NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
The penicillinase-resistant [also referred to as second generation penicillins] are semisynthetic modifications of natural penicillins that are resistant to bacterial enzyme beta-lactamase, which accounts for typical penicillin resistance. The natural penicillins from which the second generation penicillins are made are bactericidal antibiotics naturally derived from the mold, Penicillium chrysogenum. Their basic structure includes a thiazolidine ring connected to a beta-lactam ring with a variable side chain. As a class, the penicillins bind to bacterial proteins and inhibit synthesis of the bacterial cell wall, causing cell lysis particularly in rapidly growing organisms. Bacterial resistance to penicillin is usually mediated by beta-lactamase, an enzyme which destroys the beta-lactam ring of penicillin, rendering it inactive. The penicillinase-resistant penicillins resist the hydrolysis of the beta-lactam ring by the bacterial enzymes. They are active against most organisms that are susceptible to the natural penicillins (although less active than penicillin G) and have extended coverage against resistant forms.
Background
Three major penicillinase-resistant penicillins are available in the United States: dicloxacillin (dye klox" a sil' in), oxacillin (ox" a sil' in) and nafcillin (naf sil' in). Dicloxacillin is orally available; oxacillin and nafcillin have both oral and parenteral formulations, the latter being given by the intramuscular or intravenous route. Other formulations available abroad or in the past include methicillin, cloxacillin and flucloxacillin, which have been associated with a higher frequency of side effects including hepatic injury. The major indications for dicloxacillin, oxacillin and nafcillin are moderate-to-serious infections with susceptible penicillinase-producing staphylococci; these agents are also active against organisms susceptible to natural penicillins, but are less active than the natural penicillins.
Hepatotoxicity
Three forms of liver injury have been attributed to the penicillinase-resistant and other penicillins. The first is a transient and usually asymptomatic elevation in serum aminotransferase levels that occurs with high dose intravenous therapy with oxacillin (Case 1, Oxacillin) and rarely with standard penicillins (Case 1, Penicillin G). This reaction has not been described with nafcillin or dicloxacillin and patients can be safety switched to these or other forms of penicillin in the face of oxacillin injury. This form of penicillin-induced liver injury occurs only with high dose therapy that is likely due to direct hepatotoxicity.
The second form of hepatotoxicity occurs in patients with hypersensitivity reactions to the penicillin (Case 2, Penicillin G). Generally, the liver injury is mild and is overshadowed by the allergic phenomena (rash, fever, facial edema, anaphylaxis). Mild elevations of serum aminotransferase or alkaline phosphatase without jaundice are not uncommon in patients with severe penicillin reactions, and the abnormalities generally resolve rapidly with improvement in the allergic features.
The third form of hepatotoxicity is an idiosyncratic, usually self-limited cholestatic hepatitis that occurs within 1 to 6 weeks of initiation of therapy and is quite rare, described only in single case reports with oxacillin, nafcillin and dicloxacillin (Case 1, nafcillin and Case 1, dicloxacillin). This injury probably represents a class effect and patients who develop idiosyncratic liver injury due to one of the penicillinase-resistant penicillins should avoid other agents in this class. This type of reaction is much more common with flucloxacillin, an agent that is available in Australia and some countries in Europe, but not in the United States. In addition, rare cases of flucloxacillin associated liver injury have resulted in vanishing bile duct syndrome has well as instances of acute liver failure leading to liver transplantation or death. These more serious complications of drug induced liver injury have been less frequent with use of the other penicillinase-resistant penicillins.
The idiosyncratic hepatic injury caused by the second generation penicillins is probably due to hypersensitivity. The role of immunologic pathways in liver injury has been best shown with flucloxacillin, which is strongly associated with the presence of the HLA-B*57:01 allele (which also predicts abacavir hypersensitivity). Immunologic studies have begun to elucidate the reasons for the HLA association and hypersensitivity to abacavir and flucloxacillin, and a similar mechanism possibly underlies the idiosyncratic, typically cholestatic jaundice caused by dicloxacillin and other second generation penicillins. However, the incidence of liver injury due to flucloxacillin and dicloxacillin is rare and is uncommon even among persons with HLA-B*57:01, so that screening for this allele is unlikely to be practicable in preparation of using these antibiotics.
Drug Class: Antiinfective Agents
Dicloxacillin, nafcillin, and oxacillin are discussed separately with individual clinical cases, histology and specific references. General references to the hepatotoxicity of the 2nd generation penicillins and to cloxacillin, methicillin, and flucloxacillin are given below.
The following are links to each drug record:
- Cloxacillin
- Flucloxacillin
- Methicillin
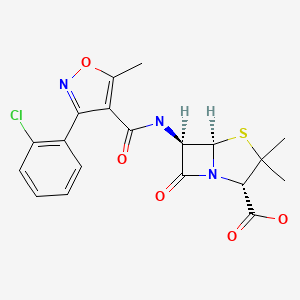
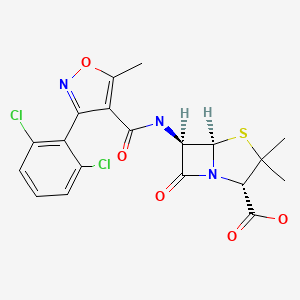
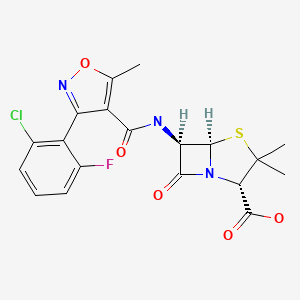
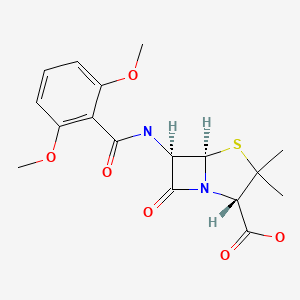
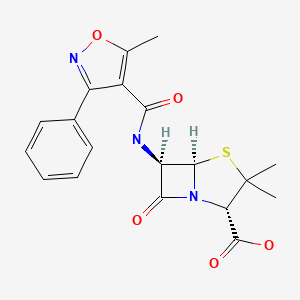
CHEMICAL FORMULAS AND STRUCTURES
ANNOTATED BIBLIOGRAPHY
References updated: 20 October 2020
- Zimmerman HJ. Synthetic penicillins. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999. p. 596-8.(Expert review of penicillins and liver injury published in 1999).
- Moseley RH. Hepatotoxicity of antimicrobials and antifungal agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 463-82.(Review of hepatotoxicity of antibiotics mentions that liver injury from the penicillins is very rare, and is usually cholestatic for the oxypenicillins such as dicloxacillin and cloxacillin).
- MacDougall C. Penicillins, cephalosporins, and other β-lactam antibiotics. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1023-38.(Textbook of pharmacology and therapeutics).
- Freedman MA. Oxacillin—apparent hematologic and hepatic toxicity. Rocky Mt Med J. 1965;62:34–6. [PubMed: 14224480](33 year old woman developed AST elevations to ~220 U/L, atypical lymphocytosis and eosinophilia after 2.5 months of high dose oral oxacillin, complicated by bone marrow suppression and breakthrough in chronic osteomyelitis).
- Pas AT, Quinn EL. Cholestatic hepatitis following the administration of sodium oxacillin. JAMA. 1965;191:674–5. [PubMed: 14242432](65 year old woman developed itching and jaundice the week after stopping a 4 week course of oral oxacillin [bilirubin 2.2 mg/dL, Alk P ~twice elevated, AST 76 U/L], resolving within 8 weeks).
- Dismukes WE. Oxacillin-induced hepatic dysfunction. JAMA. 1973;226:861–3. [PubMed: 4800332](3 cases of ALT elevations, fever and nausea arising 11-24 days after starting high dose intravenous oxacillin therapy, with rapid reversal on stopping).
- Olans RN, Weiner LB. Reversible oxacillin hepatotoxicity. J Pediatr. 1976;89:835–8. [PubMed: 978335](8 instances of ALT elevations [peak values 31-1359 U/L] without jaundice [2 had eosinophilia] after 8-25 days of intravenous oxacillin in children or young adults, with rapid resolution; no recurrence when switched to nafcillin).
- Bruckstein AH, Attia AA. Oxacillin hepatitis. Two patients with liver biopsy, and review of the literature. Am J Med. 1978;64:519–22. [PubMed: 637061](Two injection drug users treated with high dose oxacillin [12-16 g/day] for endocarditis developed increased AST levels [10-40 times ULN], with mild symptoms but no change in Alk P or bilirubin and nonspecific biopsy findings, arising after 2-3 weeks and resolving rapidly with stopping).
- Goldstein LI, Granoff M, Waisman J. Hepatic injury due to oxacillin administration. Am J Gastroenterol. 1978;70:171–4. [PubMed: 717369](21 year old male injection drug used developed aminotransferase elevations [ALT 806 U/L, AST 388 U/L, 15% eosinophils] 20 days after starting intravenous oxacillin [12 g/day], with biopsy showing hepatitis, rapid recovery).
- Onorato IM, Axelrod JL. Hepatitis from intravenous high-dose oxacillin therapy: findings in an adult inpatient population. Ann Intern Med. 1978;89:497–500. [PubMed: 697229](Review of experience with high dose oxacillin revealed 8 cases of liver injury, rising 3-19 days after start of therapy with fever and mild GI symptoms, ALT 2 to 15 times ULN, Alk P minimally increased, and no jaundice; resolving in 1 week; compared to control group, a history of penicillin allergy was given in 3 cases, but not controls).
- D'Angelo LJ. Oxacillin and hepatotoxicity. Ann Intern Med. 1979;90:442. [PubMed: 426429](Letter commenting on article by Onorato & Axelrod, without new data).
- Taylor C, Corrigan K, Steen S, Craig C. Oxacillin and hepatitis. Ann Intern Med. 1979;90:857–8. [PubMed: 434706](Letter in response to Onorato & Axelrod describing 24 year old man who developed ALT elevations [226 U/], with rash and eosinophilia after 27 days of intravenous oxacillin therapy [8 g/day], rapidly resolving upon switching to nafcillin).
- Pollock AA, Berger SA, Simberkoff MS, Rahal JJ Jr. Hepatitis associated with high-dose oxacillin therapy. Arch Intern Med. 1978;138:915–7. [PubMed: 646563](Prospective study of liver tests in 41 patients during intravenous oxacillin therapy; 15 had ALT elevations, but only 5 were attributed to oxacillin, 12-23 g/day arising 5-24 days after starting, peak ALT values 5-20 times ULN, mild Alk P elevation in 4, but normal bilirubin in all, and resolution in 4-16 days of stopping; no eosinophilia, fever or symptoms).
- Halloran TJ, Clague MD. Hepatitis associated with high-dose oxacillin therapy. Arch Intern Med. 1979;139:376–7. [PubMed: 426588](Letter in response to Pollock [1978] describing 16 year old girl with no history of injection drug use who developed AST elevations [peak 140 U/L], starting after 9 days of intravenous oxacillin, rapid resolution upon stopping).
- Enat R, Pollack S, Ben-Arieh Y, Livni E, Barzilai D. Cholestatic jaundice caused by cloxacillin: macrophage inhibition factor test in preventing rechallenge with hepatotoxic drugs. Br Med J. 1980;280:982–3. [PMC free article: PMC1601139] [PubMed: 7417768](69 year old woman developed jaundice 2 weeks after a course of ampicillin and cloxacillin [bilirubin 14.9 mg/dL, AST normal, Alk P ~5 times ULN], with recurrence within 4 days of rechallenge [bilirubin 9.3 mg/dL, ALT normal, Alk P twice ULN], positive macrophage inhibition factor test).
- Williams CN, Malatjalian DA. Severe penicillin-induced cholestasis in a 91-year-old woman. Dig Dis Sci. 1981;26:470–3. [PubMed: 7249889](91 year old woman was given both penicillin G and cloxacillin for 11 days when cholestatic hepatitis arose, bilirubin rising to 24 mg/dL, but recovery in 2 months, most likely due to cloxacillin).
- Lobatto S, Dijkmans BA, Mattie H, Van Hooff JP. Flucloxacillin-associated liver damage. Neth J Med. 1982;25:47–8. [PubMed: 7070561](63 year old woman on renal dialysis had mild ALT elevation [twice ULN] after a few days of intravenous floxacillin and cloxacillin, with positive rechallenge to oral flucloxacillin [ALT rose from 14 to 74 U/L within 1 day]).
- Nahata MC, DeBolt SL, Powell DA. Adverse effects of methicillin, nafcillin and oxacillin in pediatric patients. Dev Pharmacol Ther. 1982;4:117–23. [PubMed: 7172968](Prospective study of children treated with intravenous methicillin [28], nafcillin [32] or oxacillin [8]; minimal ALT elevations occurred in 1 on nafcillin and 1 on oxacillin; no jaundice).
- Miller WI, Souney PF, Chang JT. Hepatic dysfunction following nafcillin and cephalothin therapy in a patient with a history of oxacillin hepatitis. Clin Pharm. 1983;2:465–8. [PubMed: 6627877](Mild ALT elevations after 13 days of high dose oxacillin [18 g/day], similar increase after nafcillin and again with cephalosporin in a male injection drug user with probable chronic hepatitis C, which might have accounted for ALT fluctuations).
- Bengtsson F, Florén CH, Hägerstrand I, Söderström C, Aberg T. Flucloxacillin-induced cholestatic liver damage. Scand J Infect Dis. 1985;17:125–8. [PubMed: 3992199](2 cases of cholestatic hepatitis of moderate severity arising 4-5 weeks after starting oral cloxacillin, resolution in 6-8 weeks).
- Tauris P, Jørgensen NF, Petersen CM, Albertsen K. Prolonged severe cholestasis induced by oxacillin derivatives. A report on two cases. Acta Med Scand. 1985;217:567–9. [PubMed: 4025011](2 case reports: 65 year old man with osteomyelitis developed jaundice and pruritus 6 weeks after starting flucloxacillin [bilirubin ~10 mg/dL, AST 1.5 times ULN, Alk P 3 times ULN], biopsy showing cholestasis, resolving within 8 weeks of stopping; 21 year old man with osteomyelitis developed jaundice 9 weeks after starting dicloxacillin [bilirubin ~4 mg/dL, AST 119 U/L, Alk P 814 U/L], resolving within 6 weeks of stopping).
- Aderka D, Livni E, Salamon F, Weinberger A, Pinkhas J. Use of macrophage inhibition factor and mast-cell degranulation tests for diagnosis of cloxacillin-induced cholestasis. Am J Gastroenterol. 1986;81:1084–6. [PubMed: 3776960](58 year old man took 10 days of cloxacillin and developed jaundice 3 days later [peak bilirubin 18.7 mg/dL, ALT 450 U/L, Alk P 436 IU, no eosinophilia]; had positive macrophage inhibition factor and mast cell degranulation tests in response to cloxacillin).
- Kleinman MS, Presberg JE. Cholestatic hepatitis after dicloxacillin-sodium therapy. J Clin Gastroenterol. 1986;8:77–8. [PubMed: 3701014](56 year old man developed jaundice and pruritus 2-3 weeks after a 5 day course of dicloxacillin [bilirubin rising to 13 mg/dL, AST 225 U/L, Alk P 318 U/L], without rash, eosinophilia or fever, requiring 10 weeks to resolve).
- Konikoff F, Alcalay J, Halevy J. Cloxacillin-induced cholestatic jaundice. Am J Gastroenterol. 1986;81:1082–3. [PubMed: 3776959](77 year old woman developed fever and pruritus 5 days after starting oral cloxacillin [bilirubin 3.6 mg/dL, AST 97 U/L, Alk P 497 U/L], resolving within 5 weeks; history revealed a similar response to a previous course of oral cloxacillin, thus explaining the short latency period).
- Deboever G. Cholestatic jaundice due to derivatives of oxacillin. Am J Gastroenterol. 1987;82:483. [PubMed: 3578231](Letter in response to Konikoff [1986] describing 75 year old woman with cholestatic hepatitis [bilirubin 12.8 mg/dL, ALT 57 U/L, Alk P 868 U/L] arising 3 days after starting flucloxacillin, resolving in 2 months).
- Victorino RM, Maria VA, Correia AP, de Moura C. Floxacillin-induced cholestatic hepatitis with evidence of lymphocyte sensitization. Arch Intern Med. 1987;147:987–9. [PubMed: 3579450](45 year old man developed prolonged cholestatic hepatitis arising 15 days after starting oral floxacillin [bilirubin rising from 11 to 40.6 mg/dL, ALT 490 U/L, Alk P 171 U/L], ultimately responding to prednisone therapy).
- [Risk of liver reactions after treatment with flucloxacillin] Lakartidningen 1989; 86: 977-8. Swedish. [PubMed: 2927200]
- Turner IB, Eckstein RP, Riley JW, Lunzer MR. Prolonged hepatic cholestasis after flucloxacillin therapy. Med J Aust. 1989;151:701–5. [PubMed: 2593915](5 cases of cholestatic hepatitis arising after stopping flucloxacillin, latency 13-35 days [bilirubin 13.3-38.2 mg/dL, ALT 85-525 U/L, Alk P 263-1580 U/L], with prolonged jaundice and abnormal liver tests still present 4-9 months later).
- Miros M, Kerlin P, Walker N, Harris O. Flucloxacillin induced delayed cholestatic hepatitis. Aust N Z J Med. 1990;20:251–3. [PubMed: 2372276](6 cases of cholestatic hepatitis 17-28 days after starting flucloxacillin, with prolonged course and 3 who still had marked Alk P elevations 6 months later).
- Pascual J, Orofino L, Marcén R, Quereda C, Ortuño J. Cloxacillin-induced cholestasis in a renal allograft patient with chronic hepatitis. Am J Gastroenterol. 1990;85:335–6. [PubMed: 2106780](Man with renal transplant and advanced chronic hepatitis C developed sudden onset of itching and worsening of jaundice [bilirubin rising from 4.1 to 22 mg/dL] 3 days after starting intravenous cloxacillin [8 grams/day], with rapid reversal on stopping).
- Fairley CK, Boyd I, Purcell P, McNeil J. Flucloxacillin jaundice. Lancet. 1992;339:679. [PubMed: 1347364](Letter describing increase use of flucloxacillin in Australia [from 12,136 in 1986 to 1,000,000 prescriptions yearly in 1990] and increasing adverse events reported [from 4 in 1987 to 64 in 1990]; worldwide, 255 hepatic adverse events reported).
- Lestico MR, Vick KE, Hetsko CM. Hepatic and renal dysfunction following nafcillin administration. Ann Pharmacother. 1992;26:985–90. [PubMed: 1504413](Four cases of elevations in creatinine, BUN and bilirubin within 4 days of starting iv nafcillin, but most patients had abnormal liver tests before therapy; minimal change in AST and Alk P and all patients were septic and also received rifampin and/or gentamicin).
- Olsson R, Wiholm BE, Sand C, Zettergren L, Hultcrantz R, Myrhed M. Liver damage from flucloxacillin, cloxacillin and dicloxacillin. J Hepatol. 1992;15:154–61. [PubMed: 1506634](54 year old woman developed prolonged cholestasis [peak bilirubin 24 mg/dL] after an 18 day course of flucloxacillin leading to cirrhosis and liver transplantation 7 years later; possibly vanishing bile duct syndrome. In a review of Swedish adverse drug reaction reports, 77 flucloxacillin cases were found between 1981-90 compared to only 16 for dicloxacillin and 9 for cloxacillin, fever and eosinophilia in half, mostly cholestatic and mixed enzymes, occasional hepatocellular, older age was a risk factor).
- Derby LE, Jick H, Henry DA, Dean AD. Cholestatic hepatitis associated with flucloxacillin. Med J Aust. 1993;158:596–600. [PubMed: 8479374](Survey of 600 general practices in the UK with 132,087 patients who received flucloxacillin, 10 cases of unexplained cholestatic liver injury <45 days [mean~4 weeks] afterwards compared to 3 cases after tetracycline; estimated risk was 7.6 per 100,000 users).
- Jick H, Derby LE, Dean AD, Henry DA. Flucloxacillin and cholestatic hepatitis. Med J Aust. 1994;160:525. [PubMed: 8170433](Follow up of study by Derby et al.; risk of flucloxacillin cholestatic hepatitis in a new cohort was 6.5 per 100,000 users, with a rate similar to their previous estimate).
- Eckstein RP, Dowsett JF, Lunzer MR. Flucloxacillin induced liver disease: histopathological findings at biopsy and autopsy. Pathology. 1993;25:223–8. [PubMed: 8265236](Liver histology from 13 cases of flucloxacillin induced liver injury from Australia; ages 37-83 years given flucloxacillin for 5-23 days, onset 7-21 after stopping, mostly cholestatic; histology showed intrahepatic cholestasis, no granulomas, bile ductular injury, 3 of 4 with prolonged course had ductopenia).
- Fairley CK, McNeil JJ, Desmond P, Smallwood R, Young H, Forbes A, Purcell P, et al. Risk factors for development of flucloxacillin associated jaundice. BMJ. 1993;306:233–5. [PMC free article: PMC1676728] [PubMed: 8443520](Review of cases from the Australia adverse drug reaction system tracing 51 cases and 199 controls; injury was associated with older age, longer therapy, concomitant drugs, but not alcohol, smoking, gender or other drug allergies).
- Mazuryk H, Kastenberg D, Rubin R, Muñoz SJ. Cholestatic hepatitis associated with the use of nafcillin. Am J Gastroenterol. 1993;88:1960–2. [PubMed: 8237951](80 year old developed pruritus and rash after 2 weeks of intravenous nafcillin [8 g/day], with subsequent jaundice [bilirubin rising from 5.7 to 15 mg/dL, ALT 117 U/L, Alk P 1,102 U/L; after month of jaundice, prednisone was started with prompt improvement).
- Siegmund JB, Tarshis AM. Prolonged jaundice after dicloxacillin therapy. Am J Gastroenterol. 1993;88:1299–300. [PubMed: 8338117](36 year old woman developed fatigue and jaundice 3 weeks after starting dicloxacillin [bilirubin 18.2 mg/dL, ALT 100 U/L, Alk P 312 U/L], with slow recovery even with prednisone; 3 years later, enzymes were still mildly elevated [ALT 44 U/L, Alk P 188 U/L]).
- Koek GH, Stricker BH, Blok AP, Schalm SW, Desmet VJ. Flucloxacillin-associated hepatic injury. Liver. 1994;14:225–9. [PubMed: 7997079](Description of 11 cases of flucloxacillin hepatotoxicity reported to Dutch Adverse Events Center over 10 years, onset in 10-30 days, cholestatic in 7, mixed in 3; 2 patients died; the rest resolved in an average of 10 weeks).
- Saliba B, Herbert PN. Oxacillin hepatotoxicity in HIV-infected patients. Ann Intern Med. 1994;120:1048. [PubMed: 8185140](Retrospective review found that 81% [9/11] of HIV-positive, but only 4.5% [3/66] of HIV-negative patients receiving iv oxacillin for more than 10 days developed ALT or AST >3 fold elevated).
- Desmond PV. Flucloxacillin hepatitis--an Australian epidemic. Aust N Z J Med. 1995;25:195–6. [PubMed: 7487684](Review of Australian experience with flucloxacillin, their most common cause of drug induced liver disease; average age 58 years, onset 16 days after stopping, chronic cholestasis frequent; fatality rate 5%).
- Devereaux BM, Crawford DH, Purcell P, Powell LW, Roeser HP. Flucloxacillin associated cholestatic hepatitis. An Australian and Swedish epidemic? Eur J Clin Pharmacol. 1995;49:81–5. [PubMed: 8751026](Review of literature and history of use and pattern and frequency of hepatic injury from flucloxacillin in Australia, Sweden and UK).
- Pillans PI. Drug associated hepatic reactions in New Zealand: 21 years experience. N Z Med J. 1996;109:315–9. [PubMed: 8816722](Flucloxacillin ranked 6th as a cause of liver adverse drug reaction in New Zealand in 1990s).
- Presti ME, Janney CG, Neuschwander-Tetri BA. Nafcillin-associated hepatotoxicity. Report of a case and review of the literature. Dig Dis Sci. 1996;41:180–4. [PubMed: 8565754](63 year old developed jaundice after 5 days of intravenous nafcillin [bilirubin rising to 40 mg/dL, ALT ~210 U/L, Alk P ~375 U/L], lasting 2 months, previous history of dicloxacillin allergy-rash).
- Saab S, Venkataramani A, Yao F. Possible granulomatous hepatitis after dicloxacillin therapy. J Clin Gastroenterol. 1996;22:163–4. [PubMed: 8742666](74 year old developed rash 5 days after starting oral dicloxacillin [bilirubin 0.5 mg/dL, ALT 172 U/L, Alk P 183 U/L], biopsy showing a single granuloma and mild nonspecific changes, ultimately resolving within 4 months of stopping).
- Goland S, Malnick SD, Gratz R, Feldberg E, Geltner D, Sthoeger ZM. Severe cholestatic hepatitis following cloxacillin treatment. Postgrad Med J. 1998;74:59–60. [PMC free article: PMC2360792] [PubMed: 9538497](77 year old woman developed fever, rash and jaundice 2 weeks after stopping a 2 week course of cloxacillin and ofloxacin with bilirubin 12.9 mg/dL, ALT 144 U/L, Alk P 394 U/L; after a month of jaundice, prednisone introduced with prompt improvement).
- Al-Homaidhi H, Abdel-Haq NM, El-Baba M, Asmar BI. Severe hepatitis associated with oxacillin therapy. South Med J. 2002;95:650–2. [PubMed: 12081223](6 year old girl developed fever, abdominal pain and marked ALT elevation [peak 2,257 U/L] with normal Alk P and bilirubin [0.3 mg/dL] after 14 days of intravenous oxacillin, resolving within 3 weeks of stopping).
- Trevenzoli M, Cattelan AM, Mencarelli R, Meneghetti F. Severe hepatitis associated with oxacillin therapy. South Med J. 2003;96:324–5. [PubMed: 12659378](Letter in response to Al-Homaidhi [2002] describing 33 year old who developed liver injury [bilirubin 1.8 mg/dL, ALT 2440 U/L, Alk P 103 U/L] weeks after receiving a 4 day course of amoxicillin/clavulanate [not oxacillin as suggested by the title]).
- Ibáñez L, Pérez E, Vidal X, Laporte JR. Grup d'Estudi Multicènteric d'Hepatotoxicitat Aguda de Barcelona (GEMHAB). Prospective surveillance of acute serious liver disease unrelated to infectious, obstructive, or metabolic diseases: epidemiological and clinical features, and exposure to drugs. J Hepatol. 2002;37:592–600. [PubMed: 12399224](Survey of 107 cases of acute serious liver disease, not due to viruses, found no instances of drug induced liver injury due to penicillinase-resistant penicillins).
- Maraqa NF, Gomez MM, Rathore MH, Alvarez AM. Higher occurrence of hepatotoxicity and rash in patients treated with oxacillin, compared with those treated with nafcillin and other commonly used antimicrobials. Clin Infect Dis. 2002;34:50–4. [PubMed: 11731945](Retrospective analysis of laboratory tests from 222 children receiving outpatient parenteral oxacillin, nafcillin, clindamycin or other antibiotics found 12 cases of anicteric and self-limited hepatotoxicity, 9 [22%] from oxacillin, all hepatocellular with normal bilirubin, onset in 6-43 days, resolution in 1-3 weeks; none to nafcillin; 1 clindamycin, 1 ceftriaxone and 1 ampicillin/sulbactam/gentamicin).
- Sgro C, Clinard F, Ouazir K, Chanay H, Allard C, Guilleminet C, Lenoir C, et al. Incidence of drug-induced hepatic injuries: a French population-based study. Hepatology. 2002;36:451–5. [PubMed: 12143055](A population based study identified 34 cases of acute drug induced liver injury over a 3 year period, including 10 [25%] due to antibiotics; one was due to cloxacillin with a 5 day latency, mixed serum enzyme pattern and recovery within 2 weeks of stopping).
- Björnsson E, Jerlstad P, Bergqvist A, Olsson R. Fulminant drug-induced hepatic failure leading to death or liver transplantation in Sweden. Scand J Gastroenterol. 2005;40:1095–101. [PubMed: 16165719](Analysis of all fatal adverse drug event reports of liver injury in Sweden between 1966 and 2002, found 103 cases; most common causes were halothane [n=16], acetaminophen [14], flucloxacillin [9], and TMP-SMZ [6]).
- Dobson JL, Angus PW, Jones R, Crowley P, Gow PJ. Flucloxacillin-induced aplastic anaemia and liver failure. Transpl Int. 2005;18:487–9. [PubMed: 15773973](40 year old woman developed aplastic anemia and acute liver failure starting 4 weeks after starting 2 week course of flucloxacillin, reversed by liver transplantation).
- Hussaini SH, O'Brien CS, Despott EJ, Dalton HR. Antibiotic therapy: a major cause of drug-induced jaundice in southwest England. Eur J Gastroenterol Hepatol. 2007;19:15–20. [PubMed: 17206072](Review of causes of non-obstructive jaundice in 347 patients presenting between 1998 and 2004 at a single UK center, 28 were thought to be drug induced liver injury [8.1%] and antibiotics were the most common cause, 32% amoxicillin/clavulanate, 25% flucloxacillin, 18% other).
- Lee CY, Chen PY, Huang FL, Chi CS. Reversible oxacillin-associated hepatitis in a 9-month old boy. J Paediatr Child Health. 2008;44:146–8. [PubMed: 18307421](9 month old boy given intravenous oxacillin for septic arthritis for 8 days when he developed lethargy and marked elevations in ALT [1568 U/L], with normal Alk P and bilirubin and resolving within 10 days of switching to teicoplanin).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected from 2004 to 2008, antimicrobials accounted for 45% of cases with 23 single agent cases due to amoxicillin/clavulanate, 13 nitrofurantoin, 10 fluoroquinolones, 9 macrolides, 9 sulfonamides, 5 cephalosporins, 3 oxacillin, 2 doxycycline, 2 amoxicillin, and one each for gentamicin, imipenem, and clindamycin, but none from dicloxacillin or nafcillin).
- Devarbhavi H, Dierkhising R, Kremers WK, Sandeep MS, Karanth D, Adarsh CK. Single-center experience with drug-induced liver injury from India: causes, outcome, prognosis, and predictors of mortality. Am J Gastroenterol. 2010;105:2396–404. [PubMed: 20648003](313 cases of drug induced liver injury were seen over a 12 year period at a large hospital in Bangalore, India; leading causes were antituberculosis agents [58%], anticonvulsants [11%] and NSAIDs [2%]; specific antibiotic agents included sulfamethoxazole/ trimethoprim [2%] and amoxicillin-clavulanate [1%]).
- Ferrajolo C, Capuano A, Verhamme KMC, Schuemie M, Rossi F, Stricker BH, Sturkenboom CJM. Drug-induced hepatic injury in children: a case/non-case study of suspected adverse drug reactions in VigiBase. Br J Clin Pharmacol. 2010;70:721–8. [PMC free article: PMC2997312] [PubMed: 21039766](Among 624,673 adverse drug reports in children in a worldwide pharmacovigilance database, 6595 [1%] were for hepatic injury and antibacterials accounted for 11%, those with the highest adjusted odds ratios being aztreonam, erythromycin, ceftriaxone and minocycline; no mention of penicillins).
- Li L, Jick H, Jick SS. Updated study on risk of cholestatic liver disease and flucloxacillin. Br J Clin Pharmacol. 2009;68:269–70. [PMC free article: PMC2767292] [PubMed: 19694748](Analysis of UK General Practice Research Database showed risk of cholestatic liver disease within 45 days of first time use of flucloxacillin was stable between 1985-2007 [6.1-8.5/100,000 users compared to 0.3/100,000 users of penicillin V]).
- Daly AK, Donaldson PT, Bhatnagar P, Shen Y, Pe'er I, Floratos A, Daly MJ, et al. HLA-B*5701 genotype is a major determinant of drug-induced liver injury due to flucloxacillin. Nature Genetics. 2009;41:816–9. [PubMed: 19483685](Genome-wide association study [GWAS] in 51 cases of flucloxacillin liver injury and 285 controls found an association with a single nucleotide polymorphism linked to HLA-B*5701 [84% in cases vs 5% in controls], the same genotype associated with abacavir hypersensitivity; ~0.2% of persons with this HLA type receiving flucloxacillin develop cholestatic hepatitis, making it likely that other genes or factors are important as well).
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury including 66 due to antimicrobial agents, but none were attributed to a penicillinase-resistant penicillin).
- Leitner JM, Graninger W, Thalhammer F. Hepatotoxicity of antibacterials: pathomechanisms and clinical data. Infection. 2010;38:3–11. [PubMed: 20107858](Review of hepatotoxicity of antibiotics, mentions that cholestatic hepatitis has been reported with many beta-lactams and beta-lactamases inhibitors).
- Daly AK. Genome-wide association studies in pharmacogenomics. Nat Rev Genet. 2010;11:241–6. [PubMed: 20300088](Review of recent advances in GWAS studies of pharmacokinetics and adverse drug reactions and association of flucloxacillin injury with HLA-B*5701).
- Robles M, Toscano E, Cotta J, Lucena MI, Andrade RJ. Antibiotic-induced liver toxicity: mechanisms, clinical features and causality assessment. Curr Drug Saf. 2010;5:212–22. [PubMed: 20210729](Review of antibiotic hepatotoxicity mentions that flucloxacillin is the second most common cause of liver injury in many countries).
- Alam MB, Kadoura A, Sathaiah M. A fatal case of nafcillin-induced hepatotoxicity: a case report and the literature review. Case Rep Med. 2012;2012:953714. [PMC free article: PMC3403404] [PubMed: 22844299](53 year old woman developed jaundice 15 days after starting intravenous nafcillin for osteomyelitis [bilirubin 9.6 mg/dL, ALT 24 U/L, Alk P 388 U/L], with worsening despite stopping nafcillin [bilirubin 28.7 mg/dL, ALT 24 U/L, Alk P >1884 U/L], and death from multiorgan failure 2 months later).
- Urban TJ, Goldstein DB, Watkins PB. Genetic basis of susceptibility to drug-induced liver injury: what have we learned and where do we go from here? Pharmacogenomics. 2012;13:735–8. [PMC free article: PMC3641893] [PubMed: 22594502](Editorial summarizing recent advances in studies on the genetics of drug induced liver injury including the association of flucloxacillin injury with HLA-B*57:01).
- Monshi MM, Faulkner L, Gibson A, Jenkins RE, Farrell J, Earnshaw CJ, Alfirevic A, et al. Human leukocyte antigen (HLA)-B*57:01-restricted activation of drug-specific T cells provides the immunological basis for flucloxacillin-induced liver injury. Hepatology. 2013;57:727–39. [PubMed: 22987284](T cells from persons with HLA-B*57:01 were activated when exposed to dendritic cells presenting flucloxacillin bound to albumin, and were similarly activated by oxacillin, cloxacillin and dicloxacillin).
- Sistanizad M, Peterson GM. Drug-induced liver injury in the Australian setting. J Clin Pharm Ther. 2013;38:115–20. [PubMed: 23350857](Among 17 persons with suspected drug induced liver injury seen over at 12 month period at a referral hospital in Tasmania, 11 were attributed to antibiotics including 4 to flucloxacillin, 2 amoxicillin with clavulanate, 2 amoxicillin, and 1 each to rifampin, moxifloxacin and ciprofloxacin).
- Wuillemin N, Adam J, Fontana S, Krähenbühl S, Pichler WJ, Yerly D. HLA haplotype determines hapten or p-i T cell reactivity to flucloxacillin. J Immunol. 2013;190:4956–64. [PubMed: 23596311](Analysis of T cell responses in persons with and without HLA-B*57:01 suggested a pharmacological interaction of flucloxacillin with immune receptors on T cells, underlies the HLA association with flucloxacillin hepatoxicity).
- Vera JH, Naous N, Mackie N, Winston A, Cooke G. The safety of flucloxacillin in HIV-infected patients with positive HLA-B*5701 genotype. AIDS. 2013;27:484–5. [PubMed: 23032409](Among 10 persons with HIV infection with HLA-B*57:01 who received a course of flucloxacillin, none developed evidence of liver injury, suggesting that it is safe to use in this population of HLA-tested individuals).
- Phillips EJ, Mallal SA. HLA-B*5701 and flucloxacillin associated drug-induced liver disease. AIDS. 2013;27:491–2. [PubMed: 23291545](Letter in response to Vera [2013] arguing that the positive predictive value of HLA-B*5701 is only 0.12%, making screening an inefficient means of avoiding flucloxacillin hepatotoxicity and accounting for their negative findings because of the few patients tested).
- Kaniwa N, Saito Y. Pharmacogenomics of severe cutaneous adverse reactions and drug-induced liver injury. J Hum Genet. 2013;58:317–26. [PubMed: 23635947](Review of genetic studies of severe cutaneous and hepatic adverse events; HLA DRB*5701 has been associated with flucloxacillin hepatotoxicity, mainly in Europeans [Daly 2009]).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, including 36 [37%] due to antibiotics and specifically dicloxacillin in 1 of 22,320 patients treated and cloxacillin in 1 of 3659 patients treated).
- Wuillemin N, Terracciano L, Beltraminelli H, Schlapbach C, Fontana S, Krähenbühl S, Pichler WJ, et al. T cells infiltrate the liver and kill hepatocytes in HLA-B(*)57:01-associated floxacillin-induced liver injury. Am J Pathol. 2014;184:1677–82. [PubMed: 24731753](Analysis of T cells from HLA-B*57:01 positive, healthy, non-flucloxacillin exposed controls demonstrated cytotoxicity of their CD8 cells by exposure to increasing concentrations of flucloxacillin with HLA-linked target cells).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury from Latin American countries published between 1996 and 2012 identified 176 cases, of which 37 [19%] were attributed to antimicrobials, but none to penicillinase resistant penicillins such as oxacillin or dicloxacillin).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 323 cases [36%] were attributed to antibiotics 3 of which were due to oxacillin, all being self-limited episodes of aminotransferase elevations without jaundice; no instances of dicloxacillin or nafcillin associated liver injury).
- Yaseen FS, Saide K, Kim SH, Monshi M, Tailor A, Wood S, Meng X, et al. Promiscuous T-cell responses to drugs and drug-haptens. J Allergy Clin Immunol. 2015;136:474–6.e8. [PubMed: 25910715](T cell clones from patients with flucloxacillin induced liver injury are HLA-restricted and are activated by via a hapten mechanism, unlike T cells clones from HLA-allele matched healthy controls which are activated by the native drug).
- Ramírez A, Abril JC, Cano J. DRESS syndrome due to antibiotic therapy of osteoarticular infections in children: two case reports. Rev Esp Cir Ortop Traumatol. 2015;59:360–4. [PubMed: 25052739](2 children, aged 7 with septic arthritis and age 8 with osteomyelitis, developed fever and rash 7 and 16 days after starting cefotaxime and cloxacillin [ALT 55 and 281 U/L, bilirubin and Alk P not provided], resolving within 3 weeks of stopping antibiotics).
- Faulkner L, Gibson A, Sullivan A, Tailor A, Usui T, Alfirevic A, Pirmohamed M, et al. Detection of primary T cell responses to drugs and chemicals in HLA-typed volunteers: implications for the prediction of drug immunogenicity. Toxicol Sci. 2016;154:416–29. [PubMed: 27637899](Demonstration of T cell priming to drugs linked with specific class I HLA-alleles).
- Nicoletti P, Aithal GP, Bjornsson ES, Andrade RJ, Sawle A, Arrese M, Barnhart HX, et al. International Drug-Induced Liver Injury Consortium, Drug-Induced Liver Injury Network Investigators, and International Serious Adverse Events Consortium. Association of liver injury from specific drugs, or groups of drugs, with polymorphisms in HLA and other genes in a genome-wide association study. Gastroenterology. 2017;152:1078–89. [PMC free article: PMC5367948] [PubMed: 28043905](A genome wide association study done on 862 patients with drug induced liver injury demonstrated a strong link with HLA-A*33:01 in patients with cholestatic liver injury, particularly in cases attributed to terbinafine, fenofibrate and ticlopidine).
- Usui T, Naisbitt DJ. Human leukocyte antigen and idiosyncratic adverse drug reactions. Drug Metab Pharmacokinet. 2017;32:21–30. [PubMed: 28017537](Review of the association of specific forms of idiosyncratic drug reactions and HLA alleles focusing on class I alleles linked with abacavir [B*57:01], allopurinol [B*58:01], carbamazepine [B*15:02], amoxicillin/clavulanate [A*02:01], and flucloxacillin [B*57:01]).
- Rao Q, Schuster I, Seoud T, Zarrabi K, Goolsarran N. A patient with nafcillin-associated drug-induced liver failure. Case Rep Gastroenterol. 2017;11:564–8. [PMC free article: PMC5636993] [PubMed: 29033779](68 year old man with osteomyelitis developed jaundice 4 weeks after starting intravenous nafcillin, 2 g every 4 hours [bilirubin 9.4 rising to 14.1 mg/dL, ALT 127 U/L, Alk P 311 U/L, INR 1.6, eosinophils 21%], worsening for 7 days after stopping, but then resolving and 6 months later had normal liver tests).
- Wing K, Bhaskaran K, Pealing L, Root A, Smeeth L, van Staa TP, Klungel OH, et al. Quantification of the risk of liver injury associated with flucloxacillin: a UK population-based cohort study. J Antimicrob Chemother. 2017;72:2636–46. [PMC free article: PMC5890755] [PubMed: 28859440](Among 861,962 individuals given a first prescription of flucloxacillin and followed for the next 45 days in the UK Clinical Practice Research Datalink, 122 developed symptoms of jaundice [14.2 per 100,000 or ~1 in 7000] and 73 had laboratory confirmed liver injury [8.5 per 100,000 or ~1 in 12,000], and rates were higher with consecutive prescriptions and in older age groups).
- Visentin M, Lenggenhager D, Gai Z, Kullak-Ublick GA. Drug-induced bile duct injury. Biochim Biophys Acta Mol Basis Dis. 2018;1864 4 Pt B:1498–506. [PubMed: 28882625](Review of drug induced bile duct injury focusing on agents flucloxacillin and amoxicillin/clavulanate that injure small ducts and fluorouracil [given by hepatic artery], ketamine, scolicidal agents [for Hydatid disease given into the cysts] that injure larger ducts causing a sclerosing cholangitis like picture).
- Lavergne A, Vigneau C, Polard E, Triquet L, Rioux-Leclercq N, Tattevin P, Golbin L. Acute kidney injury during treatment with high-dose cloxacillin: a report of 23 cases and literature review. Int J Antimicrob Agents. 2018;52:344–9. [PubMed: 29665445](Among 23 patients with suspected cloxacillin induced renal dysfunction [19 had also received gentamicin], the median age was 75, duration of therapy 4 days, dose 12 gm daily and peak creatinine 3.8 mg/dL, all resolving after stopping therapy; 8 patients had abnormal liver tests but no details provided).
- Takeuchi Y, Shinozaki T, Kumamaru H, Hiramatsu T, Matsuyama Y. Analyzing intent-to-treat and per-protocol effects on safety outcomes using a medical information database: an application to the risk assessment of antibiotic-induced liver injury. Expert Opin Drug Saf. 2018;17:1071–9. [PubMed: 30252549](Cohort matching of cases with vs without antibiotic therapy in a large electronic medical record database from the University of Tokyo Hospital from 2011 to 2015 with adjustments, found rates of liver test abnormalities within 30 days of starting penicillins [25.2 per 1000] were higher than that of fluoroquinolones [11.4] and macrolide antibiotics [8.1] as well as controls [6.5 to 7.1]).
- Cirulli ET, Nicoletti P, Abramson K, Andrade RJ, Bjornsson ES, Chalasani N, Fontana RJ, et al. Drug-Induced Liver Injury Network (DILIN) investigators. International DILI consortium (iDILIC). A missense variant in PTPN22 is a risk factor for drug-induced liver injury. Gastroenterology. 2019;156:1707–1716.e2. [PMC free article: PMC6511989] [PubMed: 30664875](Genome-wide association studies on 2048 patients with drug induced liver injury and 12,439 controls identified a variant in PTPN22 which was highly associated with liver injury, allele frequency being 0.12 among cases and 0.08 among controls with highest association in Northern Europeans and in cases of amoxicillin clavulanate, PTPN22 being a cellular kinase involved in modulation of immune reactions).
- Nicoletti P, Aithal GP, Chamberlain TC, Coulthard S, Alshabeeb M, Grove JI, Andrade RJ, et al. International Drug-Induced Liver Injury Consortium. (iDILIC). Drug-induced liver injury due to flucloxacillin: relevance of multiple human leukocyte antigen alleles. Clin Pharmacol Ther. 2019;106:245–53. [PubMed: 30661239](Among 197 patients with flucloxacillin induced liver injury, the allele frequency for HLA-B*57:01 was 0.42 compared to 0.04 among population controls and HLA-B*57:03, although rare was also significantly associated with allele frequency of 0.005 compared to 0.0003 in controls, both B*57 alleles sharing a valine at position 97 of the HLA protein).
- Hashim A, Barnabas A, Miquel R, Agarwal K. Successful liver transplantation for drug-induced vanishing bile duct syndrome. BMJ Case Rep. 2020;13:e233052. [PMC free article: PMC7035849] [PubMed: 31948982](63 year old man developed jaundice shortly after completing a 10 day course of flucloxacillin which worsened over the next 3 months [bilirubin 29.3 mg/dL, ALT 60 U/L, Alk P 229 U/L, INR 1.0], liver biopsy showing bland cholestasis and rare bile duct loss, eventually undergoing successful liver transplant 6 months after presentation; genetic testing revealed homozygosity for a BSEP [ABC B11] mutation which may have contributed to the poor outcome).
- Teixeira M, Macedo S, Batista T, Martins S, Correia A, Matos LC. Flucloxacillin-induced hepatotoxicity - association with HLA-B*5701. Rev Assoc Med Bras. 2020;66(1):12–7. [PubMed: 32130375](74 year old man developed abdominal pain 2 weeks after a second 8 day course of flucloxacillin [bilirubin 3.3 rising to 24.1 mg/dL, ALT 646 U/L, Alk P 302 U/L, GGT 662 U/L] with persistence of jaundice for 3 months and abnormalities of Alk P and GGT for more than a year; HLA testing revealed B*57:01, an allele often associated with flucloxacillin liver injury).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Flucloxacillin, a new isoxazolyl penicillin, compared with oxacillin, cloxacillin, and dicloxacillin.[Br Med J. 1970]Flucloxacillin, a new isoxazolyl penicillin, compared with oxacillin, cloxacillin, and dicloxacillin.Sutherland R, Croydon EA, Rolinson GN. Br Med J. 1970 Nov 21; 4(5733):455-60.
- Relationship between penicillinase production and the in-vitro activity of methicillin, oxacillin, cloxacillin, dicloxacillin, flucloxacillin, and cephalothin against strains of Staphylococcus aureus of different phage patterns and penicillinase activity.[J Antimicrob Chemother. 1986]Relationship between penicillinase production and the in-vitro activity of methicillin, oxacillin, cloxacillin, dicloxacillin, flucloxacillin, and cephalothin against strains of Staphylococcus aureus of different phage patterns and penicillinase activity.Frimodt-Møller N, Rosdahl VT, Sørensen G, Hartzen SH, Bentzon MW. J Antimicrob Chemother. 1986 Jul; 18(1):27-33.
- Comparison of oral penicillinase-resistant penicillins: contrasts between agents and assays.[South Med J. 1982]Comparison of oral penicillinase-resistant penicillins: contrasts between agents and assays.Bass JW, Bruhn FW, Merritt WT, Suttle DE, Jirka JH, Mesrobian RB, Berkenbaugh JT. South Med J. 1982 Apr; 75(4):408-10.
- Review Frequency of drug-induced liver injury in children receiving anti-staphylococcal penicillins.[J Antimicrob Chemother. 2022]Review Frequency of drug-induced liver injury in children receiving anti-staphylococcal penicillins.Tang K, Coombs S, Gwee A. J Antimicrob Chemother. 2022 Nov 28; 77(12):3221-3230.
- Review Antimicrobial spectrum, pharmacology and therapeutic use of antibiotics. Part 2: penicillins.[Am J Hosp Pharm. 1977]Review Antimicrobial spectrum, pharmacology and therapeutic use of antibiotics. Part 2: penicillins.Barza M. Am J Hosp Pharm. 1977 Jan; 34(1):57-67.
- Penicillins (2nd Generation) - LiverToxPenicillins (2nd Generation) - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...