](Among 8 patients stopping nevirapine because of toxicity including 3 with ALT elevations [>5 times ULN], none developed liver toxicity and only one had any symptoms [facial edema] after switching to efavirenz).
- Clarke S, Harrington P, Condon C, Kelleher D, Smith OP, Mulcahy F. Late onset hepatitis and prolonged deterioration in hepatic function associated with nevirapine therapy. Int J STD AIDS. 2000;11:336–7. [PubMed: 10824944](49 year old man developed fatigue and jaundice [without fever or rash] 5 months after starting nevirapine, stavudine and didanosine for HIV infection [bilirubin 7.6 rising to 30.4 mg/dL, AST 544 U/L, Alk P 133 U/L], resolving within a few months of stopping).
- García Fernández D, García-Patos Briones V, Mollet Sánchez J, Castells Rodellas A. Rev Clin Esp. 2000;200:179–80. [Stevens-Johnson syndrome due to nevirapine] [PubMed: 10804771](35 year old man with HIV-HCV coinfection developed severe rash, fever and eosinophilia 1 month after starting nevirapine, didanosine and stavudine [bilirubin normal, ALT 143 U/L, Alk P 274 U/L], resolving on stopping and recurrence of rash with rechallenge).
- Soriano V, Dona C, Barreiro P, Gonzalez-Lahoz J. Is there cross-toxicity between nevirapine and efavirenz in subjects developing rash. AIDS. 2000;14:1672–3. [PubMed: 10983663](Retrospective review, only 1 of 8 patients with rash on nevirapine developed rash on efavirenz; no mention of hepatic cross reactions).
- Centers for Disease Control and Prevention (CDC). Serious adverse events attributed to nevirapine regimens for postexposure prophylaxis after HIV exposures–worldwide, 1997-2000. MMWR Morb Mortal Wkly Rep. 2001;49:1153–6. [PubMed: 11198946](After two reports of acute liver failure in patients receiving nevirapine for prophylaxis against HIV exposures, CDC reviewed serious adverse event reports of nevirapine prophylaxis between 1997-2000; 22 events were identified, including 12 cases of hepatotoxicity, average latency of 3 weeks, bilirubin 2.0 to 33.7 mg/dL, ALT 182 to 2790 U/L).
- Bundow D, Rosoff L, Aboulafia DM. Optimal treatment of nevirapine-associated hepatotoxicity remains uncertain. AIDS Read. 2001;11:577–80. [PubMed: 11789021](Two men, ages 39 and 33 years, developed fever, rash and eosinophilia 4 and 2 weeks after starting nevirapine [bilirubin 7.6 and 3.0 mg/dL, ALT 171 and 354 U/L, Alk P 360 and 397 U/L], resolving without corticosteroid therapy in 4-6 weeks).
- Piliero PJ, Purdy B. Nevirapine-induced hepatitis: a case series and review of the literature. AIDS Read. 2001;11:379–82. [PubMed: 11494710](2 women and 2 men with HIV infection, ages 39 to 53 years, developed liver injury 2-11 weeks after starting nevirapine therapy [peak bilirubin 3.5, 10.9, 8.6 and 21.1 mg/dL, AST 268, 505, 1450 and 160 U/L, Alk P 888, 401, 238 and 150 U/L]; one with HCV coinfection died of hepatic failure, the others recovered upon stopping).
- Prakash M, Poreddy V, Tiyyagura L, Bonacini M. Jaundice and hepatocellular damage associated with nevirapine therapy. Am J Gastroenterol. 2001;96:1571–4. [PubMed: 11374701](Four men, ages 27 to 49 years, developed rash, fever and jaundice 4-6 weeks after starting nevirapine for HIV infection [bilirubin 8.2-17.8 mg/dL, ALT 288-3493 U/L, Alk P 258-851 U/L], resolving within 5-10 weeks of stopping).
- Benn PD, Mercey DE, Brink N, Scott G, Williams IG. Prophylaxis with a nevirapine-containing triple regimen after exposure to HIV-1. Lancet. 2001;357:687–8. [PubMed: 11247556](Among 41 persons with needlestick or sexual exposure to HIV who were given nevirapine prophylaxis, 5 had ALT elevations above 5 times the ULN, all resolved, evidently none with jaundice).
- Martínez E, Blanco JL, Arnaiz JA, Pérez-Cuevas JB, Mocroft A, Cruceta A, Marcos MA, et al. Hepatotoxicity in HIV-1-infected patients receiving nevirapine-containing antiretroviral therapy. AIDS. 2001;15:1261–8. [PubMed: 11426070](Among 610 patients starting nevirapine, 10.8% developed ALT >3 times ULN and 1.1% developed symptoms [most were HCV positive as well], but all were reversible on stopping).
- Claudio GA, Martin AF, de Dios Perrino S, Velasco AA. DRESS syndrome associated with nevirapine therapy. Arch Intern Med. 2001;161:2501–2. [PubMed: 11700164](31 year old man with HIV-HCV coinfection developed rash 7 days after starting nevirapine, resolving when stopping and recurring 3 days after restarting with fever [bilirubin 12.7 mg/dL, ALT 224 U/L, Alk P 501 U/L, 30% eosinophils], resolving rapidly on stopping: Case 3).
- Núñez M, Lana R, Mendoza JL, Martín-Carbonero L, Soriano V. Risk factors for severe hepatic injury after introduction of highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2001;27:426–31. [PubMed: 11511818](Retrospective review of 222 patients started on highly active antiretroviral therapy, 125 with nonnucleoside reverse transcriptase inhibitors; 31% had ALT elevation [9% >5 times ULN], risk factors were HCV infection, alcohol use and older age; transient in all except HCV infected).
- Benhamou Y, Di Martino V, Bochet M, Colombet G, Thibault V, Liou A, Katlama C, Poynard T, Multivir C. Group. Factors affecting liver fibrosis in human immunodeficiency virus-and hepatitis C virus-coinfected patients: impact of protease inhibitor therapy. Hepatology. 2001;34:283–7. [PubMed: 11481613](Cross sectional study of 172 patients with HIV-HCV coinfection undergoing liver biopsy; those on protease inhibitors were less likely to have cirrhosis [6.3% vs 18.5%] and estimated 25 year cirrhosis rates were 9% vs 27%; other factors associated with fibrosis were excessive alcohol use, low CD4 counts and age of acquiring HCV).
- Reisler K. High hepatotoxicity rate seen among HAART patients. AIDS Alert. 2001;16:118–9. [PubMed: 11547496](News report on abstract: study of 10,011 patients in 21 clinical trials with HIV infection, showing that ALT elevations >5 times normal occur in 6.2% of highly active antiretroviral therapy treated patients; 10.8% with efavirenz, 8.9% with nevirapine and 6% with delavirdine in short term studies).
- González de Requena D, Núñez M, Jiménez-Nácher I, Soriano V. Liver toxicity caused by nevirapine. AIDS. 2002;16:290–1. [PubMed: 11807315](Case control study in 70 patients with HIV infection on nevirapine; higher plasma levels were found in those with ALT elevations [6.25 vs 5.2 µg/mL], particularly in patients with HIV-HCV co-infection).
- Bonnet F, Lawson-Ayayi S, Thiébaut R, Ramanampamonjy R, Lacoste D, Bernard N, Malvy D, et al. French Aquitaine Cohort. Groupe d'Epidémiologie Clinique du SIDA en Aquitaine (GECSA). A cohort study of nevirapine tolerance in clinical practice: French Aquitaine Cohort, 1997-1999. Clin Infect Dis. 2002;35:1231–7. [PubMed: 12410483](Retrospective study in 137 patients in routine clinical practice, 33% had side effects and 21% stopped nevirapine; 20% with rash, 1 Stevens Johnson syndrome; ALT >100 U/L in 43% of HCV or HBV coinfected and 9% without either).
- Macías J, Melguizo I, Fernández-Rivera FJ, García-García A, Mira JA, Ramos AJ, Rivera JM, Pineda JA. Mortality due to liver failure and impact on survival of hepatitis virus infections in HIV-infected patients receiving potent antiretroviral therapy. Eur J Clin Microbiol Infect Dis. 2002;21:775–81. [PubMed: 12461586](While mortality due to AIDS declined from 4.5 to 1.8/100 person years with introduction of highly active antiretroviral therapy, mortality from liver disease increased from 0.3 to 0.5/100 person years).
- De Maat MM, Mathôt RA, Veldkamp AI, Huitma AD, Mulder JW, Meenhorst PL, Van Gorp EC, Carlier H, Beijnen JH. Hepatotoxicity following nevirapine-containing regimens in HIV-1-infected individuals. Pharmacol Res. 2002;46:295–300. [PubMed: 12220974](Retrospective analysis of 174 patients receiving nevirapine based antiretroviral therapy; only 3.4% had ALT or AST elevations >5 times ULN, no correlation with plasma levels; risk factors were HBV coinfection and use of protease inhibitors).
- Clark SJ, Creighton S, Portmann B, Taylor C, Wendon JA, Cramp ME. Acute liver failure associated with antiretroviral treatment for HIV: a report of six cases. J Hepatol. 2002;36:295–301. [PubMed: 11830344](6 patients with HIV infection who developed acute liver failure on antiretroviral therapy, including stavudine [n=5], lamivudine [n=3], didanosine [n=2], saquinavir [n=2], efavirenz [n=2], nevirapine [n=2], or nelfinavir, delavirdine or zidovudine [n=1] for 1-3 months [peak bilirubin 2.7-32 mg/dL, AST 240-8650 U/L, Alk P 122-191 U/L]; 2 with signs of hypersensitivity; two with hepatitis B; 5 died, autopsies showing massive necrosis; one with massive steatosis; likely multiple causes).
- Johnson S, Chan J, Bennett CL. Hepatotoxicity after prophylaxis with a nevirapine-containing antiretroviral regimen. Ann Intern Med. 2002;137:146–7. [PubMed: 12118982](Among 174 health care workers receiving prophylaxis after accidental exposure to HIV, 8 received nevirapine containing regimens, 5 had severe hepatotoxicity, and one required liver transplantation).
- Palmon R, Koo BC, Shoultz DA, Dieterich DT. Lack of hepatotoxicity associated with nonnucleoside reverse transcriptase inhibitors. J Acquir Immune Defic Syndr. 2002;29:340–5. [PubMed: 11917237](Retrospective analysis of 272 HIV-positive patients seen in an New York City practice; ALT elevations above 5 times ULN occurred in only 1.1% regardless of type of nonnucleoside reverse transcriptase inhibitor used or presence of coinfection with HBV or HCV).
- Gökengin D, Yamazhan T. Hepatic adverse events during highly active antiretroviral therapy containing nevirapine: a case report. Ann Clin Microbiol Antimicrob. 2002;1:1. [PMC free article: PMC131012] [PubMed: 12437780](39 year old man with HIV infection developed fever and malaise one month after starting nevirapine, zidovudine and lamivudine [bilirubin 1.7 mg/dL, ALT 1558 U/L, Alk P 577 U/L], resolving within 2 weeks of stopping; lamivudine and zidovudine were restarted).
- Dodi F, Alessandrini A, Camera M, Lorenzo G, Morandi N, Pagano G. Stevens-Johnson syndrome in HIV patients treated with nevirapine: two case reports. AIDS. 2002;16:1197–8. [PubMed: 12004287](35 and 37 year old men with HIV infection developed generalized rash and oral erosions or palmar involvement 20 and 29 days after starting nevirapine, both requiring corticosteroids and having slow recovery; ALT levels were elevated in one patient who also had HCV infection).
- Dybul M, Fauci AS, Bartlett JG, Kaplan JE, Pau AK., Panel on Clinical Practices for the Treatment of HIV. Guidelines for using antiretroviral agents among HIV-infected adults and adolescents. Recommendations of the Panel on Clinical Practices for Treatment of HIV. MMWR Recomm Rep. 2002;51(RR-7):1–55. [PubMed: 12027060](Recommendations on use of antiretroviral agents for HIV infection including indications, efficacy, need for monitoring and side effects including hepatotoxicity).
- Sulkowski MS, Thomas DL, Mehta SH, Chaisson RE, Moore RD. Hepatotoxicity associated with nevirapine or efavirenz-containing antiretroviral therapy: role of hepatitis C and B infections. Hepatology. 2002;35:182–9. [PubMed: 11786975](Prospective analysis of 568 patients, ALT levels >5 times ULN occurred in 16% on nevirapine and 8% on efavirenz, only 1/3rd in first 12 weeks, usually associated with HBV or HCV coinfection [69%] or concurrent protease inhibitor use [82%]; no recurrence on switching from one to the other).
- Martín-Carbonero L, Núñez M, Ríos P, Pérez-Olmeda M, González-Lahoz J, Soriano V. Liver injury after beginning antiretroviral therapy in HIV/hepatitis C virus co-infected patients is not related to immune reconstitution. AIDS. 2002;16:1423–5. [PubMed: 12131221](Among 42 patients with HIV-HCV coinfection who were started on antiretroviral therapy, 30 [72%] developed ALT elevations which were above 5 times ULN in 6 [14%], but there was no association of these elevations with decreases in HIV RNA levels or increases in CD4 counts of HCV RNA levels).
- Pulido F, Torralba M. NNRTI hepatotoxicity: efavirenz versus nevirapine. J HIV Ther. 2002;7 Suppl 2:S3–16. [PubMed: 12735215](Review of hepatotoxicity of all antiretrovirals with focus on nonnucleoside reverse transcriptase inhibitors).
- Wit FW, Weverling GJ, Weel J, Jurriaans S, Lange JM. Incidence of and risk factors for severe hepatotoxicity associated with antiretroviral combination therapy. J Infect Dis. 2002;186:23–31. [PubMed: 12089658](Retrospective analysis found 6.3% incidence of liver enzyme elevations >5 times ULN among 560 Dutch patients on highly active antiretroviral therapy, 71% had either HBV or HCV coinfection; risk factors included recent introduction of nevirapine or high dose ritonavir or stopping lamivudine).
- Kontorinis N, Dieterich DT. Toxicity of non-nucleoside analogue reverse transcriptase inhibitors. Semin Liver Dis. 2003;23:173–82. [PubMed: 12800070](Review of hepatotoxicity of nonnucleoside reverse transcriptase inhibitors; rate of ALT elevations >5 times ULN is ~6% at 6 weeks, but thereafter is similar in nevirapine and placebo recipients raising questions regarding the causality of late elevations; ALT elevations occurred in >30% of patients on nevirapine, but lower rate of severe elevations, estimated to be 8.9% in metaanalysis of 21 studies, compared to 10.8% with efavirenz and 3.6% with delavirdine).
- Knudtson E, Para M, Boswell H, Fan-Havard P. Drug rash with eosinophilia and systemic symptoms syndrome and renal toxicity with a nevirapine-containing regimen in a pregnant patient with human immunodeficiency virus. Obstet Gynecol. 2003;101(5 Pt 2):1094–7. [PubMed: 12738113](26 year old pregnant woman with CD4 count of 614 developed rash and fever 6 weeks after starting lamivudine, zidovudine and nevirapine [9.6% eosinophilia, bilirubin 12 mg/dL, ALT 235 U/L, Alk P 257 U/L, INR 2.4], who worsened despite stopping nevirapine and receiving corticosteroids; had emergency Caesarian with subsequent recovery: Case 2).
- Wetterwald E, Le Cleach L, Michel C, David F, Revuz J. Nevirapine-induced overlap Stevens-Johnson syndrome/toxic epidermal necrolysis. Br J Dermatol. 1999;140:980–2. [PubMed: 10354056](35 and 40 year old men with HIV infection developed rash, mouth ulcers and fever 13 and 25 days after starting nevirapine with changes of both Stevens-Johnson syndrome [mucosal involvement and fever] and toxic epidermal necrolysis [skin detachment], no mention of hepatotoxicity; both recovered in 2 and 4 weeks).
- Martinez-Sierra C, Arizcorreta A, Diaz F, Roldan R, Martin-Herrera L, Perez-Guzman E, Giron-Gonzalez JA. Progression of chronic hepatitis C to liver fibrosis and cirrhosis in patients coinfected with hepatitis C virus and human immunodeficiency virus. Clin Infect Dis. 2003;36:491–8. [PubMed: 12567308](Comparison of 41 patients with HIV-HCV coinfection and 147 with HCV infection alone for clinical features; higher HCV RNA levels and more advanced fibrosis were found in HIV infected).
- Mohsen AH, Easterbrook PJ, Taylor C, Portmann B, Kulaegaram R, Murah S, Wiselka M, et al. Impact of human immunodeficiency virus(HIV) infection on the progression of liver fibrosis in hepatitis C virus infected patients. Gut. 2003;52:1035–40. [PMC free article: PMC1773713] [PubMed: 12801963](Estimated rate of fibrosis progression in cross sectional study of 153 HCV-infected and 55 HCV-HIV coinfected patients undergoing liver biopsy; HIV was associated with more rapid progression as was older age and higher ALT levels).
- Núñez M, González-Requena D, González-Lahoz J, Soriano V. Short communication: interactions between nevirapine plasma levels, chronic hepatitis C, and the development of liver toxicity in HIV-infected patients. AIDS Res Hum Retroviruses. 2003;19:187–8. [PubMed: 12689410](Case controlled study of 70 patients treated with nevirapine for HIV infection; nevirapine plasma levels were the same in HIV-HCV co-infected as in HIV-mono-infected patients: 5.8 vs 6.1 µg/mL: see Gonzalez de Requena 2002).
- Qurishi N, Kreuzberg C, Luchters G, Effenberger W, Kupfer B, Sauerbruch T, Rockstroh JK, et al. Effect of antiretroviral therapy on liver-related mortality in patients with HIV hepatitis C virus coinfection. Lancet. 2003;362:1708–13. [PubMed: 14643119](In a cohort of 285 patients with HIV infection, both overall and liver related mortality decreased [1.70 to 0.70 to 0.45 per 100 person years] with introduction of nucleoside analogues and then highly active antiretroviral therapy; 18 cases of severe hepatotoxicity [14% of treated], but none were fatal).
- Tural C, Fuster D, Tor J, Ojanguren I, Sirera G, Ballesteros A, Lasanta JAJ, et al. Time on antiretroviral therapy is a protective factor for liver fibrosis in HIV and hepatitis C virus(HCV) co-infected patients. J Viral Hepat. 2003;10:118–25. [PubMed: 12614468](Cross sectional analysis of 126 patients with HIV-HCV coinfection undergoing liver biopsy identified time on antiretroviral therapy as predictive of lesser degrees of fibrosis).
- de Maat MM, ter Heine R, van Gorp EC, Mulder JW, Mairuhu AT, Beijnen JH. Case series of acute hepatitis in a non-selected group of HIV-infected patients on nevirapine-containing antiretroviral treatment. AIDS. 2003;17:2209–14. [PubMed: 14523278](Among 306 patients starting a nevirapine-containing regimen for HIV infection, 8 developed acute hepatitis [2.6%] after 8-31 days [bilirubin 0.5-5.8 mg/mL, ALT 150-596 U/L, Alk P 67-789 U/L], all resolving within 2-7 weeks of stopping).
- Dore G. Antiretroviral therapy-related hepatotoxicity: predictors and clinical management. J HIV Ther. 2003;8:96–100. [PubMed: 14671507](Review with suggested algorithm for management of ALT elevations on antiretroviral therapy).
- Weissbrich B, Langmann P, Schubert J, Jassoy C, Klinker H. Resolution of HCV infection in a HIV-infected patient under HAART after several hepatitis flare-ups. Eur J Med Res. 2003;8:495–8. [PubMed: 14644704](43 year old man with HIV and severe hepatitis C became HIV and HCV RNA negative after complications of cirrhosis and while on long term nevirapine and indinavir therapy).
- Law WP, Dore GJ, Duncombe CJ, Mahanontharit A, Boyd MA, Ruxrungtham K, Lange JM, et al. Risk of severe hepatotoxicity associated with antiretroviral therapy in the HIV-NAT Cohort, Thailand, 1996-2001. AIDS. 2003;17:2191–9. [PubMed: 14523276](Among 692 patients in 8 controlled trials in Thailand, rate of ALT elevations above 5 times ULN was 6.1/100 patient years overall; in multivariate analysis, risk factors were HBV [Relative risk=3.9], HCV [3.0], and use of nonnucleoside reverse transcriptase inhibitors [6.8], rate with nevirapine [18.6/100 person years] higher than efavirenz [2.4/100 person years]).
- Ena J, Amador C, Benito C, Fenoll V, Pasquau F. Risk and determinants of developing severe liver toxicity during therapy with nevirapine-and efavirenz-containing regimens in HIV-infected patients. Int J STD AIDS. 2003;14:776–81. [PubMed: 14624743](Retrospective review of 136 patients treated with regimens including nonnucleoside reverse transcriptase inhibitors, 48% had ALT elevations which were >5 times ULN in 20%; risk factors were alcohol use, HCV infection and 4 drug regimens; 3 of 17 patients with ALT elevations on nevirapine redeveloped ALT elevations on restarting; 2 patient had jaundice, but had HCV coinfection and were exposed to other hepatotoxins).
- Martín-Carbonero L, Núñez M, González-Lahoz J, Soriano V. Incidence of liver injury after beginning antiretroviral therapy with efavirenz or nevirapine. HIV Clin Trials. 2003;4:115–20.(Retrospective analysis of risk factors for liver toxicity in 162 patients on nevirapine [12%] and 136 on efavirenz [4%], average onset at 5 months, risk factors were nevirapine [relative risk=3.1], HCV coinfection [4.7], alcohol abuse [4.5] and female gender [2.3]).
- Jackson JB, Barnett S, Piwowar-Manning E, Apuzzo L, Raines C, Hendrix C, Hamzeh F, et al. A phase I/II study of nevirapine for pre-exposure prophylaxis of HIV-1 transmission in uninfected subjects at high risk. AIDS. 2003;17:547–53. [PubMed: 12598775](Trial comparing weekly, twice weekly vs every other day nevirapine for 4 weeks in 33 subjects acutely exposed to HIV infection, 3 developed ALT elevations above 5 times ULN, but no clinically apparent jaundice).
- Ofotokun I, Pomeroy C. Sex differences in adverse reactions to antiretroviral drugs. Top HIV Med. 2003;11:55–9. [PubMed: 12717043](Review of sex differences in adverse events; higher frequency of mitochondrial toxicity and hypersensitivity in women than men).
- Ogedegbe AO, Sulkowski MS. Antiretroviral-associated liver injury. Clin Liver Dis. 2003;7:475–99. [PubMed: 12879995](Review of hepatotoxicity of antiretrovirals; ALT elevations above 5 times ULN reported in 7% with zidovudine, 16% didanosine, 9-13% stavudine, <1% lamivudine, tenofovir and abacavir, 3-10% protease inhibitors, 10% nevirapine and 8% efavirenz; recommended monitoring at 4 weeks and then every 12 weeks, monitoring more closely if ALT levels are elevated and stopping if ALT levels are >10 times ULN or if symptoms of liver injury are present).
- Martín-Carbonero L, Benhamou Y, Puoti M, Berenguer J, Mallolas J, Quereda C, Arizcorreta A, et al. Incidence and predictors of severe liver fibrosis in human immunodeficiency virus-infected patients with chronic hepatitis C: a European collaborative study. Clin Infect Dis. 2004;38:128–33. [PubMed: 14679458](Analysis from 10 European centers of fibrosis on liver biopsies from 914 HIV-HCV coinfected patients; 13% had cirrhosis; predictors of severe fibrosis were older age [Odds Ratio=2.95], excessive alcohol use [1.6], and low CD4 counts [1.4], but not use of antiretroviral therapy).
- Stern JO, Robinson PA, Love J, Lanes S, Imperiale MS, Mayers DL. A comprehensive hepatic safety analysis of nevirapine in different populations of HIV infected patients. J Acquir Immune Defic Syndr. 2003;34 Suppl 1:S21–33. [PubMed: 14562855](Analysis of data from 17 randomized controlled trials of nevirapine done between 1991 and 2001, ALT >5 times ULN in 10%, 2/3rds were asymptomatic; risk factors were elevated baseline ALT levels, HBV or HCV coinfection, and higher baseline CD4 counts; 4 of 2545 patients died of liver failure in noncomparative trials and 3 among 5302 patients in cohort studies ~1/1000).
- Baylor MS, Johann-Liang R. Hepatotoxicity associated with nevirapine use. J Acquir Immune Defic Syndr. 2004;35:538–9. [PubMed: 15021321](Letter in response to Stern et al. from members of the FDA whose analyses identified 285 patients [11%] with hepatic adverse events due to nevirapine; rash associated events in 2.7%, symptomatic hepatitis in 2.7%; associated with higher pretreatment CD4 counts).
- Negredo E, Moltó J, Muñoz-Moreno JA, Pedrol E, Ribera E, Viciana P, Galindos MJ, et al. Safety and efficacy of once-daily didanosine, tenofovir and nevirapine as a simplification antiretroviral approach. Antivir Ther. 2004;9:335–42. [PubMed: 15259896](Controlled trial of switching to once daily highly active antiretroviral regimen that included nevirapine in 169 patients, adverse events requiring discontinuation higher with daily regimen [14% vs 4%], including 5 cases of hepatotoxicity not otherwise characterized).
- Dieterich DT, Robinson PA, Love J, Stern JO. Drug-induced liver injury associated with the use of nonnucleoside reverse-transcriptase inhibitors. Clin Infect Dis. 2004;38 Suppl 2:S80–9. [PubMed: 14986279](Extensive review of hepatotoxicity of nonnucleoside reverse transcriptase inhibitors; in 17 controlled trials of nevirapine, 10% of patients developed ALT or AST elevations >5 times ULN and 5% had symptomatic hepatic event, 2.2% with rash).
- Manfredi R, Calza L, Chiodo F. Efavirenz versus nevirapine in current clinical practice: a prospective, open-label observational study. J Acquir Immune Defic Syndr. 2004;35:492–502. [PubMed: 15021314](Comparison of 287 patients on efavirenz vs 258 on nevirapine in practice situation; similar efficacy against HIV but higher rate of ALT abnormalities with nevirapine [52% vs 18%] and discontinuation because of liver toxicity [3.5% vs 0%]).
- Becker S. Liver toxicity in epidemiological cohorts. Clin Infect Dis. 2004;38 Suppl 2:S49–55. [PubMed: 14986275](Analysis of four large cohort studies of 5133 patients found hepatotoxicity rates similar with all antiretrovirals; major risk factor being coinfection with HBV or HCV. Nevirapine and ritonavir were associated with increased risk of hepatotoxicity in first 12 weeks).
- Patel SM, Johnson S, Belknap SM, Chan J, Sha BE, Bennett C. Serious adverse cutaneous and hepatic toxicities associated with nevirapine use by non-HIV-infected individuals. J Acquir Immune Defic Syndr. 2004;35:120–5. [PubMed: 14722442](Analysis of MedWatch system and published results found 12 instances of severe rash [3 Stevens-Johnson syndrome] in non-HIV infected persons receiving nevirapine as prophylaxis against acute HIV exposure, arising after 7-12 days, 6 with fever; 30 instances of liver injury, after average of 20 days, one fulminant).
- Rey D, Partisani M, Hess-Kempf G, Krantz V, Priester M, Cheneau C, Bernard-Henry C, et al. Tolerance of a short course of nevirapine, associated with 2 nucleoside analogues, in postexposure prophylaxis of HIV. J Acquir Immune Defic Syndr. 2004;37:1454–6. [PubMed: 15602122](Results of using nevirapine for 4 days and two nucleoside analogues for 1 month as prophylaxis against possible HIV exposure in 120 patients: 2.8% had transient ALT elevations, but no clinically apparent liver injury and no transmission).
- Pujari SN, Patel AK, Naik E, Patel KK, Dravid A, Patel JK, Mane AA, et al. Effectiveness of generic fixed-dose combinations of highly active antiretroviral therapy for treatment of HIV infection in India. J Acquir Immune Defic Syndr. 2004;37:1566–9. [PubMed: 15577409](Analysis of 1291 patients started on nevirapine based combination regimens in India; rash in 6.6% and hepatitis in 3.2%, but no deaths from liver injury except 4 with lactic acidosis on stavudine).
- Meraviglia P, Schiavini M, Castagna A, Viganò P, Bini T, Landonio S, Danise A, et al. Lopinavir/ritonavir treatment in HIV antiretroviral-experienced patients: evaluation of risk factors for liver enzyme elevation. HIV Med. 2004;5:334–43. [PubMed: 15369508](Among 782 patients on lopinavir/ritonavir for mean of one year, 9.1% had serum enzyme elevations largely in HBV or HCV coinfected patients [16% vs 3% without coinfection]; no association with nevirapine use; 13 stopped therapy because of liver toxicity).
- Hitti J, Frenkel LM, Stek AM, Nachman SA, Baker D, Gonzalez-Garcia A, Provisor A, et al. PACTG 1022 Study Team. Maternal toxicity with continuous nevirapine in pregnancy: results from PACTG 1022. J Acquir Immune Defic Syndr. 2004;36:772–6. [PubMed: 15213559](Controlled trial of nelfinavir vs nevirapine combined with lamivudine and zidovudine in HIV-positive pregnant women; 5 women stopped nevirapine, 1 for Stevens-Johnson syndrome and 4 for hepatotoxicity including one death from hepatic failure; 1 stopped nelfinavir for clinical hepatitis).
- Almond LM, Boffito M, Hoggard PG, Bonora S, Raiteri R, Reynolds HE, Garazzino S, et al. The relationship between nevirapine plasma concentrations and abnormal liver function tests. AIDS Res Hum Retroviruses. 2004;20:716–22. [PubMed: 15307917](Among 85 patients on a nevirapine based regimen, there was no association between ALT elevations and plasma nevirapine levels; slightly higher levels were present in HBV and HCV coinfected than HIV monoinfected patients).
- Claes P, Wintzen M, Allard S, Simons P, De Coninck A, Lacor P. Nevirapine-induced toxic epidermal necrolysis and toxic hepatitis treated successfully with a combination of intravenous immunoglobulins and N-acetylcysteine. Eur J Intern Med. 2004;15:255–8. [PubMed: 15288682](39 year old man developed oral ulcers within 2 weeks of starting nevirapine, progressing to Stevens-Johnson syndrome and severe hepatitis, with rapid improvement after IVIG and N-acetylcysteine therapy; few details provided).
- Dailly E, Billaud E, Reliquet V, Breurec S, Perré P, Léautez S, Jolliet P, et al. No relationship between high nevirapine plasma concentration and hepatotoxicity in HIV-1-infected patients naive of antiretroviral treatment or switched from protease inhibitors. Eur J Clin Pharmacol. 2004;60:343–8. [PubMed: 15156302](Among 77 patients with HIV infection starting nevirapine, elevated plasma levels did not correlate with serum AST elevations).
- Macías J, Castellano V, Merchante N, Palacios RB, Mira JA, Sáez C, García-García JA, et al. Effect of antiretroviral drugs on liver fibrosis in HIV-infected patients with chronic hepatitis C: harmful impact of nevirapine. AIDS. 2004;18:767–74. [PubMed: 15075511](Cross sectional analysis of factors associated with hepatic fibrosis among 152 of 559 patients with HIV-HCV coinfection undergoing liver biopsy; advanced fibrosis was more common with higher age of infection, use of protease inhibitors and nevirapine based therapy).
- Rodríguez Guardado A, Maradona Hidalgo JA, Asensi Alvarez V, Cartón Sánchez JA. Med Clin (Barc). 2004;122:317. [Assessment of nevirapine liver toxicity in patients with HIV and HVC coinfection] [PubMed: 15030745](Retrospective analysis of 57 patients treated with nevirapine [and two nucleosides]; ALT elevations >100 U/L or twice baseline in 68% of 31 HCV-infected and 8% of 26 noninfected patients; no significant change in HCV RNA levels on therapy).
- Te HS. Cholestasis in HIV-infected patients. Clin Liver Dis. 2004;8:213–28. viii-ix. [PubMed: 15062202](Review of causes of cholestasis in HIV-infected patients including antiretrovirals).
- de Maat MM, Beijnen JH, Schellens JH, Mulder JW. Chronic hepatotoxicity after long-term antiretroviral treatment including nevirapine. J Infect. 2005;50:262–4. [PubMed: 15780424](Case report of patient without HBV or HCV infection on nevirapine with mild ALT elevations that appeared to correlate with nevirapine levels and decreased with dose modification).
- Sanne I, Mommeja-Marin H, Hinkle J, Bartlett JA, Lederman MM, Maartens G, Wakeford C, et al. Severe hepatotoxicity associated with nevirapine use in HIV-infected subjects. J Infect Dis. 2005;191:825–9. [PubMed: 15717255](In a prospective study, ALT elevations >5 times normal occurred in 17% [66/385] of nevirapine vs 0% [0/83] of efavirenz treated patients, usually in first 12 weeks, most had symptoms including rash, nausea and jaundice; two cases of acute liver failure and death on nevirapine).
- Pineda JA, Macías J. Progression of liver fibrosis in patients coinfected with hepatitis C virus and human immunodeficiency virus undergoing antiretroviral therapy. J Antimicrob Chemother. 2005;55:417–9. [PubMed: 15731202](Review of evidence that HAART therapy has an effect on progression of fibrosis in chronic hepatitis C).
- Aranzabal L, Casado JL, Moya J, Quereda C, Diz S, Moreno A, Moreno L, et al. Influence of liver fibrosis on highly active antiretroviral therapy-associated hepatotoxicity in patients with HIV and hepatitis C virus coinfection. Clin Infect Dis. 2005;40:588–93. [PubMed: 15712082](Among 107 patients with HIV-HCV coinfection and pretreatment liver biopsy; ALT elevations of >5 times ULN [or 3.5 times baseline] occurred in 38% with advanced fibrosis and 15% without. Higher rates of ALT elevations with nevirapine and efavirenz [13%] found only in those with advanced fibrosis).
- Martin AM, Nolan D, James I, Cameron P, Keller J, Moore C, Phillips E, et al. Predisposition to nevirapine hypersensitivity associated with HLA-DRB1*0101 and abrogated by low CD4 T-cell counts. AIDS. 2005;19:97–9. [PubMed: 15627041](Among 235 patients on nevirapine, 26 [11%] developed rash, fever or liver abnormalities within 6 weeks; HLA-DRB1*0101 positivity was present in 17% with rash vs 4% without, with significant interactions with CD4 counts).
- Joy S, Poi M, Hughes L, Brady MT, Koletar SL, Para MF, Fan-Havard P. Third-trimester maternal toxicity with nevirapine use in pregnancy. Obstet Gynecol. 2005;106(5 Pt 1):1032–8. [PubMed: 16260522](Among 23 pregnant women with HIV given nevirapine, 3 [13%] developed liver injury, 2 with rash, eosinophilia and ALT elevations, one with asymptomatic ALT elevation [ALT 235, 295 and 241 U/L]; all 3 had baseline CD4 counts of >250/µL).
- Rotger M, Colombo S, Furrer H, Bleiber G, Buclin T, Lee BL, Keiser O, et al. Swiss HIV Cohort Study. Influence of CYP2B6 polymorphism on plasma and intracellular concentrations and toxicity of efavirenz and nevirapine in HIV-infected patients. Pharmacogenet Genomics. 2005;15:1–5. [PubMed: 15864119](Analysis of polymorphisms of CYP 2B6, the major hepatic enzyme responsible for efavirenz and nevirapine metabolism; G516T was associated with higher drug levels for both agents and higher tissue levels correlated with greater neuropsychiatric side effects).
- Abrescia N, D’Abbraccio M, Figoni M, Busto A, Maddaloni A, De Marco M. Hepatotoxicity of antiretroviral drugs. Curr Pharm Des. 2005;11:3697–710. [PubMed: 16305505](Review of hepatotoxicity of antiretrovirals; major syndrome with nonnucleoside reverse transcriptase inhibitors is hypersensitivity).
- Núñez M, Soriano V. Hepatotoxicity of antiretrovirals: incidence, mechanisms and management. Drug Saf. 2005;28:53–66. [PubMed: 15649105](Review of liver toxicity of antiretrovirals).
- Fields KS, Petersen MJ, Chiao E, Tristani-Firouzi P. Case reports: treatment of nevirapine-associated dress syndrome with intravenous immune globulin(IVIG). J Drugs Dermatol. 2005;4:510–3. [PubMed: 16004028](Onset of rash, fever, oral ulcers and adenopathy after 4 weeks of nevirapine therapy with jaundice [bilirubin 9.8 mg/dL, ALT 362 U/L, Alk P 283 U/L, eosinophils 12%], recovery in 6 weeks perhaps with help of intravenous immune globulin infusions).
- Kappelhoff BS, van Leth F, Robinson PA, MacGregor TR, Baraldi E, Montella F, Uip DE, et al. 2NN Study Group. Are adverse events of nevirapine and efavirenz related to plasma concentrations? Antivir Ther. 2005;10:489–98. [PubMed: 16038474](Among 1077 HIV positive patients started on treatment, no association was found between adverse events and plasma levels or pharmacokinetics of nevirapine or efavirenz).
- Torti C, Lapadula G, Casari S, Puoti M, Nelson M, Quiros-Roldan E, Bella D, et al. EPOKA-MASTER Study Group. Incidence and risk factors for liver enzyme elevation during highly active antiretroviral therapy in HIV-HCV co-infected patients: results from the Italian EPOKA-MASTER Cohort. BMC Infect Dis. 2005;5:58. [PMC free article: PMC1188059] [PubMed: 16018804](Among 1038 HIV-HCV coinfected patients starting antiretroviral therapy, the risk of ALT elevations above 5 times ULN was 17.1/100 patient years in treatment-naïve and 8.2 in treatment-experienced group; risk factors being higher baseline ALT levels and use of nonnucleoside reverse transcriptase inhibitors).
- Zhou J, Phanupak P, Kiertiburanakul S, Ditangco R, Kamarulzaman A, Pujary S. TREAT Asia HIV Observational Database. Highly active antiretroviral treatment containing efavirenz or nevirapine and related toxicity in the TREAT Asia HIV Observational Database. J Acquir Immune Defic Syndr. 2006;43:501–3. [PMC free article: PMC10545477] [PubMed: 17099317](Analysis of 735 HIV-positive patients starting efavirenz and 813 starting nevirapine containing regimens; 12 patients in both groups developed ALT levels >5 times ULN, but monitoring was irregular; no deaths from liver disease occurred and no racial differences in rates of ALT elevations were found; HCV coinfection was a risk factor).
- Buyse S, Vibert E, Sebagh M, Antonini T, Ichai P, Castaing D, Samuel D, et al. Liver transplantation for fulminant hepatitis related to nevirapine therapy. Liver Transpl. 2006;12:1880–2. [PubMed: 17133571](38 year old woman with HIV infection developed acute liver failure 6 weeks after starting nevirapine, zidovudine and lamivudine [bilirubin 11.2 mg/dL, ALT 12578 U/L, GGT 340 U/L], undergoing liver transplantation and later tolerating efavirenz without recurrence: Case 1).
- Haas DW, Bartlett JA, Andersen JW, Sanne I, Wilkinson GR, Hinkle J, Rousseau F, et al. Adult AIDS Clinical Trials Group. Pharmacogenetics of nevirapine-associated hepatotoxicity: an Adult AIDS Clinical Trials Group collaboration. Clin Infect Dis. 2006;43:783–6. [PubMed: 16912957](A polymorphism of the MDR gene [p-glycoprotein] was associated with lower rate of hepatotoxicity attributed to nevirapine in a controlled trial conducted in South Africa: 10.6% of cases vs 19.4% of controls had MDR1 3435C→T, believed to have an effect on the transporter function of MDR1; no linkage to CYP polymorphisms found).
- Ritchie MD, Haas DW, Motsinger AA, Donahue JP, Erdem H, Raffanti S, Rebeiro P, et al. Drug transporter and metabolizing enzyme gene variants and nonnucleoside reverse-transcriptase inhibitor hepatotoxicity. Clin Infect Dis. 2006;43:779–82. [PubMed: 16912956](Case control study of 9 nevirapine and 4 efavirenz recipients who developed ALT >5 times ULN on therapy vs 49 controls; found weak association with MDR1 [p-glycoprotein: ABCB1] polymorphism).
- Maniar JK, Shah SR, Verma R, Kamath R, Gupte P, Maniar A. Nevirapine-induced fulminant hepatitis. J Assoc Physicians India. 2006;54:957–8. [PubMed: 17334017](38 year old man with HIV infection developed abdominal pain and nausea 3 weeks after starting nevirapine, zidovudine and lamivudine [bilirubin 1.4 mg/dL, ALT 1421 U/L, Alk P not given, INR 2.6], with rapid deterioration and death in 3 days).
- Lyons F, Hopkins S, Kelleher B, McGeary A, Sheehan G, Geoghegan J, Bergin C, et al. Maternal hepatotoxicity with nevirapine as part of combination antiretroviral therapy in pregnancy. HIV Med. 2006;7:255–60. [PubMed: 16630038](Retrospective analysis of 123 women given antiretroviral regimen including nevirapine [usually with zidovudine and lamivudine] during pregnancy; one-third had ALT elevations, 8 developed ALT or AST levels >5 times ULN and 2 had fever, rash and hepatitis at 4 and 8 weeks subsequently dying of hepatic failure; risk factors appeared to be higher CD4 counts and black race).
- Björnsson E, Olsson R. Suspected drug-induced liver fatalities reported to the WHO database. Dig Liver Dis. 2006;38:33–8. [PubMed: 16054882](In WHO database of fatal adverse drug reactions from 1968-2003, 4690 reports of drug induced liver fatality; nevirapine was the 9th most common cause [~60 cases]).
- Drummond NS, Vilar FJ, Naisbitt DJ, Hanson A, Woods A, Park BK, Pirmohamed M. Drug-specific T cells in an HIV-positive patient with nevirapine-induced hepatitis. Antivir Ther. 2006;11:393–5. [PubMed: 16759058](30 year old man with HIV infection developed nausea and jaundice without rash 4 weeks after starting nevirapine [bilirubin levels unclear, ALT ~950 U/L, Alk P ~610 U/L], resolving within 6 weeks of stopping; positive lymphocyte stimulation, but unable to clone specific T cells).
- Maida I, Núñez M, Ríos MJ, Martín-Carbonero L, Sotgiu G, Toro C, Rivas P, et al. Severe liver disease associated with prolonged exposure to antiretroviral drugs. J Acquir Immune Defic Syndr. 2006;42:177–82. [PubMed: 16688096](Survey of 3200 HIV-positive patients in Spain identified 17 [0.5%] with cryptogenic chronic liver disease, 83% male, ages 27-57 years, mostly gay men with long term infection; minimal ALT, GGT, and Alk P elevations; biopsy in 5 showed nonspecific changes, elastography often abnormal; didanosine implicated in case controlled analysis, multifactorial, but some cases may have represented nodular regeneration rather than cirrhosis).
- Lyons F, Hopkins S, Kelleher B, McGeary A, Sheehan G, Geoghegan J, Bergin C, et al. Maternal hepatotoxicity with nevirapine as part of combination antiretroviral therapy in pregnancy. HIV Med. 2006;7:255–60. [PubMed: 16630038](Retrospective analysis of 123 pregnant women in Dublin treated with nevirapine; 8 developed hepatotoxicity with ALT >5 times ULN; two died of fulminant hepatitis [onset after 4 and 5 weeks of nevirapine, lamivudine and zidovudine with rash followed by jaundice; bilirubin 12.5 and 5.9 mg/dL, AST 2850 and 1276 U/L], rapidly progressing to coma and death; lesser ALT elevations occurred in another 25% of patients).
- João EC, Calvet GA, Menezes JA, D'Ippolito MM, Cruz ML, Salgado LA, Matos HJ. Nevirapine toxicity in a cohort of HIV-1-infected pregnant women. Am J Obstet Gynecol. 2006;194:199–202. [PubMed: 16389032](Retrospective study of 197 pregnant women in Brazil given nevirapine; enzyme elevations occurred in 5.6%, but only one case of serious liver toxicity, marked by rash and cholestatic hepatitis at 7 weeks).
- Servoss JC, Kitch DW, Andersen JW, Reisler RB, Chung RT, Robbins GK. Predictors of antiretroviral-related hepatotoxicity in the adult AIDS Clinical Trial Group (1989-1999). J Acquir Immune Defic Syndr. 2006;43:320–3. [PubMed: 16967041](Analysis of factors that predict “serious hepatotoxicity” in 9% of cohort of 8851 patients with HIV infection enrolled in trials of antiretroviral therapy; factors identified included elevated baseline liver tests, HCV coinfection, and in subgroups, didanosine, nevirapine and stavudine use).
- Hofman P, Nelson AM. The pathology induced by highly active antiretroviral therapy against human immunodeficiency virus: an update. Curr Med Chem. 2006;13:3121–32. [PubMed: 17168701](Review of pathology of adverse effects of antiretroviral agents with examples of hepatic mitochondrial liver injury and cholestasis).
- Núñez M. Hepatotoxicity of antiretrovirals: incidence, mechanisms and management. J Hepatol. 2006;44(1) Suppl:S132–9. [PubMed: 16364487](Review of hepatotoxicity of antiretrovirals; elevations in ALT or AST above 5 times ULN occurs in 2-18% of HIV-positive patients starting therapy, more frequent with HCV or HBV coinfection; combination of protease inhibitors with low dose ritonavir does not seem to increase risk; agents with highest risk are nevirapine and the nonnucleoside reverse transcriptase inhibitors).
- Kondo W, Carraro EA, Prandel E, Dias JM, Perini J, Macedo RL, Cornelsen TC, et al. Nevirapine-induced side effects in pregnant women: experience of a Brazilian university hospital. Braz J Infect Dis. 2007;11:544–8. [PubMed: 18327464](Among 133 women starting antiretroviral therapy during pregnancy, 21 [16%] developed rash and 6 [5%] ALT elevations usually within the first 7 weeks; all had CD4 counts >250/µL before therapy, none developed jaundice or Stevens-Johnson syndrome).
- Forna F, Liechty CA, Solberg P, Asiimwe F, Were W, Mermin J, Behumbiize P, et al. Clinical toxicity of highly active antiretroviral therapy in a home-based AIDS care program in rural Uganda. J Acquir Immune Defic Syndr. 2007;44:456–62. [PubMed: 17279048](Among 1029 adults started on nevirapine with lamivudine and stavudine, 58 [~6%] developed rash and 5 [~.5%] developed acute hepatitis, 3 with rash; 1 death due to hypersensitivity syndrome and hepatitis arising 4 weeks after starting triple therapy with nevirapine).
- Hall DB, Macgregor TR. Case-control exploration of relationships between early rash or liver toxicity and plasma concentrations of nevirapine and primary metabolites. HIV Clin Trials. 2007;8:391–9. [PubMed: 18042504](Case controlled study of plasma nevirapine and metabolite levels in 49 patients with a hypersensitivity reaction and 49 controls; no significant differences, indicating the idiosyncratic nature of this response).
- Mehta U, Maartens G. Is it safe to switch between efavirenz and nevirapine in the event of toxicity? Lancet Infect Dis. 2007;7:733–8. [PubMed: 17961859](Review; some evidence of cross sensitivity between nevirapine and efavirenz to skin rash, but none to hepatotoxicity; total of 11 patients reported in literature to have switched and none had recurrence of liver injury).
- Phillips E, Gutiérrez S, Jahnke N, Yip B, Lima VD, Hogg RS, Harrigan PR, et al. Determinants of nevirapine hypersensitivity and its effect on the association between hepatitis C status and mortality in antiretroviral drug-naïve HIV-positive patients. AIDS. 2007;21:1561–8. [PubMed: 17630551](Database analysis of nevirapine “hypersensitivity reaction” which occurred in 9.6% of patients and was associated with poor prognosis; no predictive factors of the reaction and unclear whether definition accurately captured all hypersensitivity reactions).
- Manfredi R, Calza L. Safety issues about nevirapine administration in HIV-infected pregnant women. J Acquir Immune Defic Syndr. 2007;45:365–8. [PubMed: 17592340](Experience in managing 31 pregnant women on nevirapine, none developing clinically apparent hepatotoxicity or ALT elevations above 5 times ULN).
- Natarajan U, Pym A, McDonald C, Velisetty P, Edwards SG, Hay P, Welch J, et al. Safety of nevirapine in pregnancy. HIV Med. 2007;8:64–9. [PubMed: 17305934](Retrospective study of 235 pregnant women with HIV infection in UK treated with nevirapine containing regimens; 6% developed rash and 3.4% hepatotoxicity within 6 weeks [ALT 161-807 U/L], all recovered).
- Rivero A, Mira JA, Pineda JA. Liver toxicity induced by non-nucleoside reverse transcriptase inhibitors. J Antimicrob Chemother. 2007;59:342–6. [PubMed: 17255142](Review of liver toxicity of nevirapine and efavirenz; ALT elevations reported in 1-8% of efavirenz compared to 4-16% of nevirapine recipients).
- Maggiolo F, Arici C, Airoldi M, Ripamonti D, Quinzan G, Gregis G, Ravasio V, et al. Reasons for discontinuation of nevirapine-containing HAART: results from an unselected population of a large clinical cohort. J Antimicrob Chemother. 2007;59:569–72. [PubMed: 17255141](Experience in use of nevirapine in 582 patients; among 286 discontinuations, hepatotoxicity was cause in only 29 [4%]; ALT elevations >5 ULN occurred in 10.2% [5.3/100 patient years]).
- Jamisse L, Balkus J, Hitti J, Gloyd S, Manuel R, Osman N, Djedje M, et al. Antiretroviral-associated toxicity among HIV-1-seropositive pregnant women in Mozambique receiving nevirapine-based regimens. J Acquir Immune Defic Syndr. 2007;44:371–6. [PubMed: 17259905](Among 146 pregnant women given triple therapy with nevirapine, 11 [8%] had ALT elevations >2.5 times ULN and 4 [2.7%] above 5 times ULN [261-690 U/L] 4-10 weeks after starting, all recovered upon stopping).
- Hahn JA, Maier M, Byakika-Tusiime J, Oyugi JH, Bangsberg DR. Hepatotoxicity during nevirapine-based fixed-dose combination antiretroviral therapy in Kampala, Uganda. J Int Assoc Physicians AIDS Care (Chic). 2007;6:83–6. [PubMed: 17537997](Prospective study of 97 patients starting nevirapine-based antiretroviral therapy in Uganda followed for 1-20 months; ALT elevations occurred in 22% and were >5 times ULN in 2.2%, one dying of acute liver failure at week 12 [4 weeks after onset]).
- Medrano J, Barreiro P, Tuma P, Vispo E, Labarga P, Blanco F, Soriano V. Risk for immune-mediated liver reactions by nevirapine revisited. AIDS Rev. 2008;10:110–5. [PubMed: 18615121](Review of hepatotoxicity of nevirapine; some of the risk factors identified may not apply to antiretroviral experienced patients).
- Tansuphaswadikul S, Aung SE, Phonrat B, Kaewkungwal J, Pitisuttithum P, Maek-a-nantawat W. Predisposing factors for nevirapine toxicity among AIDS patients with low baseline CD4 count. Asian Pac J Allergy Immunol. 2007;25:147–54. [PubMed: 18035802](Among 206 patients with HIV infection starting regimen with nevirapine, 8 developed hepatotoxicity [4%: 3.6 per person years], higher among patients on antituberculosis drugs).
- Phanuphak N, Apornpong T, Teeratakulpisarn S, Chaithongwongwatthana S, Taweepolcharoen C, Mangclaviraj S, Limpongsanurak S, et al. Nevirapine-associated toxicity in HIV-infected Thai men and women, including pregnant women. HIV Med. 2007;8:357–66. [PubMed: 17661843](409 patients [244 pregnant women] given triple therapy with nevirapine 64 [15.6%] developed hepatotoxicity, 5-fold higher rates in pregnant than nonpregnant women).
- Bourlière M, Duclos-Vallée JC, Pol S. Gastroenterol Clin Biol. 2007;31:895–905. [Liver and antiretrovirals: hepatotoxicity, steatosis and monitoring of patients with liver disease] French. [PubMed: 18166875](Review of hepatotoxicity of antiretrovirals discussing patterns of toxic idiosyncrasy, hypersensitivity [nevirapine and abacavir], mitochondrial toxicity [zalcitabine, didanosine, stavudine and zidovudine], steatohepatitis [protease inhibitors with lipodystrophy], immune restoration [in patients with HIV-HBV or -HCV coinfection]; recommendations for management focusing on prevention and monitoring).
- Jain MK. Drug-induced liver injury associated with HIV medications. Clin Liver Dis. 2007;11:615–39. vii-viii. [PubMed: 17723923](Review of hepatotoxicity of antiretroviral medications; ALT elevations occur in 2-18% of patients, but often resolve spontaneously even without dose modification; classes of injury include hypersensitivity [nevirapine, efavirenz, abacavir], mitochondrial injury [stavudine, didanosine, zidovudine], flares of hepatitis B [lamivudine, emtricitabine, tenofovir], flares of hepatitis C [any potent regimen], idiosyncratic injury [ritonavir, nevirapine, efavirenz], and cholestatic hepatitis [many agents]).
- Esser S, Helbig D, Hillen U, Dissemond J, Grabbe S. Side effects of HIV therapy. J Dtsch Dermatol Ges. 2007;5:745–54. [PubMed: 17760894](Review of side effects of antiretroviral agents focusing on immune reconstitution syndrome, lipodystrophy, cutaneous skin reactions, hypersensitivity reactions [abacavir, nevirapine], hyperbilirubinemia [indinavir, atazanavir], local reactions [enfuvirtide] and hyperpigmentation [zidovudine, emtricitabine]).
- Labarga P, Soriano V, Vispo ME, Pinilla J, Martin-Carbonero L, Castellares C, Casado R, et al. Hepatotoxicity of antiretroviral drugs is reduced after successful treatment of chronic hepatitis C in HIV-infected patients. J Infect Dis. 2007;196:670–6. [PubMed: 17674307](Retrospective analysis of 132 HIV/HCV coinfected patients who were treated with interferon based therapy of whom 33% had sustained virological response; subsequent ALT elevations were less common in responders [3.1%/year] than nonresponders [12.9%/year]; events also associated with exposure to nevirapine and dideoxynucleosides).
- Mussi-Pinhata MM, Rego MA, Freimanis L, Kakehasi FM, Machado DM, Cardoso EM, Read JS., NISDI Perinatal Protocol Study Group. Maternal antiretrovirals and hepatic enzyme, hematologic abnormalities among human immunodeficiency virus type 1-uninfected infants: the NISDI perinatal study. Pediatr Infect Dis J. 2007;26:1032–7. [PubMed: 17984811](Analysis of serum enzyme elevations in newborns of HIV infected mothers on various antiretroviral regimens; infants whose mothers received protease inhibitors were more likely to have ALT elevations [odds ratio 1.9] similarly for nonnucleoside reverse transcriptase inhibitors [odds ratio 2.4], most elevations were mild and self-limited).
- Torti C, Costarelli S, De Silvestri A, Quiros-Roldan E, Lapadula G, Cologni G, Paraninfo G, et al. BHCC Study Group. Analysis of severe hepatic events associated with nevirapine-containing regimens: CD4+ T-cell count and gender in hepatitis C seropositive and seronegative patients. Drug Saf. 2007;30:1161–9. [PubMed: 18035868](Among 905 patients treated with nevirapine containing regimens, ALT elevations above 5 times ULN occurred in 7%; rates were 3 fold higher among those with HCV coinfection; among HCV negative patients, higher CD4 T cell counts and gender were risk factors for increased risk of ALT elevations).
- Bae WH, Wester C, Smeaton LM, Shapiro RL, Lockman S, Onyait K, Thior I, et al. Hematologic and hepatic toxicities associated with antenatal and postnatal exposure to maternal highly active antiretroviral therapy among infants. AIDS. 2008;22:1633–40. [PMC free article: PMC2664540] [PubMed: 18670224](Prospective monitoring found that only 1 of 69 infants born to antiretroviral-treated mothers and none of 109 infants born to drug therapy unexposed mothers with HIV infection developed ALT elevations > 5 times ULN during the first 7 months of life).
- Black V, Rees H. Incidence of nevirapine-associated hepatitis in an antenatal clinic. S Afr Med J. 2008;98:116–8. [PubMed: 18350206](Experience in treating 329 pregnant HIV-positive women with nevirapine, lamivudine and zidovudine; 31 developed ALT elevations, but most were mild and only 3 patients had hepatitis [0.8%], all after 5 weeks and recovering with stopping).
- Knobel H, Guelar A, Montero M, Carmona A, Luque S, Berenguer N, González A. Risk of side effects associated with the use of nevirapine in treatment-naïve patients, with respect to gender and CD4 cell count. HIV Med. 2008;9:14–8. [PubMed: 18199168](Retrospective analysis of 142 patients at single center who started triple therapy with nevirapine for HIV infection; neither skin rash [11.2%] nor ALT elevations [5.6%] were more common with higher CD4 T cell counts at baseline).
- Wit FW, Kesselring AM, Gras L, Richter C, van der Ende ME, Brinkman K, Lange JM, et al. Discontinuation of nevirapine because of hypersensitivity reactions in patients with prior treatment experience, compared with treatment-naive patients: the ATHENA cohort study. Clin Infect Dis. 2008;46:933–40. [PubMed: 18271750](Among 3752 patients in Netherlands receiving nevirapine based combination therapy for HIV infection, 6.2% developed the hypersensitivity syndrome; occurrence correlated with female gender and high pretreatment CD4 counts).
- Dart Trial Team. Twenty-four-week safety and tolerability of nevirapine vs. abacavir in combination with zidovudine/lamivudine as first-line antiretroviral therapy: a randomized double-blind trial(NORA). Trop Med Int Health. 2008;13:6–16. [PMC free article: PMC2635484] [PubMed: 18290996](Controlled trial in 600 Ugandan patients with CD4 counts <200 given nevirapine or abacavir [with zidovudine and lamivudine] for 24 weeks; 4.6% vs 2.3% developed hypersensitivity reaction, 7 nevirapine- but no abacavir-treated patients had ALT levels >10 times ULN, all within 8 weeks of starting).
- De Lazzari E, León A, Arnaiz JA, Martinez E, Knobel H, Negredo E, Clotet B, et al. Hepatotoxicity of nevirapine in virologically suppressed patients according to gender and CD4 cell counts. HIV Med. 2008;9:221–6. [PubMed: 18366445](Metaanalysis of 4 controlled trials of nevirapine in 410 experienced patients, hepatotoxicity developed in 2% with low and 4% with high initial CD4 counts; but difference was not significant).
- Antunes AM, Duarte MP, Santos PP, da Costa GG, Heinze TM, Beland FA, Marques MM. Synthesis and characterization of DNA adducts from the HIV reverse transcriptase inhibitor nevirapine. Chem Res Toxicol. 2008;21:1443–56. [PubMed: 18597499](Nevirapine is oxidized by P450 CYP 3A4 and 2B6 and products are conjugated to glucuronides and excreted in the urine; but other pathways are possible that might yield electrophilic intermediates that can bind to DNA; in this report several nevirapine-DNA adducts were characterized).
- Medrano J, Barreiro P, Tuma P, Vispo E, Labarga P, Blanco F, Soriano V. Risk for immune-mediated liver reactions by nevirapine revisited. AIDS Rev. 2008;10:110–5. [PubMed: 18615121](Review; symptomatic hepatic events occur in ~5% of patients taking nevirapine, early hypersensitivity reactions occurring especially in women with CD4 counts >250 and those with HBV or HCV coinfection; late onset hepatotoxicity may be a class effect [also occurring with efavirenz]).
- Inductivo-Yu I, Bonacini M. Highly active antiretroviral therapy-induced liver injury. Current Drug Safety. 2008;3:4–13. [PubMed: 18690975](Review of drug induced liver injury due to antiretroviral agents; severe liver injury due to nevirapine is rare but up to 10% of patients develop ALT elevations above 5 times normal).
- Sterling RK, Chiu S, Snider K, Nixon D. The prevalence and risk factors for abnormal liver enzymes in HIV-positive patients without hepatitis B or C coinfections. Dig Dis Sci. 2008;53:1375–82. [PMC free article: PMC3836444] [PubMed: 17939038](Retrospective analysis of data on 1208 patients with HIV infection on antiretroviral therapy; mild-to-moderate ALT elevations found in 15% of HIV-mono-infected and 63% of HCV-HIV coinfected; factors associated with ALT elevations were hypertension, higher HIV RNA levels, lower CD4 counts, metabolic syndrome and absence of protease inhibitor use).
- Manosuthi W, Sungkanuparph S, Tansuphaswadikul S, Chottanapund S, Mankatitham W, Chimsuntorn S, Sittibusaya C, et al. Incidence and risk factors of nevirapine-associated severe hepatitis among HIV-infected patients with CD4 cell counts less than 250 cells/microL. J Med Assoc Thai. 2008;91:159–65. [PubMed: 18389979](Among 910 patients starting on antiretroviral therapy with nevirapine with low CD4 counts, 10 [1.2/100 patient years] developed “clinical hepatitis”, major risk factor being elevations in AST at baseline).
- Sathia L, Obiorah I, Taylor G, Kon O, O'Donoghue M, Gibbins S, Walsh J, et al. Concomitant use of nonnucleoside analogue reverse transcriptase inhibitors and rifampicin in TB/HIV type 1-coinfected patients. AIDS Res Hum Retroviruses. 2008;24:897–901. [PubMed: 18671475](Among 103 HIV positive patients with tuberculosis receiving rifampin, including 17 on nevirapine and 26 efavirenz, transient elevations in ALT occurred in 17%, but only 2 patients stopped therapy for ALT elevations >5 times ULN, and both safely restarted antituberculosis therapy after ALT abnormalities resolved).
- van Schalkwyk JE, Alimenti A, Khoo D, Maan E, Forbes JC, Burdge DR, Gilgoff S, et al. Serious toxicity associated with continuous nevirapine-based HAART in pregnancy. BJOG. 2008;115:1297–302. [PubMed: 18715416](Analysis of 103 HIV-positive pregnant women, toxicities requiring discontinuation occurred in 6 of 56 women on nevirapine [3 rash and 3 hepatotoxicity] vs only 1 of 47 treated with other agents [kidney stones: indinavir]).
- Brück S, Witte S, Brust J, Schuster D, Mosthaf F, Procaccianti M, Rump JA, et al. Hepatotoxicity in patients prescribed efavirenz or nevirapine. Eur J Med Res. 2008;13:343–8. [PubMed: 18700192](Among 151 patients starting efavirenz and 145 nevirapine, rates of ALT elevations were similar in the two groups; 6% vs 3.4% had ALT levels >2.5 times ULN and 1.2% vs 2.1% had ALT >5 times ULN; only predictive factor identified was presence of HBsAg; no fatal cases).
- Chen J, Mannargudi BM, Xu L, Uetrecht J. Demonstration of the metabolic pathway responsible for nevirapine-induced skin rash. Chem Res Toxicol. 2008;21:1862–70. [PubMed: 18729332](Rat model of skin rash induced by nevirapine; sex and strain dependent, onset after several weeks and more rapid with rechallenge even at lower dose; correlation between plasma levels and frequency of rash by strain and species; thus dose related and apparently due to 12-hydroxylation pathway possibly a quinone methide reactive metabolite).
- Kumarasamy N, Venkatesh KK, Cecelia AJ, Devaleenal B, Lai AR, Saghayam S, Balakrishnan P, Yepthomi T, Poongulali S, Flanigan TP, Solomon S, Mayer KH. Spectrum of adverse events after generic HAART in southern Indian HIV-infected patients. AIDS Patient Care STDS. 2008;22:337–44. [PubMed: 18422462](Among 3154 patients with HIV infection treated with antiretroviral agents over a 4 year period at a single center in Southern India, hepatitis occurred in 3.5%, usually within the first 3 months; lactic acidosis was more common in women and was associated with stavudine use).
- Vitezica ZG, Milpied B, Lonjou C, Borot N, Ledger TN, Fefebvre A, Hovnanian A. HLA-DRB*01 associated with cutaneous hypersensitivity induced by nevirapine and efavirenz. AIDS. 2008;22:540–1. [PubMed: 18301070](Among 21 patients with HIV infection treated with nevirapine [n=14] or efavirenz [n=7], 6 developed a hypersensitivity rash, 5 of whom had DRB1*01 compared to 1 [7%] control).
- Hammer SM, Eron JJ Jr, Reiss P, Schooley RT, Thompson MA, Walmsley S, Cahn P, et al. International AIDS Society-USA. Antiretroviral treatment of adult HIV infection: 2008 recommendations of the International AIDS Society-USA panel. JAMA. 2008;300:555–70. [PubMed: 18677028](Updated recommendations on use of antiviral therapy in adults with HIV infection, including use of recently approved agents raltegravir, maraviroc and etravirine).
- Soriano V, Puoti M, Garcia-Gascó P, Rockstroh JK, Benhamou Y, Barreiro P, McGovern B. Antiretroviral drugs and liver injury. AIDS. 2008;22:1–13. [PubMed: 18090386](Review of hepatotoxicity of antiretroviral drugs with recommendations on management, stopping therapy if symptoms arise, with overt jaundice [direct bilirubin], evidence of mitochondrial toxicity, ALT >10 times ULN, ALT at lower levels if newly marketed agent; important to rule out other causes: problematic agents include didanosine, stavudine and zidovudine; nevirapine and efavirenz, full dose ritonavir and tipranavir).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, 7 were attributed to antiretroviral agents, 2 nevirapine, 1 efavirenz and 4 miscellaneous combinations).
- Van Dyke RB, Wang L, Williams PL. Pediatric AIDS Clinical Trials Group 219C Team. Toxicities associated with dual nucleoside reverse-transcriptase inhibitor regimens in HIV-infected children. J Infect Dis. 2008;198:1599–608. [PMC free article: PMC2737265] [PubMed: 19000014](Among 2233 children receiving two nucleoside reverse transcriptase inhibitors, 0.6-1.6% developed hepatitis, 8.3-13.5% acidosis; overall ALT elevations were rare [<1%]).
- Ingiliz P, Benhamou Y. Elevated liver enzymes in HIV monoinfected patients on HIV therapy: what are the implications? J HIV Ther. 2009;14:3–7. [PubMed: 19731558](Review of the causes of serum enzyme elevations during antiretroviral therapy; nonnucleoside reverse transcriptase inhibitors are capable of causing a hypersensitivity reaction with liver injury arising during the first 6 weeks of therapy as well as an immunologically mediated injury that arises 6-12 months after starting treatment).
- Moodie EEM, Pai NP, Klein MB. Is antiretroviral therapy causing long-term liver damage? A comparative analysis of HIV-mono-infected and HIV/Hepatitis C co-infected cohorts. PLOS-ONE. 2009;4:e4517. [PMC free article: PMC2637977] [PubMed: 19223976](Analysis of ratio of AST to platelet ratio [APRI] in cohort of HIV infected patients with [n=127] or without [n=533] HCV-coinfection; APRI values were higher in patients with HCV infection and the percentage yearly increase was greater in patients on antiretroviral therapy [3.31% for protease inhibitors, 2.18% with nonnucleoside reverse transcriptase inhibitors]. Absolute values, the role of AST vs platelet count and rates for patients not on therapy were not provided).
- Ferrajolo C, Capuano A, Verhamme KM, Schuemie M, Rossi F, Stricker BH, Sturkenboom MC. Drug-induced hepatic injury in children: a case/non-case study of suspected adverse drug reactions in VigiBase. Br J Clin Pharmacol. 2010;70:721–8. [PMC free article: PMC2997312] [PubMed: 21039766](Worldwide pharmacovigilance database contained 9036 hepatic adverse drug reactions in children, 3 antiretroviral agents were among the top 40 cases, including zidovudine [8th, 106 cases], lamivudine [26th, 45 cases] and nevirapine [36th, 37 cases]).
- Colafigli M, Di Giambenedetto S, Bracciale L, Fanti I, Prosperi M, Cauda R, De Luca A. Long-term follow-up of nevirapine-treated patients in a single-centre cohort. HIV Med. 2009;10:461–9. [PubMed: 19459991](Among 573 patients with HIV infection treated with nevirapine based regimens at a single Italian center, 1.9% developed ALT elevations >5 times ULN and 2.4% discontinued for liver toxicity in first year; no cases of acute liver failure).
- McKoy JM, Bennett CL, Scheetz MH, Differding V, Chandler KL, Scarsi KK, Yarnold PR, et al. Hepatotoxicity associated with long- versus short-course HIV-prophylactic nevirapine use: a systematic review and meta-analysis from the Research on Adverse Drug events And Reports (RADAR) project. Drug Saf. 2009;32:147–58. [PMC free article: PMC2768573] [PubMed: 19236121](Metaanalysis of rates of ALT elevation >5 times ULN during short [<5 days] vs longer courses of nevirapine for prophylaxis found lower rates after acute exposures [0% vs 13%] and in mothers [0.2% vs 4.4%] and their newborns [0.8% vs 1.1%]; review of MedWatch revealed 3 severe cases in non-HIV infected and 5 deaths in pregnant women attributed to nevirapine).
- Ouyang DW, Shapiro DE, Lu M, Brogly SB, French AL, Leighty RM, Thompson B, et al. Increased risk of hepatotoxicity in HIV-infected pregnant women receiving antiretroviral therapy independent of nevirapine exposure. AIDS. 2009 Nov 27;23:2425–30. [PMC free article: PMC2783653] [PubMed: 19617813](Among 1229 pregnant and 821 nonpregnant women with HIV infection on antiretroviral therapy, ALT elevations >5 times ULN occurred in 1.2% of pregnant vs 0.6% of nonpregnant and 0.8% of nevirapine vs 1.0% of non-nevirapine taking women).
- Ouyang DW, Brogly SB, Lu M, Shapiro DE, Hershow RC, French AL, Leighty RM, et al. Lack of increased hepatotoxicity in HIV-infected pregnant women receiving nevirapine compared with other antiretrovirals. AIDS. 2010;24:109–14. [PMC free article: PMC3388940] [PubMed: 19926957](Among 1229 pregnant women with HIV infection treated with antiretroviral therapy during pregnancy, ALT elevations >5 times ULN occurred in 0.5% on nevirapine based vs 1.4% of 1011 on non-nevirapine based regimens; no maternal deaths from liver disease).
- Peters PJ, Stringer J, McConnell MS, Kiarie J, Ratanasuwan W, Intalapaporn P, Potter D, et al. Nevirapine-associated hepatotoxicity was not predicted by CD4 count ≥250 cells/μL among women in Zambia, Thailand and Kenya. HIV Med. 2010;11:650–60. [PubMed: 20659176](Among 820 women with HIV infection started on nevirapine based regimens in 3 African countries between 2005-7, 41 [5%] developed ALT elevations >5 times ULN, 27 [3%] had rash and ALT elevations, and 3 [0.4%] died of acute liver failure; no correlation with CD4 counts, age or BMI).
- Jao J, Sturdevant M, del Rio Martin J, Schiano T, Fiel MI, Huprikar S. Nevirapine-induced Stevens Johnson-syndrome and fulminant hepatic failure requiring liver transplantation. Am J Transplant. 2010;10:1713–6. [PubMed: 20642694](57 year old woman with HIV infection developed rash within 3 weeks and Stevens-Johnson syndrome with jaundice within 5 weeks of switching from tenofovir to nevirapine [peak bilirubin 24 mg/dL, ALT 2150 U/L, Alk P 285 U/L, INR 2.8], progressing to hepatic failure as rash improved, requiring liver transplantation).
- Coffie PA, Tonwe-Gold B, Tanon AK, Amani-Bosse C, Bédikou G, Abrams EJ, Dabis F, Ekouevi DK. Incidence and risk factors of severe adverse events with nevirapine-based antiretroviral therapy in HIV-infected women. MTCT-Plus program, Abidjan, Côte d'Ivoire. BMC Infect Dis. 2010;10:188. [PMC free article: PMC2904297] [PubMed: 20576111](Among 290 African women starting nevirapine based regimen for HIV infection, 3.4% developed ALT elevations >5 times ULN, but without relationship to initial CD4 counts).
- Antela A, Ocampo A, Gómez R, López MJ, Mariño A, Losada E, Rodríguez R, et al. Galician HIV Study Group. Liver toxicity after switching or simplifying to nevirapine-based therapy is not related to CD4 cell counts: results of the TOSCANA study. HIV Clin Trials. 2010;11:11–7. [PubMed: 20400407](Among 221 patients with HIV infection on antiretroviral therapy who were switched to nevirapine, 6.6% developed ALT elevations >5 times ULN; no correlation with initial CD4 count or gender, but higher rate in those with HCV coinfection [12.9%]).
- Chu KM, Boulle AM, Ford N, Goemaere E, Asselman V, Van Cutsem G. Nevirapine-associated early hepatotoxicity: incidence, risk factors, and associated mortality in a primary care ART programme in South Africa. PLoS One. 2010;5:e9183. [PMC free article: PMC2822855] [PubMed: 20174653](Among 1809 patients with HIV infection starting nevirapine based regimens, 26 [1.4%] developed ALT elevations >5 times ULN within 3 months, half symptomatic, none fatal, most resolving after switch to efavirenz; no association found with initial CD4 counts).
- Moses M, Zachariah R, Tayler-Smith K, Misinde D, Foncha C, Manzi M, Bauerfeind A, et al. Outcomes and safety of concomitant nevirapine and rifampicin treatment under programme conditions in Malawi. Int J Tuberc Lung Dis. 2010;14:197–202. [PubMed: 20074411](Among 156 African patients with HIV infection and tuberculosis starting treatment with stavudine, lamivudine and nevirapine and given isoniazid, rifampin and pyrazinamide for tuberculosis, ALT elevations >5 times ULN developed in only one patient and none had clinically apparent liver injury).
- Ciccacci C, Borgiani P, Ceffa S, Sirianni E, Marazzi MC, Altan AM, Paturzo G, et al. Nevirapine-induced hepatotoxicity and pharmacogenetics: a retrospective study in a population from Mozambique. Pharmacogenomics. 2010;11:23–31. [PubMed: 20017669](Case controlled analysis of ABC B1 and CYP single nucleotide polymorphisms [SNPs] in 78 African patients with nevirapine hepatotoxicity and 78 without; found an ABC B1 SNP associated with hepatotoxicity [p=0.04] and several CYP 2B6 SNPs associated with ALT [but not AST] elevations).
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury and 4 to antiretroviral agents, including 3 to combinations with stavudine and 1 to abacavir).
- Li ZC, Li HJ, Dai LL, Gao YQ, Cai WP, Li HY, Huang XJ, et al. Liver injury in HIV-1-infected patients receiving non-nucleosides reverse transcriptase inhibitors-based antiretroviral therapy. Chin Med J (Engl). 2010;123:3587–90. [PubMed: 22166636](Among 75 Chinese patients on antiretroviral therapy with nevirapine or efavirenz, 45 developed abnormal liver tests, most of which were transient and mild, and risk factors included HBV or HCV coinfection, use of nevirapine and exposure to other hepatotoxic agents).
- Dejesus E, Mills A, Bhatti L, Conner C, Storfer S. A randomised comparison of safety and efficacy of nevirapine vs. atazanavir/ritonavir combined with tenofovir/ emtricitabine in treatment-naïve patients. Int J Clin Pract. 2011;65:1240–9. [PubMed: 21999631](Among 152 patients with HIV infection treated with nevirapine vs atazanavir/ritonavir, 1 patient in each group discontinued therapy for liver injury [enzyme elevations and jaundice).
- Mankhatitham W, Lueangniyomkul A, Manosuthi W. Hepatotoxicity in patients co-infected with tuberculosis and HIV-1 while receiving non-nucleoside reverse transcriptase inhibitor-based antiretroviral therapy and rifampicin-containing anti-tuberculosis regimen. Southeast Asian J Trop Med Public Health. 2011;42:651–8. [PubMed: 21706943](Among 134 patients with HIV infection and tuberculosis treated with rifampin, ALT elevations >5 times ULN occurred in 3 patients on nevirapine [4.6%] and 1 [1.4%] on efavirenz).
- Molleston JP, Fontana RJ, Lopez MJ, Kleiner DE, Gu J, Chalasani N. Drug-induced Liver Injury Network. Characteristics of idiosyncratic drug-induced liver injury in children: results from the DILIN prospective study. J Pediatr Gastroenterol Nutr. 2011;53:182–9. [PMC free article: PMC3634369] [PubMed: 21788760](Among 30 children with suspected drug induced liver injury, none were attributed to an antiretroviral agent).
- Wang J, Kou H, Fu Q, Han Y, Qiu Z, Zuo L, Li Y, et al. Nevirapine plasma concentrations are associated with virologic response and hepatotoxicity in Chinese patients with HIV infection. PLoS One. 2011;6:e26739. [PMC free article: PMC3204986] [PubMed: 22066007](Analysis of nevirapine plasma levels in 227 patients found a weak correlation of higher levels with grade 3 hepatotoxicity, but only in males).
- Anwikar SR, Bandekar MS, Smrati B, Pazare AP, Tatke PA, Kshirsagar NA. HAART induced adverse drug reactions: a retrospective analysis at a tertiary referral health care center in India. Int J Risk Saf Med. 2011;23:163–9. [PubMed: 22020396](Among 1844 patients treated for HIV infection at a single Indian health center, 12% reported at least one adverse event).
- Htun WL, Bowonwatanuwong C, Phonrat B, Pitisuttithum P. Long term outcomes of nevirapine containing antiretroviral therapy at a center in Thailand. Southeast Asian J Trop Med Public Health. 2012;43:860–70. [PubMed: 23077808](Among 285 patients treated with nevirapine for HIV infection at a single center in Thailand, 10 [4%] had elevated liver enzymes before and only 5 [2%] after 5 years of treatment).
- Chu KM, Manzi M, Zuniga I, Biot M, Ford NP, Rasschaert F, Zachariah R. Nevirapine- and efavirenz-associated hepatotoxicity under programmatic conditions in Kenya and Mozambique. Int J STD AIDS. 2012;23:403–7. [PubMed: 22807533](Among 5832 African patients starting nevirapine or efavirenz based antiretroviral therapy for HIV infection, 124 [(2.4%] developed ALT or AST elevations >5 times ULN, mostly within the first 6 months; mortality rates were the same in patients with [5.7%] and without [5.2%] liver enzyme abnormalities).
- Macías J, Neukam K, Mallolas J, López-Cortés LF, Cartón JA, Domingo P, Moreno S, et al. COINS Study Team. Liver toxicity of initial antiretroviral drug regimens including two nucleoside analogs plus one non-nucleoside analog or one ritonavir-boosted protease inhibitor in HIV/HCV-coinfected patients. HIV Clin Trials. 2012;13:61–9. [PubMed: 22510353](Among 745 Spanish patients with HIV infection started on antiretroviral therapy [with 0.8-3 years of follow up], hepatotoxicity requiring discontinuation occurred in 13% on nevirapine, 4% on efavirenz, and 6% on protease inhibitors).
- Lopez-Delgado JC, Mendiluce RM, Pinol TS, Fernández XP, Sanchez L, Vicente RG. Urgent liver transplantation for nevirapine-induced acute liver failure: report of a case and review of the literature. Ann Transplant. 2012;17:122–7. [PubMed: 22466918](40 year old woman with HIV infection on long term antiretroviral therapy developed fever and jaundice 4 weeks after addition of nevirapine [bilirubin 5.0 mg/dL, ALT 5200 U/L, GGT 258 U/L, INR 4.5], progressing to hepatic failure and liver transplant).
- Van Welzen B, Mudrikova T, Arends J, Hoepelman A. No increased risk of hepatotoxicity in long-term use of nonnucleoside reverse transcriptase inhibitors in HIV-infected patients. HIV Med. 2012;13:448–52. [PubMed: 22413955](Rates of hepatotoxicity were similar in patients on nevirapine or efavirenz based [14.8%] as on protease inhibitor based [18.5%] antiretroviral regimens, abnormalities occurring mostly during the first year and the major risk factor being HCV coinfection).
- Dong BJ, Zheng Y, Hughes MD, Frymoyer A, Verotta D, Lizak P, Sawe F, Currier JS, Lockman S, Aweeka FT., AIDS Clinical Trials Group Study 5208 Team. Nevirapine pharmacokinetics and risk of rash and hepatitis among HIV-infected sub-Saharan African women. AIDS. 2012;26:833–41. [PMC free article: PMC3506024] [PubMed: 22301417](Among 359 women started on a nevirapine based antiretroviral regimen, 54% developed rash and 23% ALT elevations [.5 times ULN in 3%]; rash but not ALT elevations could be related to drug levels; risk factors included higher CD4 counts).
- Snijdewind IJ, Smit C, Godfried MH, Nellen JF, de Wolf F, Boer K, van der Ende ME. HCV coinfection, an important risk factor for hepatotoxicity in pregnant women starting antiretroviral therapy. J Infect. 2012;64:409–16. [PubMed: 22227465](Among 425 pregnant and 1120 nonpregnant women starting antiretroviral therapy, 77 [5%] developed ALT or AST elevations >5 times ULN; risk factors being HCV coinfection [OR 5.5] and nevirapine [OR 2.0], but not pregnancy).
- Liptrott NJ, Pushpakom S, Wyen C, Fätkenheuer G, Hoffmann C, Mauss S, Knechten H, et al. German Competence Network for HIV/AIDS. Association of ABCC10 polymorphisms with nevirapine plasma concentrations in the German Competence Network for HIV/AIDS. Pharmacogenet Genomics. 2012;22:10–9. [PMC free article: PMC3605700] [PubMed: 22082652](Study of intracellular accumulation of nevirapine in cell culture focusing on the role of the ABC C10 transporter suggesting that variation in drug levels may be related to genetic variations in this transporter).
- Wongkitisophon P, Chanprapaph K. attanakaemakorn P, Vachiramon V. Six-year retrospective review of drug reaction with eosinophilia and systemic symptoms. Acta Derm Venereol. 2012;92:200–5. [PubMed: 22002792](Among 27 patients with DRESS syndrome seen between 2005 and 2010 at a single tertiary referral center in Thailand, 26 [96%] had liver involvement and 9 [33%] were jaundiced; 4 [15%] were attributed to nevirapine, 10 [37%] phenytoin, 4 [15%] sulfonamides, and 3 [11%] allopurinol).
- Carr DF, Chaponda M, Jorgensen AL, Castro EC, van Oosterhout JJ, Khoo SH, Lalloo DG, et al. Association of human leukocyte antigen alleles and nevirapine hypersensitivity in a Malawian HIV-infected population. Clin Infect Dis. 2013;56:1330–9. [PMC free article: PMC3616517] [PubMed: 23362284](Among 117 HIV-infected Malawian adults with nevirapine hypersensitivity, HLA typing identified HLA-C*04:01 as a risk factor for Stevens-Johnson syndrome and toxic epidermal necrolysis).
- Oppenheimer AP, Koh C, McLaughlin M, Williamson JC, Norton TD, Laudadio J, Heller T, et al. Vanishing bile duct syndrome in human immunodeficiency virus infected adults: a report of two cases. World J Gastroenterol. 2013;19:115–21. [PMC free article: PMC3542762] [PubMed: 23326172](Description of 2 patients with HIV infection and fatal vanishing bile duct syndrome, in neither of which the cause could be established).
- Vispo E, Fernández-Montero JV, Labarga P, Barreiro P, Soriano V. Low risk of liver toxicity using the most recently approved antiretroviral agents but still increased in HIV-hepatitis C virus coinfected patients. AIDS. 2013;27:1187–8. [PubMed: 23739226](Serum enzyme elevations occurred in 9% of 1982 patients with HIV infection started on antiretroviral therapy, including 17% of those with HCV coinfection and 6% of those without; highest rates occurred in those on nevirapine [23% with HCV, 8% without]).
- Phillips E, Bartlett JA, Sanne I, Lederman MM, Hinkle J, Rousseau F, Dunn D, et al. Associations between HLA-DRB1*0102, HLA-B*5801, and hepatotoxicity during initiation of nevirapine-containing regimens in South Africa. J Acquir Immune Defic Syndr. 2013;62:e55–7. [PMC free article: PMC3551216] [PubMed: 23328091](Among 385 patients with HIV infection receiving nevirapine, 66 [17%] developed liver enzyme elevations, usually within first 12 weekly; HLA testing showed a link with B*58:01 [23.5 vs 8.8%] and DRB1*01:02 [15.7% vs 3.9%]).
- Zhang C, Wang W, Zhou M, Han Y, Xie J, Qiu Z, Guo F, et al. The interaction of CD4 T-cell count and nevirapine hepatotoxicity in China: a change in national treatment guidelines may be warranted. J Acquir Immune Defic Syndr. 2013;62:540–5. [PubMed: 23288032](Among 566 patients with HIV infection who were started on antiretroviral therapy, 36% developed ALT elevations which were >5 times ULN in 7.7%, which were more common among those with higher CD4 cell counts).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, none of which were due to nevirapine or other antiretroviral agents).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America: an analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Among 176 reports of drug induced liver injury from Latin America published between 1996 and 2012, 3 were attributed to antiviral agents including 1 to nevirapine).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 12 [1.3%] were attributed to antiretroviral agents including 2 to nevirapine).
- Cornejo Castro EM, Carr DF, Jorgensen AL, Alfirevic A, Pirmohamed M. HLA-allelotype associations with nevirapine-induced hypersensitivity reactions and hepatotoxicity: a systematic review of the literature and meta-analysis. Pharmacogenet Genomics. 2015;25:186–98. [PubMed: 25714001](Systematic review of studies of HLA associations with nevirapine hepatotoxicity including HLA-B*58:01 and DRB1*01 in different populations).
- Hiransuthikul A, Rattananupong T, Klaewsongkram J, Rerknimitr P, Pongprutthipan M, Ruxrungtham K. Drug-induced hypersensitivity syndrome/drug reaction with eosinophilia and systemic symptoms (DIHS/DRESS): 11 years retrospective study in Thailand. Allergol Int. 2016;65:432–8. [PubMed: 27134114](Among 52 patients with DRESS syndrome presenting at a Thai medical center between 2004 and 2004, the most common causes were phenytoin [23%], nevirapine [17%], allopurinol [15%], and amoxicillin-clavulanate [14%] with liver involvement in 95%, fever 80%, lymphadenopathy 50%, and eosinophilia 60%).
- Brandariz D, Smithson A, Anton-Vazquez V. Drug reaction with eosinophilia and systemic symptoms related to antiretroviral treatment in human immunodeficiency virus patients. Indian J Sex Transm Dis AIDS. 2017;38:163–70. [PMC free article: PMC6085929] [PubMed: 30148271](Systematic review of literature on DRESS syndrome in HIV positive patients published between 1998 and 2017 identified 35 cases due to 5 agents: nevirapine 12, abacavir 10, efavirenz 6, raltegravir 6 and tenofovir 1; with fever in 83%, rash 83%, lymphadenopathy 34%, leukocytosis 26%, atypical lymphs 9%, eosinophilia 51%, liver involvement 80%, but no deaths).
- Wu PY, Cheng CY, Liu CE, Lee YC, Yang CJ, Tsai MS, Cheng SH, et al. Multicenter study of skin rashes and hepatotoxicity in antiretroviral-naïve HIV-positive patients receiving non-nucleoside reverse-transcriptase inhibitor plus nucleoside reverse-transcriptase inhibitors in Taiwan. PLoS One. 2017;12:e0171596. [PMC free article: PMC5319792] [PubMed: 28222098](Among 2341 Taiwanese HIV-positive patients initiating combination therapy including a non-nucleoside reverse transcriptase inhibitor between 2012 and 2015, ALT elevations above 3 times ULN developed within 4 weeks in 5.2% on nevirapine, 2.2% on efavirenz and 0.6% of rilpivirine).
- Devarbhavi H, Raj S. Drug-induced liver injury with skin reactions: drugs and host risk factors, clinical phenotypes and prognosis. Liver Int. 2019;39:802–11. [PubMed: 30515930](Review of adverse drug reactions with both skin and liver injury, typically with DRESS, the major causes of which are anticonvulsants [phenytoin, carbamazepine, lamotrigine], antibiotics [sulfonamides], allopurinol, and nevirapine; often with HLA associations but differing by agent, organ involvement, and often race).
- Giacomelli A, Riva A, Falvella FS, Oreni ML, Cattaneo D, Cheli S, Renisi G, et al. Clinical and genetic factors associated with increased risk of severe liver toxicity in a monocentric cohort of HIV positive patients receiving nevirapine-based antiretroviral therapy. BMC Infect Dis. 2018;18:556. [PMC free article: PMC6233541] [PubMed: 30419834](Among 362 patients receiving nevirapine for HIV infection, 8 [2.2%] developed severe hepatotoxicity, risk factors being HCV or HBV coinfection [n=7], female sex [n=6], slightly higher CD4 counts, and baseline ALT levels [median = 82 vs 27 U/L]).
- Delicio AM, Lajos GJ, Amaral E, Lopes F, Cavichiolli F, Myioshi I, Milanez H. Adverse effects of antiretroviral therapy in pregnant women infected with HIV in Brazil from 2000 to 2015: a cohort study. BMC Infect Dis. 2018;18:485. [PMC free article: PMC6161436] [PubMed: 30261855](Among 793 pregnancies in women with HIV infection on antiretroviral therapy, maternal adverse effects included dyslipidemia in 92%, anemia in 56% and liver test abnormalities in 56% including hyperbilirubinemia in 12%, most of the reactions being “mild” and no deaths; highest rates in women on non-nucleoside reverse transcriptase inhibitors such as nevirapine).
- Tadesse BT, Foster BA, Kabeta A, Ayalew F. Hepatic and renal toxicity and associated factors among HIV-infected children on antiretroviral therapy: a prospective cohort study. HIV Med. 2019;20:147–56. H/Meskel G, Jerene D, Makonnen E, et al. [PubMed: 30474906](Among 705 HIV-infected Ethiopian children followed on combination antiretroviral therapy, 12% had ALT elevations at baseline but mean levels decreased over time).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Delavirdine.[LiverTox: Clinical and Researc...]Review Delavirdine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Drug-induced liver injury associated with the use of nonnucleoside reverse-transcriptase inhibitors.[Clin Infect Dis. 2004]Drug-induced liver injury associated with the use of nonnucleoside reverse-transcriptase inhibitors.Dieterich DT, Robinson PA, Love J, Stern JO. Clin Infect Dis. 2004 Mar 1; 38 Suppl 2:S80-9.
- Review Etravirine.[LiverTox: Clinical and Researc...]Review Etravirine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Successful bosentan and nonnucleoside reverse transcriptase inhibitor-based therapy in a patient with acquired immunodeficiency syndrome and pulmonary arterial hypertension.[Pharmacotherapy. 2010]Successful bosentan and nonnucleoside reverse transcriptase inhibitor-based therapy in a patient with acquired immunodeficiency syndrome and pulmonary arterial hypertension.Hardy H, Backman ES, Farber HW. Pharmacotherapy. 2010 Apr; 30(4):139e-44e.
- Review Rilpivirine.[LiverTox: Clinical and Researc...]Review Rilpivirine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Nevirapine - LiverToxNevirapine - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...