NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Sertraline is a selective serotonin reuptake inhibitor (SSRI) used in the therapy of depression, anxiety disorders and obsessive-compulsive disorder. Sertraline therapy can be associated with transient asymptomatic elevations in serum aminotransferase levels and has been linked to rare instances of clinically apparent acute liver injury.
Background
Sertraline (ser' tra leen) is a selective serotonin reuptake inhibitor (SSRI) that acts by blocking the reuptake of serotonin in CNS synaptic clefts, thus increasing serotonin levels in the brain which is associated with its psychiatric effects. Sertraline was approved for use in the United States in 1991, and it remains in wide use, with almost 40 million prescriptions being filled yearly. Indications for sertraline include major depression, obsessive-compulsive disorder, panic disorder, and major anxiety disorders including social anxiety, post-trauma stress and generalized anxiety disorder. Sertraline is also used for headache, premenstrual dysphoric disorder, diabetic neuropathy and premature ejaculation. Sertraline is available as tablets of 25, 50 and 100 mg and as an oral suspension in multiple generic forms and under the brand name of Zoloft. The recommended dosage for depression in adults is 50 or 100 mg once daily, increasing the dosage by 25 or 50 mg increments to a maximum of 200 mg. Common side effects are drowsiness, dyspepsia, nausea, headache, increased sweating, increased appetite, weight gain and sexual dysfunction. Rare but potentially severe adverse events include suicidal ideation and behavior, activation of mania, serotonin syndrome, discontinuation syndrome, increased risk of bleeding, seizures, acute glaucoma, hypersensitivity reactions and embryo-fetal toxicity.
Hepatotoxicity
Liver test abnormalities have been reported to occur in up to 1% of patients on sertraline, but elevations are usually modest and infrequently require dose modification or discontinuation. Rare instances of acute, clinically apparent episodes of liver injury with marked liver enzyme elevations with or without jaundice have been reported in patients on sertraline. The onset of injury is usually within 2 to 24 weeks and the pattern of serum enzyme elevations has varied from hepatocellular to mixed and cholestatic. Autoimmune (autoantibodies) and immunoallergic features (rash, fever, eosinophilia) are uncommon. Acute liver failure due to sertraline has been described but is very rare.
Likelihood score: B (likely but rare cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism by which sertraline causes liver injury is not known. Sertraline is metabolized at least in part by the liver, mainly via the cytochrome P450 system and PYP 2D6 and 2B6 which can cause drug-drug interactions. The hepatotoxicity of sertraline may be mediated by toxic intermediates of its metabolism.
Outcome and Management
The serum aminotransferase elevations that occur on sertraline therapy are usually self-limited and do not require dose modification or discontinuation of therapy. Rare instances of acute liver failure have been attributed to sertraline therapy. Rechallenge usually results in recurrence of liver injury and should be avoided. Persons with intolerance to sertraline may have similar reactions to other SSRIs and careful monitoring is warranted if other such agents are used.
Drug Class: Antidepressant Agents
Other Drugs in the Subclass, SNRIs/SSRIs: Citalopram, Escitalopram, Duloxetine, Fluoxetine, Fluvoxamine, Levomilnacipran, Paroxetine, Venlafaxine, Vilazodone, Vortioxetine
CASE REPORT
Case 1. Acute liver injury due to sertraline.(1)
A 44 year old woman with mild reactive depression was treated with sertraline (50 mg daily) and developed fatigue followed by pruritus and jaundice 4-5 weeks later. She was also on levothyroxine and birth control pills which she had been taking for several years. She drank little alcohol and had no previous history of liver disease or known exposures to hepatitis. On presentation, she was jaundiced but had no fever or rash. Laboratory tests showed elevations in serum bilirubin and enzyme levels (Table), which were reported to have been normal in the past. She was admitted for evaluation; sertraline and the oral contraceptives were discontinued. Tests for hepatitis A, B and C were negative. There were low titers of antinuclear antibody (ANA 1:40), but no smooth muscle or mitochondrial antibodies. Abdominal ultrasound showed no evidence of biliary obstruction. She began to improve without specific therapy; jaundice resolved within 1 month, pruritus within 2 months and laboratory tests were normal at 6 months after presentation. Oral contraceptives were restarted without further incident.
Key Points
| Medication: | Sertraline |
|---|---|
| Pattern: | Initially mixed (R=2.5), later cholestatic (R=1.2) |
| Severity: | 3+ (jaundice, hospitalization) |
| Latency: | 1 month |
| Recovery: | 1-2 months symptomatically, 6 months biochemically |
| Other medications: | Birth control pills, levothyroxine |
Laboratory Values
| Time After Starting | Time After Stopping | ALT (U/L) | Alk P (U/L) | Bilirubin (mg/dL) | Comments |
|---|---|---|---|---|---|
| Sertraline taken for 5 weeks | |||||
| 1 month | 0 | 300 | 333 | 4.2 | Sertraline stopped |
| 1 week | 236 | 299 | 5.1 | Ultrasound normal | |
| 2 weeks | 116 | 311 | 3.3 | ||
| 2 months | 4 weeks | 132 | 253 | 1.8 | |
| 3 months | 2 months | 84 | 173 | 0.8 | |
| 5 months | 4 months | 44 | Normal | 0.6 | |
| 7 months | 6 months | Normal | Normal | 0.6 | |
| Normal Values | <40 | <115 | <1.2 | ||
- *
Converted from times the upper limit of normal to U/L using normals provided.
Comment
More than 20 million prescriptions for sertraline are filled yearly in the United States, and therapy is typically long term. Nevertheless, cases of clinically apparent liver disease from sertraline are rare. This case was typical with an onset within 1 to 3 months of starting therapy and a somewhat prolonged course of cholestatic hepatitis, but with ultimate recovery. When patients develop acute liver injury from an SSRI, it is not clear whether another member of this group can be substituted. A structurally unrelated substitute along with careful monitoring is perhaps prudent if antidepressant therapy is considered necessary.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Sertraline – Generic, Zoloft®
DRUG CLASS
Antidepressant Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Sertraline | 79617-96-2 | C17-H17-C12-N |
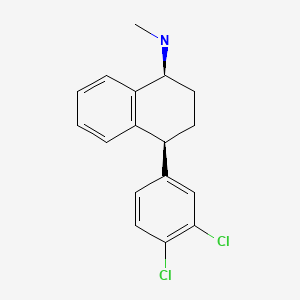
|
CITED REFERENCE
- 1.
- Hautekeete ML, Colle I, van Vlierberghe H, Elewaut A. Symptomatic liver injury probably related to sertraline. Gastroenterol Clin Biol. 1998;22:364–5. [PubMed: 9762229]
ANNOTATED BIBLIOGRAPHY
References updated: 08 April 2020
Abbreviations: MAO inhibitor, monoamine oxidase inhibitor; SSRI, selective serotonin reuptake inhibitor; SNRI, serotonin and norepinephrine reuptake inhibitor.
- Zimmerman HJ. Antidepressants. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 493-8.(Expert review of hepatotoxicity published in 1999; reports that one case of acute drug-induced liver injury attributed to sertraline has been published).
- Larrey D, Ripault MP. Hepatotoxicity of psychotropic drugs and drugs of abuse. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 443-62.(Review of hepatotoxicity of antidepressants mentions that clinically apparent liver injury from the SSRIs is rare and sertraline has been implicated in only a few cases of severe hepatic injury).
- O'Donnell JM, Bies RR, Shelton RC. Drug therapy of depression and anxiety disorders. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 267-77.(Textbook of pharmacology and therapeutics).
- Doogan DP. Toleration and safety of sertraline: experience worldwide. Int Clin Psychopharmacol. 1991;6 Suppl 2:47–56. [PubMed: 1806630](Rates of drug discontinuation for serum enzyme elevations were 0.5% for 1902 patients on sertraline vs 0.6% of 500 on active comparators and 0.0% of 666 on placebo; no cases of clinically apparent liver injury).
- Menon RR, Howard R. Sertraline and liver toxicity in the elderly. Int J Geriatr Psychiatry. 1994;9:332–4.(Two cases of sertraline hepatotoxicity; 81 year old man had a rise in AST [36→98 U/L] and Alk P [78→452 U/L] without jaundice 3 weeks after starting sertraline, resolving within 2 months of stopping; 84 year old woman developed rise in ALT [1148 U/L] and Alk P [117→549 U/L], with subsequent multiorgan failure and death; few specific details given).
- Hautekeete ML, Colle I, van Vlierberghe H, Elewaut A. Symptomatic liver injury probably related to sertraline. Gastroenterol Clin Biol. 1998;22:364–5. [PubMed: 9762229](44 year old woman developed jaundice, fatigue and itching 4-5 weeks after starting sertraline [bilirubin 4.2 mg/dL, ALT 7.5 times ULN, Alk P 2.9 times ULN], resolving within few months of stopping).
- Mourilhe P, Stokes PE. Risks and benefits of selective serotonin reuptake inhibitors in the treatment of depression. Drug Saf. 1998;18:57–82. [PubMed: 9466088](Review of pharmacology, efficacy and safety of SSRIs; no mention of ALT elevations or hepatotoxicity).
- Grohmann R, Rüther E, Engel RR, Hippius H. Assessment of adverse drug reactions in psychiatric inpatients with the AMSP drug safety program: methods and first results for tricyclic antidepressants and SSRI. Pharmacopsychiatry. 1999;32:21–8. [PubMed: 10071179](Analysis of reporting of adverse events among inpatients in 29 German hospitals between 1993 to 1997; 896 severe adverse events among 48,564 patients [1.8%], both total and hepatic events were more common with tricyclics than SSRIs).
- Kim KY, Hwang W, Narendran R. Acute liver damage possibly related to sertraline and venlafaxine ingestion. Ann Pharmacother. 1999;33:381–2. [PubMed: 10200868](27 year old man took overdose of sertraline and cephalexin and had elevations of ALT to 1247 U/L, bilirubin 2.1 mg/dL; switched to venlafaxine, but 1 week later developed abdominal pain with bilirubin 1.6 mg/dL and ALT 814 U/L, improving on stopping but relapsing 3 days after restarting sertraline; recovered on stopping all SSRIs).
- Verrico MM, Nace DA, Towers AL. Fulminant chemical hepatitis possibly associated with donepezil and sertraline therapy. J Am Geriatr Soc. 2000;48:1659–63. [PubMed: 11129758](83 year old woman developed confusion and jaundice 4 months after starting sertraline and 10 days after starting donepezil [bilirubin 5.6 mg/dL, ALT 529 U/L and Alk P 369 U/L], resolving within 4 months of stopping both).
- Fartoux-Heymann L, Hézode C, Zafrani ES, Dhumeaux D, Mallat A. Acute fatal hepatitis related to sertraline. J Hepatol. 2001;35:683–4. [PubMed: 11690719](54 year old man with alcoholism developed jaundice within 2 weeks of starting sertraline [bilirubin 10.5 mg/dL, ALT 906 U/L, Alk P 121 U/L, eosinophilia and prothrombin activity of 30%], and progressed to liver failure and death within 10 days, autopsy showing extensive necrosis without fat or Mallory bodies).
- Carvajal García-Pando A, García del Pozo J, Sánchez AS, Velasco MA, Rueda de Castro AM, Lucena MI. Hepatotoxicity associated with the new antidepressants. J Clin Psychiatry. 2002;63:135–7. [PubMed: 11874214](Analysis of cases of hepatotoxicity from antidepressants in Spanish Pharmacovigilance System from 1989-1999, identified 99 cases; among SSRIs, 26 were due to fluoxetine, 14 paroxetine, 6 fluvoxamine, 5 sertraline, 3 venlafaxine and 2 citalopram; among tricyclics, 16 were due to clomipramine 7 amitriptyline, 6 imipramine; among miscellaneous, 3 were due to nefazodone and 1 trazodone; but all had a similar incidence=1-3 per 100,000 patient-years of exposure, except for nefazodone=29 per 100,000).
- Lucena MI, Carvajal A, Andrade RJ, Velasco A. Antidepressant-induced hepatotoxicity. Expert Opin Drug Saf. 2003;2:249–62. [PubMed: 12904104](Review of hepatotoxicity of antidepressants; antidepressant use has increased markedly between 1992 and 2002, accounting for 5% of cases of hepatotoxicity; SSRIs are less likely to cause injury than tricyclics and MAO inhibitors; range of presentations, typically self-limited and rapid recovery; no hallmarks of hypersensitivity).
- Persky S, Reinus JF. Sertraline hepatotoxicity: a case report and review of the literature on selective serotonin reuptake inhibitor hepatotoxicity. Dig Dis Sci. 2003;48:939–44. [PubMed: 12772794](23 year old woman developed fever and nausea during sertraline therapy [bilirubin 2.1 mg/dL, ALT ~850 U/L], resolving upon stopping and recurring [ALT~230 U/L] on restarting for 3 days).
- Spigset O, Hägg S, Bate A. Hepatic injury and pancreatitis during treatment with serotonin reuptake inhibitors: data from the World Health Organization (WHO) database of adverse drug reactions. Int Clin Psychopharmacol. 2003;18:157–61. [PubMed: 12702895](Among 27,542 reports of hepatic injury in WHO database, 786 were related to SSRIs [3%], including citalopram 42, fluoxetine 222, fluvoxamine 54, paroxetine 191, sertraline 112, nefazodone 91 and venlafaxine 74; only nefazodone has an excess of hepatic reports in relationship to total reports).
- Degner D, Grohmann R, Kropp S, Rüther E, Bender S, Engel RR, Schmidt LG. Severe adverse drug reactions of antidepressants: results of the German multicenter drug surveillance program AMSP. Pharmacopsychiatry. 2004;37 Suppl 1:S39–45. [PubMed: 15052513](Analysis of adverse drug reactions reported from 1993-2000 in 35 psychiatric hospitals; 0.7% of SSRI recipients had a severe adverse event; hepatic in 0.05%).
- Solomons K, Gooch S, Wong A. Toxicity with selective serotonin reuptake inhibitors. Am J Psychiatry. 2005;162:1225. [PubMed: 15930079](38 year old woman developed abdominal pain and ALT elevations [378 U/L] without jaundice 9 days after starting fluvoxamine; then had a positive rechallenge and recurrence with starting citalopram [ALT 379 within 4 days], and positive rechallenge with citalopram again 1 year later).
- Pinzani V, Peyriere H, Hillaire-Buys D, Pageaux GP, Blayac BP, Larrey D. Specific serotonin recapture inhibitor (SSRI) antidepressants: hepatoxicity assessment in a large cohort in France. J Hepatol. 2006;44:S256.(Abstract: Analysis of French Pharmacovigilance data on SSRIs found 63 cases of hepatotoxicity from paroxetine, 45 fluoxetine, 30 citalopram, 18 sertraline, and 2 fluvoxamine).
- Sabaté M, Ibáñez L, Pérez E, Vidal X, Buti M, Xiol X, Mas A, et al. Risk of acute liver injury associated with the use of drugs: a multicentre population survey. Aliment Pharmacol Ther. 2007;25:1401–9. [PubMed: 17539979](Among 126 cases of drug induced liver injury seen in Spain between 1993-2000, 3 were attributed to paroxetine and 3 to fluoxetine, with a relative risk of injury to rate of use in the population of 3.0 and 1.8, respectively).
- DeSanty KP, Amabile CM. Antidepressant-induced liver injury. Ann Pharmacother. 2007;41:1201–11. [PubMed: 17609231](Review of drug induced liver injury and reports of injury from MAO inhibitors, SSRIs, tricyclics and atypical agents).
- Collados Arroyo V, Plaza Aniorte J, Hallal H, Perez Cuadradob E. Farm Hosp. 2008;32:60–1. [Hepatotoxicity associated with sertraline] [PubMed: 18426707](47 year old man developed fatigue one month after starting sertraline [bilirubin 2.7 mg/dL, ALT 500 U/L, Alk P 377 U/L], resolving within 3 months of stopping).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected from 2004 to 2008, 6 were attributed to duloxetine, 3 atomoxetine, 2 fluoxetine, 2 bupropion, and 1 sertraline as single agents).
- Tabak F, Gunduz F, Tahan V, Tabak O, Ozaras R. Sertraline hepatotoxicity: report of a case and review of the literature. Dig Dis Sci. 2009;54:1589–91. [PubMed: 18958618](17 year old boy developed jaundice 6 months after starting sertraline [bilirubin 2.1 mg/dL, ALT 1280 U/L, Alk P 483 U/L], resolving within 6 months of stopping).
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, one was attributed to venlafaxine and one to fluoxetine but none to sertraline).
- Collados V, Hallal H, Andrade RJ. Sertraline hepatotoxicity: report of a case and review of the literature. Dig Dis Sci. 2010;55:1806–7. [PubMed: 20411428](Review of published cases of sertraline hepatotoxicity mentions 4 cases [bilirubin 2.6 to 10.5 mg/dL, ALT 144-906 U/L, Alk P 121-1034 U/L], one fatal and three resolving within 3-6 months).
- García-Aparicio J, Herrero-Herrero JI. Farm Hosp. 2010;34:152–4. [Toxic hepatitis following sequential treatment with cotrimoxazol, levofloxacin, doxycycline and sertraline in a patient with a respiratory infection] Spanish. [PubMed: 20471573](65 year old woman developed jaundice several weeks after receiving several antibiotics and 15 days after starting sertraline [bilirubin 3.5 mg/dL, ALT 937 U/L, Alk P 373 U/L], resolving within 3 months of stopping sertraline).
- Molleston JP, Fontana RJ, Lopez MJ, Kleiner DE, Gu J, Chalasani N. Drug-induced Liver Injury Network. Characteristics of idiosyncratic drug-induced liver injury in children: results from the DILIN prospective study. J Pediatr Gastroenterol Nutr. 2011;53:182–9. [PMC free article: PMC3634369] [PubMed: 21788760](Among 30 children with suspected drug induced liver injury, half [n=15] were due to antimicrobials [minocycline 4, INH 3, azithromycin 3] and the rest largely due to CNS agents and anticonvulsants; one case was attributed to amitriptyline, but sertraline was not listed).
- Park SH, Ishino R. Liver injury associated with antidepressants. Curr Drug Saf. 2013;8:207–23. [PubMed: 23914755](Review of antidepressant induced liver injury).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, none of which were attributed to sertraline even though it is ranked as one of the top 20 most prescribed medications in Iceland).
- Suen CF, Boyapati R, Simpson I, Dev A. Acute liver injury secondary to sertraline. BMJ Case Rep. 2013;2013:bcr2013201022. pii. [PMC free article: PMC3794285] [PubMed: 24072839](26 year old pregnant woman developed nausea and dark urine 24 weeks after starting and 3 weeks after increasing the dose of sertraline [bilirubin 1.5 mg/dL, ALT 700 U/L, Alk P 113 U/L, INR normal], resolving within 80 days of stopping and subsequent normal delivery).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, only one of which was attributed to an antidepressant [amitriptyline] and none to a MAO inhibitor, SSRI or SNRI).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 20 cases [2%] were attributed to antidepressants including 9 due to SNRIs [7 to duloxetine, 1 each to nefazodone and trazodone], 5 to bupropion, 5 to SSRIs [3 to escitalopram, and 1 each to fluoxetine and sertraline], and only 1 to tricyclics [imipramine]).
- Freiesleben SD, Furczyk K. A systematic review of agomelatine-induced liver injury. J Mol Psychiatry. 2015;3:4. [PMC free article: PMC4407422] [PubMed: 25932327](Review of the literature on liver injury associated with agomelatine therapy concludes that serum ALT levels arise more frequently during agomelatine compared to placebo treatment, but that similar rates of enzyme elevations are found with many other antidepressants).
- Voican CS, Martin S, Verstuyft C, Corruble E, Perlemuter G, Colle R. Liver function test abnormalities in depressed patients treated with antidepressants: a real-world systematic observational study in psychiatric settings. PLoS One. 2016;11:e0155234. [PMC free article: PMC4865191] [PubMed: 27171561](Among 321 psychiatric inpatients, only 116 [36%] had liver tests performed and only 18 during therapy with an antidepressant, 3 of which were suspected to have drug induced liver injury, 1 each with escitalopram, venlafaxine and amitriptyline, all without jaundice and 2 without symptoms, all 3 resolving).
- Friedrich ME, Akimova E, Huf W, Konstantinidis A, Papageorgiou K, Winkler D, Toto S, et al. Drug-induced liver injury during antidepressant treatment: results of AMSP, a drug surveillance program. Int J Neuropsychopharmacol. 2016;19(4):pyv126. pii. [PMC free article: PMC4851269] [PubMed: 26721950](Among 184,234 psychiatric inpatients from 80 hospitals, 149 cases [0.08%] of drug induced liver injury were reported including 22 of 70,060 [0.03%] receiving SSRIs, 71 of 50,201 [0.14%] patients treated with tricyclics and 3 of 3869 receiving MAO inhibitors [0.08%]).
- Gahr M, Zeiss R, Lang D, Connemann BJ, Hiemke C, Schönfeldt-Lecuona C. Drug-Induced liver injury associated with antidepressive psychopharmacotherapy: an explorative assessment based on quantitative signal detection using different MedDRA terms. J Clin Pharmacol. 2016;56:769–78. [PubMed: 26470856](Using data on adverse drug reaction reports from the Uppsala Monitoring Center of WHO, there were higher relative hepatotoxicity reports for nefazodone, agomelatine, many tricyclics and mirtazapine).
- Conrad MA, Cui J, Lin HC. Sertraline-associated cholestasis and ductopenia consistent with vanishing bile duct syndrome. J Pediatr. 2016;169:313–5.e1. [PubMed: 26597434](15 year old developed jaundice and itching 5 months after starting sertraline [bilirubin 8.0 rising to 33.7 mg/dL, ALT 238 U/L, GGT 36], with a delay in stopping until a liver biopsy showed cholestatic hepatitis, slow to resolving, but all tests were normal 4 months later).
- Nicoletti P, Aithal GP, Bjornsson ES, Andrade RJ, Sawle A, Arrese M, Barnhart HX, et al. International Drug-Induced Liver Injury Consortium, Drug-Induced Liver Injury Network Investigators, and International Serious Adverse Events Consortium. Association of liver Injury from specific drugs, or groups of drugs, with polymorphisms in HLA and other genes in a genome-wide association study. Gastroenterology. 2017;152:1078–89. [PMC free article: PMC5367948] [PubMed: 28043905](A genome wide association study done on 862 patients with drug induced liver injury found several associations within the HLA region, most striking was HLA-A*33:01 with an allele frequency of 0.01 in Caucasian controls and 0.02 in drug induced liver injury patients [0.01 with hepatocellular and 0.04 with cholestatic injury], particularly frequent with injury due to ticlopidine [in 4 of 5 cases], methyldopa [2 or 4], fenofibrate [4 of 7], terbinafine [6 of 14], enalapril [2 or 4], sertraline [2 of 5] and erythromycin [2 of 10]).
- Chen VC, Lin CF, Hsieh YH, Liang HY, Huang KY, Chiu WC, Lee Y, McIntyre RS, et al. Hepatocellular carcinoma and antidepressants: a nationwide population-based study. Oncotarget. 2017;8:30464–70. [PMC free article: PMC5444756] [PubMed: 27783998](Among almost 50,000 cases of hepatocellular carcinoma registered in the Taiwan National Health Insurance Research Database, the rate of antidepressant use was lower than in approximately 250,000 matched controls from the database).
- Osorio S, Escudero-Vilaplana V, Reguilón-Gallego L, Gómez-Centurión I, Díez JL, Ferrer-Marín F. Severe liver toxicity in a chronic myeloid leukemia patient probably induced by a drug interaction between imatinib and sertraline. J Oncol Pharm Pract. 2017 Jan 1;:1078155217735689. [Epub ahead of print] [PubMed: 29065786](43 year old man with chronic myelogenous leukemia developed liver injury 4 months after starting imatinib and 5 weeks after starting sertraline [bilirubin 1.0 rising to 10 mg/dL, ALT 791 U/L, Alk P 457 U/L] worsened for 2 weeks despite stopping both drugs and then began to improve; after recovery the leukemia relapsed and he was started on dasatinib without recurrence of liver injury).
- Thébaut A, Habes D, Gottrand F, Rivet C, Cohen J, Debray D, Jacquemin E, et al. Sertraline as an additional treatment for cholestatic pruritus in children. J Pediatr Gastroenterol Nutr. 2017;64:431–5. [PubMed: 27557426](Among 20 children with pruritis due to liver disease treated with sertraline [1-4 mg/kg/day], pruritis improved in 14 who were maintained on therapy long term, while bile acid and bilirubin levels did not change and there were no serious adverse events or mention of worsening of ALT levels or hepatotoxicity).
- Ferrajolo C, Scavone C, Donati M, Bortolami O, Stoppa G, Motola D, Vannacci A, et al. DILI-IT Study Group. Antidepressant-induced acute liver injury: a case-control study in an Italian inpatient population. Drug Saf. 2018;41:95–102. [PubMed: 28770534](Among 179 cases of hospitalizations for unexplained acute liver injury enrolled in an Italian prospective study between 2010 and 2014, 17 had been exposed to antidepressants the major implicated agents being citalopram [n=4], sertraline [n=3], paroxetine [n=3], tricyclics [n=2], trazodone [n=1], fluoxetine [n=1], and duloxetine [n=1]; no MAO inhibitors listed).
- Billioti de Gage S, Collin C, Le-Tri T, Pariente A, Bégaud B, Verdoux H, Dray-Spira R, et al. Antidepressants and hepatotoxicity: a cohort study among 5 million individuals registered in the French National Health Insurance Database. CNS Drugs. 2018;32:673–84. [PMC free article: PMC6061298] [PubMed: 29959758](Among 5 million persons identified in a national French health insurance database who started an antidepressant between 2010 and 2015, 382 developed serious liver injury resulting in hospitalization, rates per 100,0000 persons-years being 19 for SSRIs, 22 venlafaxine, 13 duloxetine, and 33 mirtazapine).
- Chan HL, Chiu WC, Chen VC, Huang KY, Wang TN, Lee Y, McIntyre RS, et al. SSRIs associated with decreased risk of hepatocellular carcinoma: A population-based case-control study. Psychooncology. 2018;27:187–92. [PubMed: 28666060](Analysis of the Taiwan National Health Service Insurance Research Database identified 59,859 patients with initial diagnosis of hepatocellular carcinoma and 285,124 matched controls; SSRI [including sertraline] use was more frequent in the controls than in the HCC cases but only in analyses adjusted for possibly confounding factors).
- Lochmann D, Richardson T. Selective serotonin reuptake inhibitors. Handb Exp Pharmacol. 2019;250:135–44. [PubMed: 30838457](Overview of the SSRIs mentioned that they have similar efficacy in treating depression and similar rates and adverse event profile which largely represents the effects of serotonin excess: nausea, diarrhea, dizziness, somnolence, insomnia, sweating, tremor anxiety, dry mouth, anxiety and restlessness; they can also cause weigh gain and sex dysfunction as well as activate mania and cause withdrawn symptoms).
- Tejedor-Tejada J, García-Pajares F, Madrigal Rubiales B. Hepatobiliary and Pancreatic: Sertraline-induced vanishing bile duct syndrome treated with plasmapheresis. J Gastroenterol Hepatol. 2019;34:488. [PubMed: 30536927](39 year old woman developed jaundice 15 weeks after starting sertraline [bilirubin not given, ALT ~370 U/L, GGT ~220 rising to 920 U/L), biopsy showing bile duct paucity and slow but eventual full recovery after stopping).
- Drugs for anxiety disorders. Med Lett Drugs Ther. 2019;61(1578):121–6. [PubMed: 31386647](Concise review of drugs for anxiety including SSRIs, SNRIs and benzodiazepines including mechanism of action, clinical efficacy, safety and costs; does not mention ALT elevations or hepatotoxicity).
- Drugs for depression. Med Lett Drugs Ther. 2020;62(1592):25–32. [PubMed: 32320387](Concise review of the mechanism of action, clinical efficacy, safety and costs of drugs for depression; hepatotoxicity is mentioned only for nefazodone [now rarely used because of severe hepatotoxicity] and duloxetine [in heavy drinkers]).
- Ueberberg B, Frommberger U, Messer T, Zwanzger P, Kuhn J, Anghelescu I, Ackermann K, Assion HJ. Drug-induced liver injury (DILI) in patients with depression treated with antidepressants: a retrospective multicenter study. Pharmacopsychiatry. 2020;53:60–4. [PubMed: 31958850](Among 329 psychiatric inpatients with depression seen at 6 psychiatric centers in Germany, 17 [5%] had serum aminotransferase elevations but none had clinically apparent liver injury, most commonly implicated drugs included mirtazapine, agomelatine, citalopram and venlafaxine).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Paroxetine.[LiverTox: Clinical and Researc...]Review Paroxetine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Fluvoxamine.[LiverTox: Clinical and Researc...]Review Fluvoxamine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Optimal treatment for obsessive compulsive disorder: a randomized controlled feasibility study of the clinical-effectiveness and cost-effectiveness of cognitive-behavioural therapy, selective serotonin reuptake inhibitors and their combination in the management of obsessive compulsive disorder.[Int Clin Psychopharmacol. 2018]Optimal treatment for obsessive compulsive disorder: a randomized controlled feasibility study of the clinical-effectiveness and cost-effectiveness of cognitive-behavioural therapy, selective serotonin reuptake inhibitors and their combination in the management of obsessive compulsive disorder.Fineberg NA, Baldwin DS, Drummond LM, Wyatt S, Hanson J, Gopi S, Kaur S, Reid J, Marwah V, Sachdev RA, et al. Int Clin Psychopharmacol. 2018 Nov; 33(6):334-348.
- Sertraline and obsessive compulsive disorder: new indication. Limited assessment.[Prescrire Int. 2000]Sertraline and obsessive compulsive disorder: new indication. Limited assessment.. Prescrire Int. 2000 Aug; 9(48):112-3.
- Review Fluoxetine.[LiverTox: Clinical and Researc...]Review Fluoxetine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Sertraline - LiverToxSertraline - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...