NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Labetalol is an antihypertensive agent with both alpha- and beta-adrenergic receptor blocking activity. Labetalol has been linked to several cases of clinically apparent drug induced liver disease, some of which have been severe and even fatal.
Background
Labetalol (la bayt' a lol) is a unique antihypertensive agent that has both alpha- and beta-adrenergic receptor blocking activity. The beta-blockade is nonselective, acting on both beta-1 and beta-2 adrenergic receptors. Beta-1 adrenergic blockade reduces the heart rate and myocardial contractility by slowing the AV conduction and suppressing automaticity. Beta-2 blockade affects peripheral vascular resistance and can cause bronchospasm and hypoglycemia. The alpha blockade is largely directed at the alpha-1 receptors and leads to relaxation of arterial smooth muscle and vasodilation. Labetalol was approved for use in the United States in 1984 and currently more than 2 million prescriptions are filled yearly. Current indications for labetalol are in the therapy of hypertension alone or in combination with other agents. Parenteral forms of labetalol are indicated for therapy of hypertensive emergencies, severe hypertension and pheochromocytoma. Labetalol is available in tablets of 100, 200 and 300 mg in generic formulations and under the trade name Trandate. Parenteral formulations for intravenous administration are also available. The typical oral dose of labetalol in adults is 100 mg twice daily initially with subsequent dose adjustments based upon clinical response and tolerance to a range of 200 to 1200 mg daily. Common side effects include bradycardia, hypotension, fatigue, dizziness, orthostatic hypotension, depression, memory loss, impotence, weight gain and diarrhea. As with all beta-blockers, sudden withdrawal can trigger rebound hypertension.
Hepatotoxicity
Labetalol therapy has been associated with mild-to-moderate elevations of serum aminotransferase levels in up to 8% of patients, a rate far higher than with other beta-blockers. These elevations, however, are usually transient, not associated with symptoms, and can resolve even with continuation of therapy. Idiosyncratic, clinically apparent liver injury from labetalol is rare, but several instances have been reported as isolated case reports as well as in case series. The liver injury typically arises after 4 to 16 weeks of therapy and the pattern of serum enzyme elevations is usually hepatocellular with an acute hepatitis-like onset and course. Immunoallergic features (rash, fever, eosinophilia) are uncommon as is autoantibody formation. While most cases resolve rapidly once labetalol is stopped, there have been several instances of acute liver failure and death or need for emergency liver transplantation associated with labetalol use, particularly if there is a delay in its discontinuation. Labetalol is the beta-blocker with the highest apparent risk for causing clinically apparent liver injury.
Likelihood score: C (probable although rare cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism of labetalol hepatic injury is unknown, but it believed to be due to metabolic idiosyncratic disposition of the agent, which is known to be extensively metabolized in the liver. There is little evidence for hypersensitivity as the cause of injury but it is likely to be due to an idiosyncractic rather than an intrinsic reaction.
Outcome and Management
Severity ranges from minimal and transient ALT elevations to clinically apparent acute hepatitis with jaundice to acute liver failure and death or need for liver transplantation. No instances of chronic hepatic injury or vanishing bile duct syndrome attributable to labetalol have been reported. Rechallenge is usually followed by recurrence of liver injury and should be avoided. There is little information on whether there is cross reactivity of the liver injury with other beta-blockers and patients who are switched to other agents should be carefully monitored.
References to the safety and potential hepatotoxicity of labetalol are provided in the overview on Beta-Adrenergic Receptor Antagonists, last updated June 2019.
Drug Class: Beta-Adrenergic Receptor Antagonists
CASE REPORT
Case 1. Labetalol induced acute liver injury.
[Modified from: Douglas DD, Yang RD, Jensen P, Thiele DL. Fatal labetalol-induced hepatic injury. Am J Med 1989; 87: 235-6. PubMed Citation]
A 63 year old woman developed nausea and dark urine approximately 3 months after starting labetalol (200 mg daily) for hypertension. She had no previous history of liver disease, jaundice, or risk factors for viral hepatitis. She was not taking any other medications and denied alcohol abuse. Laboratory testing showed serum bilirubin of 3.6 mg/dL and serum enzyme elevations typical of acute hepatitis (Table). She was negative for serological markers for hepatitis A and B. No diagnosis was made, and she was given another prescription for labetalol, but evidently stopped taking it on her own. Over the next few weeks she recovered, but was then lost to follow up for at least 6 months. When seen again, she had normal liver tests and was hypertensive. Labetalol was restarted. Two months later she developed anorexia and the following month presented with jaundice and serum bilirubin of 3.1 mg/dL. Labetalol was stopped and she was monitored closely. Tests for viral hepatitis were again negative as were routine autoantibodies. Abdominal ultrasound showed gallstones, but no evidence of biliary obstruction. There was mild ascites. Her liver condition worsened, and she developed progressive hepatic failure and died approximately 6 weeks after stopping labetalol for the second time. Autopsy showed a shrunken liver with extensive multilobular collapse with broad bands of fibrosis.
Key Points
| Medication: | Labetalol (200 mg daily) |
| Pattern: | Hepatocellular (R=23) |
| Severity: | 2+ (initially); 5+ (upon reexposure); fatal |
| Latency: | 3 months |
| Recovery: | 1 month after initial episode |
| Other medications: | None |
Laboratory Values
| Weeks After Starting | Weeks After Stopping | AST* (U/L) | Alk P* (U/L) | Bilirubin* (mg/dL) | Other |
|---|---|---|---|---|---|
| 0 (pre) | 0 | 11 | 92 | 0.3 | |
| 12 | 0 | 1253 | 205 | 3.6 | Labetolol stopped |
| 14 | 2 weeks | 247 | 150 | 1.5 | |
| 16 | 4 weeks | 37 | 111 | 0.4 | |
| Patient was lost to follow up for 6 months | |||||
| 0 | 0 | 13 | 117 | 0.3 | Labetalol restarted |
| 13 | 0 | 1007 | 172 | 3.1 | |
| 16 | 3 | 582 | 283 | 9.5 | |
| 17 | 4 | 402 | 315 | 11.3 | |
| 18 | 5 | 303 | 321 | 12.0 | |
| 19 | 6 | 225 | 266 | 16.8 | Death from liver failure |
| Normal Values | <40 | <110 | <1.2 | ||
* Converted from μKat/L and μmol/L.
Comment
This patient developed an acute hepatitis-like clinical picture 3 months after starting labetalol. Despite the lack of a suitable diagnosis, labetalol was not discontinued, although the patient evidently stopped taking it on her own and did not return for further management of her hypertension. When seen 6 months later, labetalol was restarted and a similar clinical syndrome arose 2 to 3 months later, but with a progressive and ultimately fatal course. Labetalol has been implicated in at least a dozen cases of acute liver injury with a predominantly hepatocellular pattern of enzyme elevations, a latency period of 2 to 16 weeks, and fatal outcome or emergency liver transplantation in several instances. In contrast, most cases of clinically apparent liver injury due to other beta-blockers have had a somewhat shorter latency period (2 to 12 weeks) and a milder course and outcome. Acute liver injury has also been described with dilevolol, which is one of the 4 stereoisomers of labetalol that has predominantly beta-adrenergic blocking activity.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Labetalol – Generic, Trandate®
DRUG CLASS
Beta-Adrenergic Receptor Antagonists
Product labeling at DailyMed, National Library of Medicine, NIH
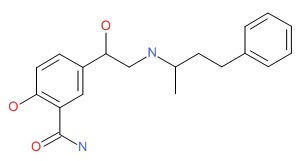
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Labetalol | 36894-69-6 | C19-H24-N2-O3 |
 |
- PubChem SubstanceRelated PubChem Substances
- Review Properties of labetalol, a combined alpha- and beta-blocking agent, relevant to the treatment of myocardial ischemia.[Cardiovasc Drugs Ther. 1988]Review Properties of labetalol, a combined alpha- and beta-blocking agent, relevant to the treatment of myocardial ischemia.Frishman WH. Cardiovasc Drugs Ther. 1988 Sep; 2(3):343-53.
- Review Combined alpha- and beta-receptor inhibition in the treatment of hypertension.[Drugs. 1984]Review Combined alpha- and beta-receptor inhibition in the treatment of hypertension.Prichard BN. Drugs. 1984; 28 Suppl 2:51-68.
- Synthesis and comparison of some cardiovascular properties of the stereoisomers of labetalol.[J Med Chem. 1982]Synthesis and comparison of some cardiovascular properties of the stereoisomers of labetalol.Gold EH, Chang W, Cohen M, Baum T, Ehrreich S, Johnson G, Prioli N, Sybertz EJ. J Med Chem. 1982 Nov; 25(11):1363-70.
- Labetalol: an alpha- and beta-adrenoceptor blocking drug.[Ann Intern Med. 1983]Labetalol: an alpha- and beta-adrenoceptor blocking drug.Michelson EL, Frishman WH. Ann Intern Med. 1983 Oct; 99(4):553-5.
- Review Current status of labetalol, the first alpha- and beta-blocking agent.[Int J Clin Pharmacol Ther Toxi...]Review Current status of labetalol, the first alpha- and beta-blocking agent.Kanto JH. Int J Clin Pharmacol Ther Toxicol. 1985 Nov; 23(11):617-28.
- Labetalol - LiverToxLabetalol - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...