NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Floxuridine (FUDR) is a pyrimidine analogue used as an antineoplastic agent, usually as a continuous hepatic arterial infusion to treat hepatic metastases from colon cancer. Intraarterial floxuridine is associated with a very high rate of serum enzyme and bilirubin elevations during therapy, and with frequent biliary damage that can result in a secondary sclerosing cholangitis, which can be severe and lead to cirrhosis.
Background
Floxuridine (flox ure' i deen) is a fluoropyrimidine (fluorodeoxyuridine; FUDR) that has antineoplastic action against several solid tumors including liver, gastrointestinal adenocarcinoma and colorectal cancers. Floxuridine, like fluorouracil, requires conversion to monophosphate and possibly the triphosphate. It appears to act by inhibition of production or direct competition with thymidine triphosphate, which is necessary for DNA synthesis. Floxuridine was approved for use as an anticancer agent in the United States in 1970 and is given predominantly by continuous infusion into the hepatic artery to treat metastatic carcinoma of the colon or following resection of colon cancer metastases. Floxuridine is available as a powder for reconstitution in 500 mg vials (5 mL, 100 mg/mL) in several generic forms. Floxuridine is typically given by infusion pump into the hepatic artery in a dose of 0.1 to 0.6 mg/kg/day. Because the liver metabolizes floxuridine, administration by direct infusion into the hepatic artery deceases the systemic side effects which can be severe. Common side effects of intraarterial therapy include bone marrow suppression, fatigue, weakness, headache, dizziness, insomnia, paresthesias, abdominal pain, constipation, diarrhea, dyspepsia, nausea, stomatitis, and rash.
Hepatotoxicity
Serum aminotransferase elevations occur in a high proportion of patients given floxuridine by infusion into the hepatic artery, the reported rates ranging from 25% to 100%. These elevations are generally mild to moderate in severity and resolve with stopping therapy. "Chemical hepatitis," however, not infrequently is a cause of dose modification or delay in cycles of treatment. In addition, prolonged or repeated hepatic arterial infusions of FUDR can cause acalculous cholecystitis and multiple biliary strictures that can cause jaundice and a chronic sclerosing cholangitis-like syndrome. Between 5% and 25% of patients treated with hepatic arterial infusions of FUDR will develop symptomatic biliary strictures with pain and jaundice. These typically arise after 2 to 6 months of therapy, but can appear later, even more than a year after initiating FUDR therapy. The biliary strictures typically affect central bile ducts in the area of the porta hepatis, generally in and around the bifurcation of the common hepatic duct. Similar inflammation and fibrosis account for the acalculous cholecystitis that can occur with FUDR therapy, but which can be avoided by cholecystectomy at the time of hepatic resection of metastases or placement of the intraarterial infusion pump. The biliary strictures generally improve with stopping therapy, but can progress or require endoscopic or surgical intervention. Deaths from progressive biliary strictures and cholestatic liver injury have been described and can be a major cause of death among survivors of this metastatic tumor. The frequency of biliary strictures after FUDR therapy may be decreased by concurrent administration of dexamethasone and avoided by monitoring with hepatic and biliary imaging. However, the many complications of hepatic arterial infusion chemotherapy have decreased enthusiasm for this therapy, particularly with newer, more potent systemic antineoplastic agents.
Likelihood score: A (well known cause of clinically apparent liver and biliary injury).
Mechanism of Injury
FUDR can cause both hepatocellular (chemical hepatitis) and cholestatic (biliary strictures, cholangitis) injury. Both appear to be the direct, intrinsic toxicity of FUDR. In a dog animal model, the biliary injury can be reproduced with hepatic artery infusions and the hepatocellular injury (without bile duct damage) by portal vein infusions of FUDR.
Outcome and Management
The severity of the liver injury linked to floxuridine therapy ranges from minimal and transient serum enzyme elevations to severe cholestatic liver injury due to severe biliary strictures. Hepatic injury arising during FUDR therapy is a frequent reason for dose modification or delay in cycles of therapy. Appearance of jaundice due to hepatic arterial infusions of FUDR should lead to its discontinuation, as further therapy usually worsens the course. If the infusions are discontinued early, partial recovery with resolution of jaundice and symptoms is not uncommon. There is little evidence for cross sensitivity to hepatic injury among the various pyrimidine analogue antineoplastic agents. However, hepatic toxicity between floxuridine and fluorouracil can be additive.
Drug Class: Antineoplastic Agents
Other Drugs in the Subclass, Pyrimidine Analogues: Azacitidine, Capecitabine, Cytarabine, Decitabine, Fluorouracil, Gemcitabine, Trifluridine/Tipracil
CASE REPORT
Case 1. Sclerosing cholangitis due to intrahepatic infusions of floxuridine.
[Modified from: Ludwig J, Kim CH, Wiesner RH, Krom RA. Floxuridine-induced sclerosing cholangitis: an ischemic cholangiopathy? Hepatology 1989; 9: 215-8. PubMed Citation]
A 43 year old man was found to have a single hepatic metastasis 10 months after resection of a rectal adenocarcinoma. He underwent left hepatic lobectomy and placement of a subcutaneous infusion pump with a catheter in the common hepatic artery for adjuvant chemotherapy. Continuous intraarterial infusions of floxuridine [0.3 mg per kg per day for 2 weeks each month] were started. Because of liver test abnormalities, treatment was discontinued intermittently with subsequent improvement. After 21 months of treatment and 15 courses (total dose of 4.725 g), however, he developed persistent jaundice and pruritus. Serum bilirubin was 17.1 mg/dL, ALT 128 U/L and alkaline phosphatase 630 U/L. Values had been normal before therapy (Table). Endoscopic retrograde cholangiopancreatography showed strictures in the common bile duct. A liver biopsy revealed cholestatic hepatitis, paucity of intrahepatic bile ducts and marked periductular fibrosis. Therapy was discontinued, but he continued to worsen. A trial of prednisolone was unsuccessful. Within 6 months, he had developed signs of hepatic failure with ascites and intractable pruritus. He had no evidence of cancer recurrence, was placed on a liver transplant list and underwent successful orthotopic liver transplantation 2.5 years after starting chemotherapy.
Key Points
| Medication: | Floxuridine(by hepatic artery infusion) |
|---|---|
| Pattern: | Cholestatic (R=1.5) |
| Severity: | 4+ (progression to cirrhosis) |
| Latency: | 21 months |
| Recovery: | Incomplete |
| Other medications: | Not mentioned |
Laboratory Values
| Time After Starting | Time After Stopping | ALT (U/L) | Alk P (U/L) | Bilirubin (mg/dL) | Other |
|---|---|---|---|---|---|
| Pre | Pre | 24 | 175 | 0.9 | Before therapy |
| 0 | Pre | Started chemotherapy with hepatic arterial infusions of FUDR | |||
| 6 months | Pre | 118 | 485 | 7.1 | Therapy held transiently |
| 21 months | 0 | 128 | 630 | 17.1 | Therapy permanently stopped |
| 26 months | 5 months | 150 | 1206 | 29.2 | |
| 32 months | 11 months | 190 | 1242 | 21.2 | Liver transplantation |
| Normal Values | <32 | <239 | <1.2 | ||
Comment
Careful analysis of the explants at the time of liver transplantation showed no evidence of tumor recurrence. The liver was enlarged and the porta hepatis was scarred and difficult to dissect. Histologically there was obstructive arteriopathy and venopathy with partial occlusion of portal arterioles and venules. Bile ducts were obliterated and the periphery of the liver showed paucity of small bile ducts. Thus, the primary lesion was considered to be ischemic damage to bile ducts of the porta hepatis causing sclerosis, loss of intrahepatic ducts, obstructive jaundice and a secondary biliary cirrhosis.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Floxuridine – Generic
DRUG CLASS
Antineoplastic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Floxuridine | 50-91-9 | C9-H11-F-N2-O5 |
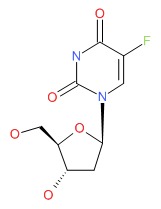 |
ANNOTATED BIBLIOGRAPHY
References updated: 02 February 2018
- Zimmerman HJ. Hepatotoxic effects of oncotherapeutic and immunosuppressive agents. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 673-708.(Expert review of hepatotoxicity of cancer chemotherapeutic agents published in 1999; mentions that pump intraarterial infusions of floxuridine (FUDR) cause a high rate of biochemical abnormalities and cause a sclerosing cholangitis-like syndrome in 5-100% of recipients, depending upon the dose and duration of therapy and the efforts made to identify the lesion).
- DeLeve LD. Cancer chemotherapy. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rdd ed. Amsterdam: Elsevier, 2013, p. 541-67.(Review of hepatotoxicity of cancer chemotherapeutic agents; mentions that floxuridine, when given as intrahepatic arterial infusion, can cause transient liver test abnormalities in 15-22% of patients and severe biliary sclerosis in 9%).
- Chabner BA, Bertino J, Cleary J, Ortiz T, Lane A, Supko JG, Ryan D. Cytotoxic agents. Chemotherapy of neoplastic diseases. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman.s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1677-730.(Textbook of pharmacology and therapeutics; FUDR is used primarily by continuous infusion into the hepatic artery for treatment of hepatic metastases).
- Chabner BA, Myers CE, Coleman CN, Johns DG. The clinical pharmacology of antineoplastic agents (first of two parts). N Engl J Med 1975; 292: 1107-13. [PubMed: 124015](Review of the pharmacology, metabolism and mechanism of action of methotrexate and fluorouracil).
- Stagg RJ, Lewis BJ, Friedman MA, Ignoffo RJ, Hohn DC. Hepatic arterial chemotherapy for colorectal cancer metastatic to the liver. Ann Intern Med 1984; 100: 736-43. [PubMed: 6231876](Review of the rationale, technique and efficacy of hepatic arterial chemotherapy for hepatic metastases of colorectal cancer, which was developed because of poor responses to systemic therapy; summarizing results in more than 1000 patients, including 445 given fluorouracil and 264 FUDR; little discussion of toxicity).
- Daly JM, Kemeny N, Oderman P, Botet J. Long-term hepatic arterial infusion chemotherapy. Arch Surg 1984; 119: 935-41. [PubMed: 6378147](40 patients with metastatic colorectal cancer underwent hepatic arterial infusions with FUDR; toxic effects were largely gastrointestinal with ulcers [30%], gastritis without ulcers [18%], elevations in bilirubin >3 mg/dL [23%], AST [65%], and extrahepatic bile duct strictures [5%]).
- Kemeny MM, Goldberg DA, Browning S, Metter GE, Miner PJ, Terz JJ. Experience with continuous regional chemotherapy and hepatic resection as treatment of hepatic metastases from colorectal primaries. A prospective randomized study. Cancer 1985; 55: 1265-70. [PubMed: 3971296](Among 46 patients with hepatic metastases from colorectal cancer treated with continuous hepatic artery infusions of FUDR, 58% had chemical hepatitis with ALT or AST >3 times ULN and mild jaundice, 8 also developed biliary strictures, and 6 of the first 19 required cholecystectomy for cholecystitis; one patient with strictures died of hepatic failure).
- Botet JF, Watson RC, Kemeny N, Daly JM, Yeh S. Cholangitis complicating intraarterial chemotherapy in liver metastasis. Radiology 1985; 156: 335-7. [PubMed: 3160063](Among 87 patients with metastatic colorectal cancer treated with hepatic arterial infusions of FUDR, 6 developed jaundice after 2 to 9 months of therapy, with biliary strictures resembling sclerosing cholangitis [largely around the bifurcation of the common bile duct], resolving with stopping but sometimes after several weeks of progressive worsening).
- Lafon PC, Reed K, Rosenthal D. Acute cholecystitis associated with hepatic arterial infusion of floxuridine. Am J Surg 1985; 150: 687-9. [PubMed: 2933968](Among 13 patients treated for hepatic metastases from colorectal cancer with hepatic arterial infusions of FUDR, 5 developed chemical cholecystitis [with obliterative fibrosis of the gallbladder and cystic duct] and one developed biliary strictures and jaundice, suggesting that cholecystectomy should be performed at the time of hepatectomy or pump placement).
- Hohn DC, Rayner AA, Economou JS, Ignoffo RJ, Lewis BJ, Stagg RJ. Toxicities and complications of implanted pump hepatic arterial and intravenous floxuridine infusion. Cancer 1986; 57: 465-70. [PubMed: 2935242](Among 35 patients with hepatic metastases from colorectal cancer treated with continuous hepatic arterial infusions of FUDR, all developed liver enzyme elevations during therapy and cholangiograms in 7 showed cholangiopathy in all, usually in or around the porta hepatis).
- Kemeny MM, Battifora H, Blayney DW, Cecchi G, Goldberg DA, Leong LA, Margolin KA, et al. Sclerosing cholangitis after continuous hepatic artery infusion of FUDR. Ann Surg 1985; 02: 176-81. [PMC free article: PMC1250871] [PubMed: 3160313](Among 46 patients with hepatic metastases from colorectal cancer treated with hepatic arterial infusions of FUDR, 8 [17%] developed biliary strictures, 2 to 10 months after starting chemotherapy [bilirubin 3.5-10.8 mg/dL, ALT 38-576 U/L, Alk P 460-2082 U/L], 2 of whom died).
- Shepard KV, Levin B, Karl RC, Faintuch J, DuBrow RA, Hagle M, Cooper RM, et al. Therapy for metastatic colorectal cancer with hepatic artery infusion chemotherapy using a subcutaneous implanted pump. J Clin Oncol 1985; 3: 161-9. [PubMed: 3155793](Among 53 patients with hepatic metastases from colorectal cancer treated with continuous hepatic arterial infusions of FUDR, 26 [49%] developed ALT or AST elevations >2 times ULN, and 13 jaundice at a mean of 2.8 months after starting, resolving in all with stopping).
- Pien EH, Zeman RK, Benjamin SB, Barth KH, Jaffe MH, Choyke PL, Clark LR, Paushter DM. Iatrogenic sclerosing cholangitis following hepatic arterial chemotherapy infusion. Radiology. 1985; 156: 329-30. [PubMed: 3160062](53 year old man with metastatic colon cancer treated with hepatic arterial infusions of FUDR for an undisclosed period developed jaundice [bilirubin "near 6" mg/dL] and biliary strictures suggestive of sclerosing cholangitis, which improved but did not completely resolve upon stopping the infusions).
- Shea WJ Jr, Demas BE, Goldberg HI, Hohn DC, Ferrell LD, Kerlan RK. Sclerosing cholangitis associated with hepatic arterial FUDR chemotherapy: radiographic-histologic correlation. AJR Am J Roentgenol 1986; 146: 717-21. [PubMed: 2937274](Among 17 patients receiving hepatic arterial infusions of FUDR who developed cholestasis, Alk P levels were >3 times ULN in all, and cholangiography showed strictures at the bifurcation of the common bile duct with segmental involvement and none at the distal bile duct; histology showed canalicular cholestasis, ductal proliferation, and pericholangitis; autopsies showed replacement of porta hepatis with hard mass of tissue composed entirely of scar with residual portal tracts).
- Doria MI Jr, Shepard KV, Levin B, Riddell RH. Liver pathology following hepatic arterial infusion chemotherapy. Hepatic toxicity with FUDR. Cancer 1986; 58: 855-61. [PubMed: 2941140](Hepatic histology in 8 patients with liver injury after hepatic arterial infusions of FUDR with jaundice arising after 24-95 weeks of treatment showed periductular and portal fibrosis, steatosis, mild inflammation, ductular proliferation and central vein lesions suggestive of sinusoidal obstruction syndrome).
- Pettavel J, Gardiol D, Bergier N, Schnyder P. Fatal liver cirrhosis associated with long-term arterial infusion of floxuridine. Lancet 1986; 2 (8516): 1162-3. [PubMed: 2877311](59 year old woman with hepatic metastases due to colon cancer was treated with hepatic arterial infusions of FUDR for 27 months and had minimal serum enzyme elevations during treatment but, nevetheless, developed cirrhosis which progressed to liver failure and death).
- Bolton JS, Bowen JC. Biliary sclerosis associated with hepatic artery infusion of floxuridine. Surgery 1986; 99: 119-22. [PubMed: 2934836](Two cases of biliary sclerosis after hepatic artery infusions with FUDR: 52 year old man and 32 year old woman developed jaundice after 3 and 2 cycles of therapy [bilirubin 17.4 and 4.0 mg/dL, ALT 1203 and 112 U/L, Alk P 1203 and 420 U/L], improving with stopping infusions with mild residual liver test abnormalities).
- Anderson SD, Holley HC, Berland LL, Van Dyke JA, Stanley RJ. Causes of jaundice during hepatic artery infusion chemotherapy. Radiology 1986; 161: 439-42. [PubMed: 2945226](Among 176 patients with hepatic metastases treated with hepatic arterial infusions of FUDR, 94 [54%] developed jaundice [bilirubin >2.0 mg/dL], 49 of whom were analyzed further, focal or diffuse stricturing was the most common cause, and in only 3 patients was jaundice due to the metastatic liver involvement).
- Laughlin EH. Common duct stricture associated with hepatic artery infusion of FUDR. J Surg Oncol 1986; 31: 56-9. [PubMed: 2935680](59 year old man with hepatic metastases from colon cancer developed jaundice after 34 weeks of hepatic artery infusions of FUDR [bilirubin 13.2 mg/dL], laparotomy showing stricturing at the bifurcation of the common bile duct).
- Bergmann JF, Rougier P, Liguory C, Zafrani ES, Méeau JM, Dhumeaux D. [Sclerosing cholangitis after chemotherapy by continuous hepatic intra-arterial infusion of fluorodeoxyuridine]. Gastroenterol Clin Biol 1986; 10: 177-9. French. [PubMed: 2939001](64 year old man with hepatic metastases from colorectal cancer developed jaundice 2 months after starting hepatic arterial infusions of FUDR [bilirubin 2.7 mg/dL, ALT 1122 U/L, Alk P 795 U/L], with biliary strictures and improving after endoscopic stenting).
- Pietrafitta JJ, Anderson BG, O'Brien MJ, Deckers PJ. Cholecystitis secondary to infusion chemotherapy. J Surg Oncol 1986; 31: 287-93. [PubMed: 2941626](39 year old woman developed chemical cholecystitis and recurrent pain during hepatic artery infusions of FUDR without biliary strictures and a shrunken, fibrotic gallbladder at surgery, later tolerating the FUDR infusions without pain).
- Kemeny N, Daly J, Reichman B, Geller N, Botet J, Oderman P. Intrahepatic or systemic infusion of fluorodeoxyuridine in patients with liver metastases from colorectal carcinoma. A randomized trial. Ann Intern Med 1987; 107: 459-65. [PubMed: 2957943](Among 99 patients with hepatic metastases from colorectal cancer treated with 14 day courses of intravenous [iv] vs hepatic artery infusions [hai] of FUDR monthly, AST elevations occurred in 24% of iv- vs 42% of hai-treated patients, and biliary abnormalities arose in none vs 4 [9%]).
- Shepard KV, Levin B, Faintuch J, Doria MI, DuBrow RA, Riddell RH. Hepatitis in patients receiving intraarterial chemotherapy for metastatic colorectal carcinoma. Am J Clin Oncol 1987; 10: 36-40. [PubMed: 2950752](Among 51 patients with metastatic colorectal cancer treated with hepatic arterial infusions of FUDR with either dichloromethotrexate or mitomycin C, 24 [47%] developed hepatitis 1 week to 8 months after starting therapy [bilirubin 3.0-12.5 mg/dL, ALT 26-710 U/L, mean Alk P 550 U/L]; no mention of biliary imaging or description of ultimate outcome).
- Clark RA, Gallant TE. Bile duct strictures associated with hepatic arterial infusion chemotherapy. Gastrointest Radiol 1987; 12: 148-51. [PubMed: 2951292](Six patients with metastatic colon cancer developed biliary strictures after 3-21 months of hepatic artery infusions of FUDR [bilirubin 4 to 27 mg/dL, ALT and Alk P raised in all]; strictures were shown by CT scans or ERCP).
- Ludwig J, Kim CH, Wiesner RH, Krom RA. Floxuridine-induced sclerosing cholangitis: an ischemic cholangiopathy? Hepatology 1989; 9: 215-8. [PubMed: 2521475](43 year old man with colorectal cancer developed jaundice after 18 months of hepatic artery infusions of FUDR [bilirubin 17.1 mg/dL, ALT 128 U/L, Alk P 630 U/L], progressing to liver failure and transplantation; explant showed sclerosing cholangitis and obliteration of arteries and small portal veins in the perihilar area, suggesting ischemia as the cause of cholangiopathy).
- Andrews JC, Knol J, Wollner I, Knutsen C, Smith P, Prieskorn D, Ensminger W. Floxuridine-associated sclerosing cholangitis. A dog model. Invest Radiol 1989; 24: 47-51. [PubMed: 2521845](Infusion of FUDR but not saline into the hepatic artery of dogs led to rises in Alk P, ALT and bilirubin within 2-4 weeks, accompanied by strictures of the central bile ducts and attenuation of intrahepatic ducts, improving slightly but not resolving completely with stopping the infusions).
- Nakhleh RE, Wesen C, Snover DC, Grage T. Venoocclusive lesions of the central veins and portal vein radicles secondary to intraarterial 5-fluoro-2'-deoxyuridine infusion. Hum Pathol 1989; 20: 1218-20. [PubMed: 2531719](Abstract: liver at autopsy of a patient with biliary strictures due to hepatic arterial infusions of FUDR showed changes of sinusoidal obstruction syndrome and obliteration of portal vein radicles).
- Wagman LD, Kemeny MM, Leong L, Terz JJ, Hill LR, Beatty JD, Kokal WA, et al. A prospective, randomized evaluation of the treatment of colorectal cancer metastatic to the liver. J Clin Oncol 1990; 8: 1885-93. [PubMed: 2146370](91 patients with hepatic metastases from colorectal cancer were randomized into 6 treatment arms with FUDR; after 4-5 year follow up, 79 [87%] had died of progressive disease and 5 [5.5%] of sclerosing cholangitis).
- Andrews JC, Kuntsen C, Terio P, Priescorn D, Ensminger WD. Hepatobiliary toxicity of 5-fluoro-2'-deoxyuridine. Intra-arterial versus portal venous routes of infusion. Invest Radiol 1991; 26: 461-4. [PubMed: 1829068](Infusion of FUDR into the portal vein of dogs resulted in ALT, Alk P and bilirubin elevations similar to that seen with hepatic artery infusions; however, no biliary strictures were seen, indicating direct toxicity to the central bile ducts rather than toxicity of a metabolite excreted in bile).
- Horsmans Y, Harvengt C. [Secondary drug-induced cholestasis with bile duct involvement]. Acta Gastroenterol Belg 1991; 54: 27-33. French. [PubMed: 2058347](Review of the causes and mechanisms of drug induced cholestasis due to biliary injury; biliary strictures occur in 5-30% of persons who receive FUDR by hepatic artery infusion).
- Pozniak MA, Babel SG, Trump DL. Complications of hepatic arterial infusion chemotherapy. Radiographics 1991; 11: 67-79. [PubMed: 1825358](Demonstration of radiologic features of complications of continuous hepatic artery infusions with FUDR; among 45 patients treated, 24% developed hepatitis and 7% sclerosing cholangitis).
- Rougier P, Laplanche A, Huguier M, Hay JM, Ollivier JM, Escat J, Salmon R, et al. Hepatic arterial infusion of floxuridine in patients with liver metastases from colorectal carcinoma: long-term results of a prospective randomized trial. J Clin Oncol 1992; 10: 1112-8. [PubMed: 1296590](Among 163 patients with liver metastases from colorectal cancer randomized to receive hepatic arterial infusions of FUDR or systemic therapy, 28 of 72 [39%] treated with hepatic artery infusions developed "chemical hepatitis" and 19 [26%] sclerosing cholangitis).
- Kemeny N, Seiter K, Niedzwiecki D, Chapman D, Sigurdson E, Cohen A, Botet J, et al. A randomized trial of intrahepatic infusion of fluorodeoxyuridine with dexamethasone versus fluorodeoxyuridine alone in the treatment of metastatic colorectal cancer. Cancer 1992; 69: 327-34. [PubMed: 1303612](Among 50 patients with metastatic colorectal cancer treated with hepatic arterial infusions of FUDR with or without dexamethasone, those given corticosteroids had lower rates of elevations in bilirubin [9% vs 30%], Alk P [57% vs 67%], AST [52% vs 57%] and of sclerosing cholangitis [0% vs 6%], as well as slightly higher response rates and survival).
- Kemeny N, Huang Y, Cohen AM, Shi W, Conti JA, Brennan MF, Bertino JR, et al. Hepatic arterial infusion of chemotherapy after resection of hepatic metastases from colorectal cancer. N Engl J Med 1999; 341: 2039-48. [PubMed: 10615075](156 patients with hepatic metastases from colorectal cancer were treated with intravenous 5-FU and leucovorin with or without 6 cycles of hepatic arterial infusions of FUDR with dexamethasone; FUDR therapy was associated with better survival, but Alk P elevations >2 times ULN occurred in 29%, AST >3 times ULN in 65%, bilirubin >3 mg/dL in 18%, and fatal sclerosing cholangitis in 2 [3%] patients on FUDR).
- Aldrighetti L, Arru M, Ronzoni M, Salvioni M, Villa E, Ferla G. Extrahepatic biliary stenoses after hepatic arterial infusion(HAI) of floxuridine(FUdR) for liver metastases from colorectal cancer. Hepatogastroenterology 2001; 48: 1302-7. [PubMed: 11677951](Among 54 patients treated with 9 to 19 cycles of 14 day hepatic arterial infusions of FUDR with dexamethasone, 5 [9%] developed jaundice and biliary complications [bilirubin 1.0-48 mg/dL, ALT 50-683 U/L, Alk P 428-4155 U/L], all of whom had strictures in the common bile duct and all improved with stopping therapy, with or without endoscopic or percutaneous balloon dilatation).
- Barnett KT, Malafa MP. Complications of hepatic artery infusion: a review of 4580 reported cases. Int J Gastrointest Cancer 2001; 30: 147-60. [PubMed: 12540027](Systematic review of literature on complications of hepatic artery infusion therapy of cancer; in 23 randomized trials, mortality rate was 1% with "chemical hepatitis" in 5% using 5-FU alone vs 31% with FUDR alone, biliary toxicity in <1% vs 14%, and sclerosing cholangitis in <1% vs 12%).
- Phongkitkarun S, Kobayashi S, Varavithya V, Huang X, Curley SA, Charnsangavej C. Bile duct complications of hepatic arterial infusion chemotherapy evaluated by helical CT. Clin Radiol 2005; 60: 700-9. [PubMed: 16038698](Among 60 patients who received hepatic arterial infusions of FUDR and were monitored every 3 months by helical CT, bile duct abnormalities were identified in 34 [57%] after 1-12 months of therapy, 10 of whom developed progressive jaundice requiring intervention).
- Sandrasegaran K, Alazmi WM, Tann M, Fogel EL, McHenry L, Lehman GA. Chemotherapy-induced sclerosing cholangitis. Clin Radiol 2006; 61: 670-8. [PubMed: 16843750](Description of 11 patients with FUDR [n=9] or 5-FU [n=2] induced sclerosing cholangitis who underwent ERCP at a single institution; onset after 2-132 months of therapy with jaundice, pruritus or liver test abnormalities [bilirubin 0.4 to 17.6 mg/dL, Alk P 191-1106 U/L]).
- Alazmi WM, McHenry L, Watkins JL, Fogel EL, Schmidt S, Sherman S, Lehman GL. Chemotherapy-induced sclerosing cholangitis: long-term response to endoscopic therapy. J Clin Gastroenterol. 2006; 40: 353-7. [PubMed: 16633109](Description of 11 patients with FUDR [n=9] or 5-FU [n=2] induced sclerosing cholangitis who underwent ERCP at a single institution, strictures were typically in the common hepatic duct near the bifurcation).
- Bolton JS, O'Connell MJ, Mahoney MR, Farr GH Jr, Fitch TR, Maples WJ, Nagorney DM, et al. Hepatic arterial infusion and systemic chemotherapy after multiple metastasectomy in patients with colorectal carcinoma metastatic to the liver: a North Central Cancer Treatment Group (NCCTG) phase II study, 92-46-52. Clin Colorectal Cancer 2012; 11: 31-7. [PMC free article: PMC3249000] [PubMed: 21729678](Among 49 patients with complete resection of liver metastases from colorectal cancer who were treated with either FUDR or systemic chemotherapy with 5-FU and leucovorin, elevated liver enzymes occurred in 5 [14%], chemical hepatitis in 10 [28%], no mention of biliary strictures).
- Ito K, Ito H, Kemeny NE, Gonen M, Allen PJ, Paty PB, Fong Y, et al. Biliary sclerosis after hepatic arterial infusion pump chemotherapy for patients with colorectal cancer liver metastasis: incidence, clinical features, and risk factors. Ann Surg Oncol 2012; 19: 1609-17. [PubMed: 21989666](Retrospective review of 475 patients treated with hepatic arterial infusions of chemotherapy identified 29 patients who developed jaundice which did not resolve with stopping therapy and required stenting, which was associated with higher dosing per cycle, abnormal flow scans, and postoperative infections; no patient died of biliary complications).
- Ang C, Jhaveri K, Patel D, Gewirtz A, Seidman A, Kemeny N. Hepatic arterial infusion and systemic chemotherapy for breast cancer liver metastases. Breast J 2013; 19: 96-9. [PubMed: 23173748](Among 9 women with advanced, metastatic breast cancer, who were treated with hepatic arterial infusions of FUDR and dexamethasone combined with other systemic anticancer agents, 4 had liver enzyme elevations attributable to therapy and 3 discontinued the infusions because of liver test abnormalities).
- Magge D, Choudry HA, Zeh HJ 3rd, Cunningham DE, Steel J, Holtzman MP, Jones HL, et al. Outcome analysis of a decade-long experience of isolated hepatic perfusion for unresectable liver metastases at a single institution. Ann Surg 2014; 259: 953-9. [PubMed: 24169176](Among 88 patients with unresectable liver metastases who underwent intrahepatic artery perusion with floxuridine at a single US referral center between 2003 and 2012, ALT elevations above 5 times ULN occurred in 44% and 5 developed "salvageable hepatic failure").
- Cercek A, D'Angelica M, Power D, Capanu M, Gewirtz A, Patel D, Allen P,et al. Floxuridine hepatic arterial infusion associated biliary toxicity is increased by concurrent administration of systemic bevacizumab. Ann Surg Oncol 2014; 21: 479-86. [PubMed: 24154839](Among 203 patients from 3 prospective studies of hepatic artery infusions of floxuridine with or without bevacizumab [monoclonal anti-VEGF] for hepatic metastases, liver test abnormalities and biliary stenting was required more frequently when bevacizumab was used [13% vs 0%]).
- DʼAngelica MI, Correa-Gallego C, Paty PB, Cercek A, Gewirtz AN, Chou JF, Capanu M, et al. Phase II trial of hepatic artery infusional and systemic chemotherapy for patients with unresectable hepatic metastases from colorectal cancer: conversion to resection and long-term outcomes. Ann Surg 2015; 261: 353-60. [PMC free article: PMC4578807] [PubMed: 24646562](Among 49 patients with colorectal cancer who had unresectable hepatic metastases and received hepatic artery infusions of floxuridine, 23 were able to undergo successful resection of the metastases and 10 had no evidence of disease 2-5 years later; AST elevations above 5 times ULN occurred in 8 [16%] and biliary stenting was required in 4 [8%]).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52.e7. (Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 49 [5.5%] [PMC free article: PMC4446235] [PubMed: 25754159]were attributed to anticancer agents, but none to floxuridine).
- Chang W, Wei Y, Ren L, Zhong Y, Yu Y, Chen J, Zhu D, et al. Randomized controlled trial of intraportal chemotherapy combined with adjuvant chemotherapy (mFOLFOX6) for stage II and III colon cancer. Ann Surg 2016; 263: 434-9. [PubMed: 26465781](Among 237 pateints with metastatic colorectal cancer treated with folinic acid, floxuridine and oxaplatin [FOLFOX], ALT or AST elevations were more frequent in a group that also received intraoperative intraportal chemotherapy [6% vs 1%], but there were no liver related severe adverse events).
- Kemeny NE, Chou JF, Boucher TM, Capanu M, DeMatteo RP, Jarnagin WR, Allen PJ, et al. Updated long-term survival for patients with metastatic colorectal cancer treated with liver resection followed by hepatic arterial infusion and systemic chemotherapy. J Surg Oncol 2016; 113: 477-84. [PMC free article: PMC5076474] [PubMed: 26830685](Long term follow up on 287 patients with colorectal cancer and liver metastases who were enrolled in 4 prospective trials of intrahepatic artery infusions of floxuridine with leucovorin, oxaliplatin or irinotecan, the overall 10 year survival was 34% and the major complication of the therapy was biliary sclerosis which occurred in 3%).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Extrahepatic biliary stenoses after hepatic arterial infusion (HAI) of floxuridine (FUdR) for liver metastases from colorectal cancer.[Hepatogastroenterology. 2001]Extrahepatic biliary stenoses after hepatic arterial infusion (HAI) of floxuridine (FUdR) for liver metastases from colorectal cancer.Aldrighetti L, Arru M, Ronzoni M, Salvioni M, Villa E, Ferla G. Hepatogastroenterology. 2001 Sep-Oct; 48(41):1302-7.
- A randomized trial of continuous intravenous versus hepatic intraarterial floxuridine in patients with colorectal cancer metastatic to the liver: the Northern California Oncology Group trial.[J Clin Oncol. 1989]A randomized trial of continuous intravenous versus hepatic intraarterial floxuridine in patients with colorectal cancer metastatic to the liver: the Northern California Oncology Group trial.Hohn DC, Stagg RJ, Friedman MA, Hannigan JF Jr, Rayner A, Ignoffo RJ, Acord P, Lewis BJ. J Clin Oncol. 1989 Nov; 7(11):1646-54.
- Hepatobiliary toxicity of 5-fluoro-2'-deoxyuridine. Intra-arterial versus portal venous routes of infusion.[Invest Radiol. 1991]Hepatobiliary toxicity of 5-fluoro-2'-deoxyuridine. Intra-arterial versus portal venous routes of infusion.Andrews JC, Kuntsen C, Terio P, Priescorn D, Ensminger WD. Invest Radiol. 1991 May; 26(5):461-4.
- Review Complications of hepatic artery infusion: a review of 4580 reported cases.[Int J Gastrointest Cancer. 2001]Review Complications of hepatic artery infusion: a review of 4580 reported cases.Barnett KT, Malafa MP. Int J Gastrointest Cancer. 2001; 30(3):147-60.
- Review The role of floxuridine in metastatic liver disease.[Mol Cancer Ther. 2009]Review The role of floxuridine in metastatic liver disease.Power DG, Kemeny NE. Mol Cancer Ther. 2009 May; 8(5):1015-25. Epub 2009 Apr 21.
- Floxuridine - LiverToxFloxuridine - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...