NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Lacosamide is an amino acid derivative with a unique anticonvulsant activity that is used in combination with other agents as therapy of partial onset seizures. Lacosamide therapy is associated with a low rate of transient serum enzyme elevations and has been linked to rare instances of clinically apparent liver injury.
Background
Lacosamide (la koe' sa mide) is a functionalized amino acid derivative that appears to act by slow inactivation of voltage gated sodium channels in the central nervous system, which decreases the rate of neurotransmission and diminishes rapid, repetitive neuronal firing. Lacosamide was approved for use as an anticonvulsant in the United States in 2011 and current indications are for its use in partial-onset seizures in patients 4 years of age or above either alone or in combination with other anti-epileptic agents. Lacosamide is available in tablets of 50, 100, 150 and 200 mg under the brand name Vimpat. It is also available in solution as for oral (10 mg/mL) use and in an intravenous form (200 mg in single-use 20 mL vials) for short term use in adults when oral administration. The typical dose is 50 mg twice daily initially, with subsequent dose increases to an average of 200 to 400 mg daily. Side effects may include headache, dizziness, ataxia, blurred vision, nausea, fatigue and tremor.
Hepatotoxicity
In prelicensure clinical trials, addition of lacosamide to standard anticonvulsant therapy was reported to be associated with ALT elevations above 3 times the upper limit of normal (ULN) in 7 of 935 patients (0.7%) compared to none of 356 treated with placebo. A single case of hepatitis with jaundice during lacosamide therapy was also reported. Since approval, there have been rare isolated reports of clinically apparent liver injury associated with lacosamide used, but the clinical features suggested that hepatic ischemia or other anticonvulsants combined with lacosamide may have been responsible. The onset was within a few days to several months after starting and the presentation was with a hepatocellular pattern of serum enzyme elevations, one case being asymptomatic and mild and the other severe. In both instances, there was rapid recovery.
Likelihood score: D (possible rare cause of clinically apparent liver injury)
Mechanism of Injury
Lacosamide is metabolized by the liver, largely by CYP 2C19, 2C9 and 3A4, but has not been reported to have clinically significant drug interactions. Approximately 40% is excreted unchanged in the urine, and the metabolites of lacosamide are inactive. The mechanism of hepatic injury from lacosamide is not known, but may relate to a toxic or immunogenic metabolite.
Outcome and Management
There is no information on the possible cross sensitivity to hepatotoxicity between lacosamide and other anticonvulsants, but its structure suggests that it would not have shared sensitivity to liver injury.
Drug Class: Anticonvulsants
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Lacosamide – Vimpat®
DRUG CLASS
Anticonvulsants
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Lacosamide | 175481-36-4 | C13-H18-N2-O3 |
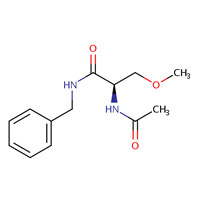 |
ANNOTATED BIBLIOGRAPHY
References updated: 20 March 2019
- Zimmerman HJ. Anticonvulsants. In, Zimmerman, HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999: pp. 498-516.(Expert review of anticonvulsants and liver injury published in 1999 before the availability of lacosamide).
- Pirmohamed M, Leeder SJ. Anticonvulsant agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013: pp 423-42.(Review of anticonvulsant induced liver injury; lacosamide is not discussed).
- Smith MD, Metcalf CS, Wilcox KS. Pharmacotherapy of the epilepsies. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, p. 303-326.(Textbook of pharmacology and therapeutics).
- Ben-Menachem E, Biton V, Jatuzis D, Abou-Khalil B, Doty P, Rudd GD. Efficacy and safety of oral lacosamide as adjunctive therapy in adults with partial-onset seizures. Epilepsia 2007; 48: 1308-17. [PubMed: 17635557](Among 418 adults with poorly controlled, partial onset seizures treated with 1 of 3 doses of lacosamide or placebo for 18 weeks, there was a dose related decrease in seizure activity; 2 patients [0.5%] had ALT elevations above 3 times ULN [124 and 203 U/L], without symptoms or bilirubin elevations and both rapidly returning to normal).
- Björnsson E. Hepatotoxicity associated with antiepileptic drugs. Acta Neurol Scan 2008; 118: 281-90. [PubMed: 18341684](Review of the hepatotoxicity of anticonvulsants; no discussion of lacosamide).
- Wymer JP, Simpson J, Sen D, Bongardt S; Lacosamide SP742 Study Group. Efficacy and safety of lacosamide in diabetic neuropathic pain: an 18-week double-blind placebo-controlled trial of fixed-dose regimens. Clin J Pain 2009; 25: 376-85. [PubMed: 19454870](Among 370 patients with diabetic neuropathy treated with placebo or 1 of 3 doses of lacosamide for 12 weeks, common side effects of dizziness, nausea, fatigue, headache and tremor were dose related and “laboratory variables were generally unremarkable”, although abnormal liver tests were recorded in some patients).
- Halász P, Kälviäinen R, Mazurkiewicz-Beldzińska M, Rosenow F, Doty P, Hebert D, Sullivan T; SP755 Study Group. Adjunctive lacosamide for partial-onset seizures: Efficacy and safety results from a randomized controlled trial. Epilepsia 2009; 50: 443-53. [PubMed: 19183227](Among 485 patients with uncontrolled partial onset seizures who received lacosamide [200 or 400 mg daily] or placebo, side effects were more common with drug and included dizziness, diplopia, nausea, vertigo and fatigue, and no patient had an ALT elevation above 3 times ULN and a bilirubin of 2.0 concurrently).
- Shaibani A, Biton V, Rauck R, Koch B, Simpson J. Long-term oral lacosamide in painful diabetic neuropathy: a two-year open-label extension trial. Eur J Pain 2009; 13: 458-63. [PubMed: 18619874](Among 69 patients with diabetic neuropathy treated with lacosamide [100 to 400 mg daily] for up to 2.5 years in an extension treatment trial, laboratory values overall “were generally unremarkable”).
- Bauer S, David Rudd G, Mylius V, Hamer HM, Rosenow F. Lacosamide intoxication in attempted suicide. Epilepsy Behav 2010; 17: 549-51. [PubMed: 20171144](27 year old woman took an overdose of her anticonvulsants including 12 g of lacosamide, 56 g of gabapentin, 2 g of topiramate and 2.8 g of zonisamide with subsequent coma, rebound seizures and aspiration pneumonia, but ultimate recovery; no mention of ALT elevations or liver injury).
- Chung S, Sperling MR, Biton V, Krauss G, Hebert D, Rudd GD, Doty P; SP754 Study Group. Lacosamide as adjunctive therapy for partial-onset seizures: a randomized controlled trial. Epilepsia 2010; 51: 958-67. [PubMed: 20132285](Among 405 patients with partial onset seizures given lacosamide or placebo as adjunctive therapy for 12 weeks, results of clinical laboratory tests did not identify "any changes that appeared to be associated with lacosamide”; 2 patients had ALT elevations above 3 times ULN, but they were transient and asymptomatic).
- Ziegler D, Hidvégi T, Gurieva I, Bongardt S, Freynhagen R, Sen D, Sommerville K; Lacosamide SP743 Study Group. Efficacy and safety of lacosamide in painful diabetic neuropathy. Diabetes Care 2010; 33: 839-41. [PMC free article: PMC2845038] [PubMed: 20067958](Among 355 patients with diabetic neuropathy treated with lacosamide [400 or 600 mg daily] or placebo for 18 weeks, reduction in pain scores was greater with drug, and adverse events included dizziness, fatigue, nausea, vertigo and headache, but “changes in laboratory variables…revealed no issues of clinical concern”).
- Casas-Fernández C, Martínez-Bermejo A, Rufo-Campos M, Smeyers-Durá P, Herranz-Fernández JL, Ibáñez-Micó S, Campistol-Plana J, et al. Efficacy and tolerability of lacosamide in the concomitant treatment of 130 patients under 16 years of age with refractory epilepsy: a prospective, open-label, observational, multicenter study in Spain. Drugs R D 2012; 12: 187-97. [PMC free article: PMC3585895] [PubMed: 23193979](Among 160 children [6 months to 16 years old] given adjunctive lacosamide therapy for refractory epilepsy for 3 months, “there were no alterations in conventional laboratory tests”).
- Husain A, Chung S, Faught E, Isojarvi J, McShea C, Doty P. Long-term safety and efficacy in patients with uncontrolled partial-onset seizures treated with adjunctive lacosamide: results from a Phase III open-label extension trial. Epilepsia 2012; 53: 521-8. [PubMed: 22372628](In an open label, extension study, 208 patients were treated with lacosamide for up to 5 years; no mention of ALT elevations or hepatotoxicity and “no clinically relevant pattern of change was observed in median or mean…clinical chemistry values”).
- Gutiérrez-Grobe Y, Bahena-Gonzalez JA, Herrera-Gomar M, Mendoza-Diaz P, García-López S, González-Chon O. Acute liver failure associated with levetiracetam and lacosamide combination treatment for unspecified epileptic disorder. Case Rep Emerg Med 2013; 2013: 634174. [PMC free article: PMC3762071] [PubMed: 24027645](22 year old woman developed uncontrollable seizures 2 months after starting levetiracetam and lacosamide and was admitted with acute liver failure [bilirubin 2.1 rising to 20 mg/dL, ALT 4341 U/L, Alk P 74 U/L, INR not given], with requirement for ventilator and hepatic assist support but ultimate recovery, enzymes falling to normal within 12 days; the liver injury perhaps due to hepatic ischemia from status epilepticus).
- Gaitatzis A, Sander JW. The long-term safety of antiepileptic drugs. CNS Drugs 2013; 27: 435-55. [PubMed: 23673774](Review of the long term safety and adverse event profile of anticonvulsants mentions that valproate and felbamate can cause liver failure, but does not mention hepatotoxicity of other anticonvulsants).
- Verrotti A, Loiacono G, Pizzolorusso A, Parisi P, Bruni O, Luchetti A, Zamponi N, et al. Lacosamide in pediatric and adult patients: comparison of efficacy and safety. Seizure 2013; 22: 210-6. [PubMed: 23298605](Among 108 patients with uncontrolled epilepsy who received with adjunctive lacosamide therapy for up to 1 year, overall results of clinical laboratory tests “did not reveal any changes associated with lacosamide treatment”).
- Drugs for epilepsy. Treat Guidel Med Lett 2013; 11: 9-18. [PubMed: 23348233](Concise review of indications and side effects of anticonvulsants; lacosamide is approved as add-on therapy of adults with partial seizures; discussion of adverse effects does not mention hepatotoxicity).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 2013; 144: 1419-25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, but none of the 96, none were attributed to lacosamide).
- Rosenfeld W, Fountain NB, Kaubrys G, Ben-Menachem E, McShea C, Isojarvi J, Doty P; SP615 Study Investigators. Safety and efficacy of adjunctive lacosamide among patients with partial-onset seizures in a long-term open-label extension trial of up to 8 years. Epilepsy Behav 2014; 41: 164-70. [PubMed: 25461210](Among 370 patients enrolled in a long term study [up to 8 years] of adjunctive lacosamide therapy of partial onset seizures, the safety profile was similar to that in controlled trials and therapy was not associated with changes in clinical chemistry results “that were considered clinically relevant”).
- Pasha I, Kamate M, Didagi SK. Efficacy and tolerability of lacosamide as an adjunctive therapy in children with refractory partial epilepsy. Pediatr Neurol 2014; 51: 509-14. [PubMed: 25266613](Among 79 children with refractory seizures on adjunctive therapy with lacosamide, “overall results of clinical laboratory tests…did not reveal any changes during lacosamide treatment”).
- Biton V, Gil-Nagel A, Isojarvi J, Doty P, Hebert D, Fountain NB. Safety and tolerability of lacosamide as adjunctive therapy for adults with partial-onset seizures: Analysis of data pooled from three randomized, double-blind, placebo-controlled clinical trials. Epilepsy Behav 2015; 52 (Pt A): 119-27. [PubMed: 26414341](Combined analysis of 1308 patients with partial onset seizures who received adjunctive therapy with lacosamide or placebo in 3 randomized controlled trials, common side effects were dizziness [31%], nausea [11%] and diplopia [11%], while ALT elevations above 3 times ULN occurred in 0.5% of lacosamide vs 0% of placebo recipients, and 4 patients were withdrawn from treatment because of liver test abnormalities, although no patient was reported as having a hepatic related serious adverse event).
- Zadeh WW, Escartin A, Byrnes W, Tennigkeit F, Borghs S, Li T, Dedeken P, De Backer M; SP0954 Study Group. Efficacy and safety of lacosamide as first add-on or later adjunctive treatment for uncontrolled partial-onset seizures: A multicentre open-label trial. Seizure 2015; 31: 72-9. [PubMed: 26362380](Among 456 patients with uncontrolled partial onset seizures who received adjunctive lacosamide therapy for 24 weeks, no “consistent or clinically relevant effect” was seen on laboratory results).
- Giráldez BG, Toledano R, García-Morales I, Gil-Nagel A, López-González FJ, Tortosa D, Ojeda J, Serratosa JM. Long-term efficacy and safety of lacosamide monotherapy in the treatment of partial-onset seizures: A multicenter evaluation. Seizure 2015; 29: 119-22. [PubMed: 26076854](Retrospective analysis of 66 patients with partial onset seizures treated with lacosamide alone for an average of 15 months found two-thirds were seizure free and side effects were usually mild, only 3 patients being withdrawn from treatment for side effects, none of which were related to ALT elevations or liver injury).
- Sunwoo JS, Byun JI, Lee SK. A case of lacosamide-induced hepatotoxicity. Int J Clin Pharmacol Ther 2015; 53: 471-3. [PubMed: 25907173](22 year old woman with refractory epilepsy developed nausea and abdominal pain within a few days of adding lacosamide to her anticonvulsant regimen of zonisamide and clobazam [bilirubin normal, ALT 299 rising to 635 U/L, Alk P 169 rising to 188 U/L], with rapid recovery upon stopping lacosamide).
- Baulac M, Rosenow F, Toledo M, Terada K, Li T, De Backer M, Werhahn KJ, et al. Efficacy, safety, and tolerability of lacosamide monotherapy versus controlled-release carbamazepine in patients with newly diagnosed epilepsy: a phase 3, randomised, double-blind, non-inferiority trial. Lancet Neurol 2017; 16: 43-54. [PubMed: 27889312](Among 888 patients with epilepse at 185 medical centers treated with titrated doses of lacosamide or controlled release carbamazepine twice daily, 74% on lacosamide and 70% on carbamazepine remained seizure free while serious adverse events arose in 7% vs 10%, withdrawal due to adverse events in 11% vs 16%, and ALT elevations in 10% vs 19%; no mention of clinically apparent hepatotoxicity although 2 patients on carbamazepine developed DRESS syndrome).
- Vossler DG, Wechsler RT, Williams P, Byrnes W, Therriault S; ALEX-MT study group. Long-term exposure and safety of lacosamide monotherapy for the treatment of artial-onset (focal) seizures: Results from a multicenter, open-label trial. Epilepsia 2016; 57: 1625-33. [PubMed: 27528101](Among 322 patients with focal seizures treated with lacosamide, 258 for more than 1 year and 216 for 2 years, common adverse events were dizziness [27%], headache [17%] and nausea [14%] and "there was no evidence of any clinically relevant effect of lacosamide treatment on laboratory parameters").
- Vidaurre J, Gedela S, Yarosz S. Antiepileptic drugs and liver disease. Pediatr Neurol 2017; 77: 23-36. [PubMed: 29097018](Review of the use of anticonvulsants in patients with liver disease recommends use of agents that have little hepatic metabolism such as levetiracetam, lacosamide, topiramate, gabapentin and pregabalin, lacosamide being a good choice because of linear pharmacokinetics, only partial hepatic metabolism, with inactive metabolites and lack of clinically significant CYP450 interactions).
- Misra UK, Dubey D, Kalita J. Comparison of lacosamide versus sodium valproate in status epilepticus: A pilot study. Epilepsy Behav 2017; 76: 110-3. (Among 66 patients wtih status epilepticus not responding to benzodiazepines treated with lacosamide or valproate intravenously, 24-hour control of seizures was more frequent with lacosamide [67% vs 46%] and adverse event rates were similar, but ALT elevations occurred only in those on valproate [n=6:18%] with peak values of. [PubMed: 28919386]128 to 918 U/L and accompanying bilirubin elevations in two [1.8 and 3.2 mg/dL]).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 40 [4.5%] were attributed to anticonvulsants, but none to lacosamide).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Eslicarbazepine.[LiverTox: Clinical and Researc...]Review Eslicarbazepine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Lacosamide: an adjunctive agent for partial-onset seizures and potential therapy for neuropathic pain.[Ann Pharmacother. 2009]Review Lacosamide: an adjunctive agent for partial-onset seizures and potential therapy for neuropathic pain.Harris JA, Murphy JA. Ann Pharmacother. 2009 Nov; 43(11):1809-17. Epub 2009 Oct 20.
- Review Lacosamide: a review of its use as adjunctive therapy in the management of partial-onset seizures.[CNS Drugs. 2013]Review Lacosamide: a review of its use as adjunctive therapy in the management of partial-onset seizures.Hoy SM. CNS Drugs. 2013 Dec; 27(12):1125-42.
- Review Rufinamide.[LiverTox: Clinical and Researc...]Review Rufinamide.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Acute liver failure associated with levetiracetam and lacosamide combination treatment for unspecified epileptic disorder.[Case Rep Emerg Med. 2013]Acute liver failure associated with levetiracetam and lacosamide combination treatment for unspecified epileptic disorder.Gutiérrez-Grobe Y, Bahena-Gonzalez JA, Herrera-Gomar M, Mendoza-Diaz P, García-López S, González-Chon O. Case Rep Emerg Med. 2013; 2013:634174. Epub 2013 Aug 20.
- Lacosamide - LiverToxLacosamide - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...