NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Information
Vancomycin is a broad spectrum antibiotic that has activity against methicillin-resistant strains of Staphylococcus aureus and is generally reserved for serious drug resistant gram-positive infections. Vancomycin therapy has been linked many to instances of hypersensitivity with fever, rash and eosinophilia that can be associated with mild hepatic injury, but has only rarely been associated with severe or life-threatening liver injury.
Background
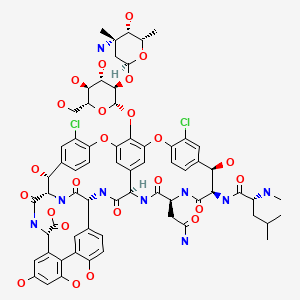
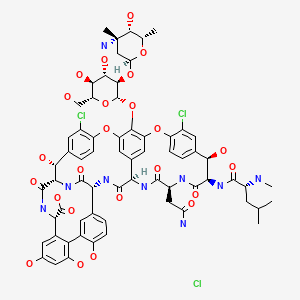
Vancomycin (van" koe mye' sin) is a glycopeptide antibiotic produced by Streptococcus orientalis with primary activity against gram positive bacteria. Vancomycin has a large, complex and unusual structure and is believed to act by inhibition of bacterial cell wall synthesis via binding to the cell wall precursor molecules. Vancomycin is active against, and its major use is in therapy of, infections due to methicillin-resistant Staphylococcus aureus (MRSA), including antibiotic-induced pseudomembranous colitis, staphylococcal enterocolitis, bacterial endocarditis, and sepsis. Vancomycin is not well absorbed orally and for systemic infections it is given intravenously. It is frequently used in combination with other antibiotics and started before bacterial sensitivity results are available. For localized or nonsystemic infections, other routes of administration are used, including oral, rectal, topical, inhalational, intrathecal, intraperitoneal, and intraventricular. The recommended parenteral dosage in adults is 500 mg iv every 6 hours or 1000 mg every 12 hours, with modification to achieve a therapeutic range as needed. The recommended oral dosage in the treatment of antibiotic induced pseudomembranous enterocolitis is 125 to 500 mg every 6 hours for 7 to 10 days. Vancomycin is available generically and under several commercial names including Vancoled, Vancor, Lyphocin, and Vancocin in 125 and 250 mg pulvules and as power for injection or oral administration. Vancomycin was first approved for use in the United States in 1958 and it continues to be widely used, particularly with the recent rise in incidence of serious MRSA infections. Vancomycin is largely well tolerated; common side effects include diarrhea, nausea, nephrotoxicity and neutropenia. Uncommon but potentially severe adverse reactions include infusion reactions, flushing reactions, anaphylaxis, nephrotoxicity, ototoxicity, hypersensitivity reactions including Stevens-Johnson syndrome, and drug reactions with rash, eosinophilia and systemic symptoms (DRESS syndrome).
Hepatotoxicity
Intravenous vancomycin is associated with minor, transient and asymptomatic elevations in serum aminotransferase levels in 1% to 5% of patients, but similar or minimally lower rates of abnormalities are usually reported with comparative agents. In rare instances, the serum enzyme elevations are more marked and may be associated with mild symptoms, although usually without jaundice. In recent years, vancomycin has been linked to hypersensitivity reactions, including Stevens-Johnson syndrome, toxic epidermal necrolysis and the distinctive syndrome of drug reaction, eosinophilia and systemic symptoms (DRESS). These forms of hypersensitivity generally arise within a few days to 3 to 4 weeks after initiation of intravenous (iv) vancomycin therapy. Fever and severe skin rash generally dominate the clinical presentation, but systemic symptoms can include renal, respiratory or heart failure, neutropenia, thrombocytopenia, and liver injury. Cases of DRESS syndrome associated with vancomycin are often accompanied by serum enzyme elevations (Case 1), but marked elevations, symptoms and jaundice are uncommon. The usual systemic features of vancomycin induced DRESS syndrome are renal rather than liver injury but features of hypersensitivity are usually more prominent than organ-specific injury. Nevertheless, in rare instances the liver injury can be severe (Case 2) and result in hepatic failure and death. Patients who receive intravenous vancomycin often have multiple comorbidities including sepsis and receive multiple antibiotics which make the attribution of the hypersensitivity reactions and liver injury with vancomycin difficult. Other more well-known causes of DRESS syndrome include allopurinol, sulfonamides, and the aromatic anticonvulsants. These other causes of DRESS syndrome are more likely to be associated with clinically apparent and even fatal liver injury.
Vancomycin is also associated with several forms of acute infusion reactions, most notably anaphylaxis and the vancomycin flushing reaction, previously known as “red man syndrome”. Vancomycin flushing reactions occur typically during the first 15 to 20 minutes of an initial infusion of vancomycin, most commonly when given rapidly and in relative high doses (1000 mg given over less than 60 minutes). The reaction is characterized by flushing, erythema, and itching usually of the face, neck and upper torso, sometimes accompanied by chest and back pain and variable degrees of hypotension. Rarely, flushing reactions have been associated with oral vancomycin therapy, particularly in elderly patients with active colitis and renal dysfunction. The cause of the symptoms is probably the acute degranulation of mast cells by the direct effect of vancomycin or S. Aureus toxins. The mediator of the reaction is histamine and other active amines or components in mast cell granules. Plasma histamine levels are usually elevated in persons with vancomycin flushing reactions, but the correlation of changes in plasma histamine levels and severity of symptoms is poor. Nevertheless, the symptoms of the vancomycin flushing reaction can be prevented or ameliorated by pretreatment with antihistamines. Perhaps a better approach is the use of slower infusion rates and lower doses of vancomycin. Liver injury is not a feature of vancomycin flushing reactions but can arise secondarily in cases with prolonged or severe hypotension.
Likelihood score: B (highly likely cause of clinically apparent liver injury usually in association with DRESS syndrome).
Mechanism of Injury
Vancomycin is rapidly excreted in the urine without significant hepatic metabolism, which perhaps explains the lack of significant direct hepatotoxicity. Hypersensitivity probably accounts for the instances of mild anicteric hepatitis associated with DRESS syndrome and Stevens-Johnson syndrome due to intravenous vancomycin. Case series have recently shown a close association of vancomycin induced DRESS syndrome with the HLA allele A*32:01, which was detected in 83% of vancomycin induced DRESS syndrome cases but only 6% of population controls. Interestingly, this allele was not associated with cases of Stevens-Johnson syndrome related to vancomycin. The association of ALT elevations and the vancomycin flushing reaction with oral vancomycin is surprising in view of its lack of oral absorption, but the presence of active colitis may allow for some systemic exposure.
Outcome and Management
In published cases, the hepatic injury has usually been self-limited, but rare instances of acute liver failure in the context of hypersensitivity reactions have been linked to vancomycin therapy. Vancomycin should be discontinued promptly in patients who develop immunoallergic features. Corticosteroids are often used to treat the systemic hypersensitivity and relapse may occur when they are discontinued early. In general, spontaneous recovery is usually slow despite early discontinuation of vancomycin, while corticosteroids generally result in rapid resolution. There is no evidence for cross sensitivity to hypersensitivity reactions to vancomycin with other antibiotics, except in some instances for teicoplanin, a vancomycin-like antibiotic available in some countries, but not the United States.
Drug Class: Antiinfective Agents
Other Drugs in the Subclass, Glycopeptide Antibiotics: Dalbavancin, Oritavancin, Telavancin
CASE REPORT
Case 1. DRESS Syndrome without jaundice due to intravenous vancomycin therapy.(1)
A 64 year old man with diabetes, severe obesity, hyperlipidemia, asthma and depression developed DRESS syndrome have receiving intravenous vancomycin for an infected hematoma, a complication of bilateral hernia repair. The patient had a long history of obesity and at one point was found to have serum ALT elevations which were attributed to nonalcoholic fatty liver. After bilateral hernia repair operation he developed a local hematoma that became infected and was treated with intravenous vancomycin (1.5 to 2 mg daily) and piperacillin/tazobactam which was discontinued after 5 days and switched to oral ciprofloxacin and metronidazole. After 10 days of vancomycin therapy, he developed fever followed by rash, and vancomycin was discontinued. The rash worsened and he developed evidence of both renal and hepatic injury leading to his admission. A skin biopsy and the presence of eosinophilia supported the diagnosis of DRESS syndrome and he was started on prednisone. Serum ALT levels rose to 1200 U/L with an alkaline phosphatase of 256 U/L and an INR of 1.8, while bilirubin levels increased slightly to a peak of 1.9 mg/dL. Serum creatinine peaked at 1.9 mg/dL. These values had been normal before the onset of DRESS (Table). His rash as well as both renal and hepatic tests began to improve and he was discharged and followed monthly in clinic. At 6 and 9 months after onset, he was asymptomatic, no longer taking prednisone and both liver and kidney tests were all within in normal range.
Key Points
| Medication: | Vancomycin (1.5 mg daily) iv for 14 days |
|---|---|
| Pattern: | Hepatocellular (R=6.2 rising to 11.3] |
| Severity: | Mild (enzyme elevations without jaundice) |
| Latency: | 2 weeks |
| Recovery: | 2 months |
| Other medications: | Piperacillin/tazobactam, ciprofloxacin |
Laboratory Values
| Time After Starting | Time After Stopping | ALT (U/L) | Alk P (U/L) | Bilirubin (mg/dL) | Other |
|---|---|---|---|---|---|
| Pre | Pre | 30 | 67 | 0.5 | |
| 0 | Pre | 27 | 78 | 0.4 | INR 1.1 |
| 15 days | 0 | Rash and fever: Vancomycin stopped | |||
| 3 weeks | 6 days | 301 | 78 | 0.6 | INR 1.5 |
| 7 days | 580 | 94 | 0.5 | Prednisone started | |
| 8 days | 791 | 111 | 0.5 | Creatinine 1.9 mg/dL | |
| 9 days | 1168 | 242 | 1.2 | INR 1.8 | |
| 10 days | 1200 | 238 | 1.7 | INR 1.8 | |
| 11 days | 1000 | 256 | 1.9 | INR 1.5 | |
| 4 weeks | 2 weeks | 619 | 258 | 1.3 | Discharged |
| 5 weeks | 3 weeks | 129 | 134 | 0.6 | |
| 5 weeks | 50 | 77 | 0.4 | ||
| 2 months | 7 weeks | 47 | 70 | 0.3 | |
| 3 months | 47 | 78 | 0.4 | Prednisone stopped: INR 1.0 | |
| 4 months | 38 | 76 | 0.3 | ||
| 5 months | 36 | 64 | 0.5 | ||
| 10 months | 9 months | 54 | 66 | 0.5 | Creatinine 0.8 mg/dL |
| Normal Values | <75 | <120 | <1.2 | ||
Comment
This man with diabetes, severe obesity and suspected nonalcoholic fatty liver disease developed DRESS syndrome 2 weeks after starting intravenous vancomycin for a postoperative infection. Despite stopping vancomycin fairly promptly and initiation of corticosteroid therapy a week later, liver tests worsened for another ten days before they began to improve. In follow up, he was able to stop the corticosteroid therapy and liver tests remained normal. As is typical of DRESS syndrome induced by vancomycin, renal dysfunction was also present and also resolved with prednisone therapy and time.
Case 2. DRESS Syndrome with jaundice due to vancomycin therapy.(1)
A 60 year old man with acute bacterial endocarditis due to Staphylococcus aureus was initially treated with intravenous vancomycin and nafcillin. Vancomycin was discontinued after 3 days when sensitivity results showed that the S. aureus was methicillin-sensitive. Two weeks later he developed rash and renal dysfunction that was attributed to nafcillin, which was discontinued and vancomycin restarted. Three weeks later he developed a worsening rash that spread to his entire body accompanied by fever and facial edema. He had recently been started on hydralazine because of hypertension not adequately controlled by metoprolol. Laboratory testing showed marked eosinophilia (16%) and abnormal liver tests with ALT 2018 U/L, AST 1232 U/L, Alk P 343 U/L and bilirubin 1.3 mg/dL. Renal function had worsened and serum creatinine was 6.4 mg/dL. Vancomycin and hydralazine were stopped and he was followed as an outpatient. A few days later his rash was worse and he was admitted for evaluation and therapy. A skin biopsy suggested a drug reaction. Tests for hepatitis A, B and C, Epstein Barr virus and cytomegalovirus were negative as were autoantibodies. Serum immunoglobulins were normal. Hydralazine was stopped and high dose corticosteroids were started. Thereafter, he improved rapidly and prednisone dose was slowly lowered. When seen 3, 5 and 6 months after onset, his liver tests were normal, but he remained on low doses of prednisone.
Key Points
| Medication: | Vancomycin (1.5 gm iv daily for 3 weeks) |
|---|---|
| Pattern: | Hepatocellular (R=28.2) |
| Severity: | Severe (INR >1.5) |
| Latency: | 3 weeks after restarting |
| Recovery: | 3 months on prednisone |
| Other medications: | Nafcillin, hydralazine (2 weeks), metoprolol |
Laboratory Values
| Time After Starting | Time After Stopping | ALT (U/L) | Alk P (U/L) | Bilirubin (mg/dL) | Albumin (g/dL) | INR | Comments |
|---|---|---|---|---|---|---|---|
| 0 | Pre | Started on intravenous nafcillin and vancomycin for bacterial endocarditis | |||||
| 3 days | Vancomycin discontinued: S. aureus methicillin-sensitive | ||||||
| 9 days | 17 | 32 | 0.3 | 3.5 | |||
| 18 days | 19 | 60 | 0.6 | 2.0 | Vancomycin restarted | ||
| 21 days | 37 | 107 | 0.4 | 3.4 | 1.1 | ||
| 40 days | 0 | 2018 | 260 | 1.3 | 3.8 | Vancomycin stopped | |
| 1 days | 1645 | 339 | 1.8 | Creatinine 6.4 mg/dL | |||
| 7 days | 457 | 343 | 3.0 | ||||
| 8 days | 361 | 293 | 2.3 | 2.8 | 1.6 | Prednisone started | |
| 9 days | 361 | 327 | 2.0 | 2.8 | 1.5 | ||
| 10 days | 384 | 292 | 1.9 | 2.7 | 1.5 | ||
| 14 days | 328 | 255 | 1.7 | 3.0 | 1.3 | ||
| 22 days | 85 | 176 | 0.9 | 3.5 | 1.1 | ||
| 31 days | 49 | 118 | 0.7 | ||||
| 41 days | 38 | 114 | 0.5 | ||||
| 3 months | 2 months | 21 | 98 | 0.5 | |||
| 3 months | 21 | 84 | 0.5 | ||||
| 5 months | 17 | 32 | 0.3 | 1.1 | |||
| 7 months | 6 months | 20 | 75 | 0.5 | 4.5 | 1.0 | Creatinine 1.1 mg/dL |
| Normal Values | <35 | <30 | <1.2 | >3.8 | <1.2 | ||
Comment
This man with bacterial endocarditis developed skin rash that was probably misinterpreted as being due to nafcillin and was restarted on vancomycin, the more likely culprit. Within 3 weeks he had a disseminated rash, fever, marked eosinophilia, worsening renal insufficiency and marked elevations in serum aminotransferase levels at which point vancomycin was discontinued. He became jaundiced and was started on prednisone which improved the symptoms of hypersensitivity. The renal and hepatic abnormalities improved slowly but were back in the normal range within the next few months. Why he was also taking hydralazine, the time to onset and clinical features were not typical of hydralazine induced liver injury. Most instances of DRESS associated with vancomycin arise within 1 to 6 weeks of starting the medication and are associated with mild or minimal hepatic abnormalities and more prominent renal dysfunction. In this instance, the prolonged therapy probably led to a more serious renal and hepatic involvement. While the hepatic abnormalities were associated with jaundice, the degree of hyperbilirubinemia was mild. Despite that, the INR rose to a level above 1.5 indicating that severe liver injury may have been present.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Vancomycin – Generic, Vancocin®
DRUG CLASS
Antiinfective Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULAS AND STRUCTURES
CITED REFERENCES
- 1.
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159]
ANNOTATED BIBLIOGRAPHY
References updated: 20 August 2020
Abbreviations: DRESS, drug reaction with eosinophilia and systemic symptoms; HLA, human leukocyte antigen; SJS, Stevens-Johnson syndrome; TEN, toxic epidermal necrolysis; iv, intravenous.
- Zimmerman HJ. Hepatic injury from antimicrobial agents. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, p. 592.(Expert review of liver injury published in 1999; does not mention vancomycin).
- Moseley RH. Vancomycin. Hepatotoxicity of antimicrobials and antifungal agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 469.(Expert review of antibiotic induced liver injury mentions that a single case report of vancomycin causing ALT elevations has been published).
- MacDougall C. Glycopeptides. Protein synthesis inhibitors and miscellaneous antibacterial agents. In, Brunton LL, Hilal-Dandan R, Knollman KC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1059-61.(Textbook of pharmacology and therapeutics).
- Rothenberg HJ. Anaphylactoid reaction to vancomycin. J Am Med Assoc. 1959;171:1101–2. [PubMed: 14439446](17 year old girl with acute bacterial endocarditis developed sudden onset of urticaria, rash, pruritis, chest pain, dyspnea and swelling of face, 10 minutes after receiving an initial dose of intravenous vancomycin [1 gm over 25 minutes], resolving rapidly with epinephrine and Benadryl, described as an “anaphylactoid” reaction).
- Geraci JE, Nichols DR, Wellman WE. Vancomycin in serious staphylococcal infections. Arch Intern Med. 1962;109:507–15. [PubMed: 13897823](Among 85 patients treated with vancomycin, none developed hepatic abnormalities and no instance of anaphylaxis was observed although cases have been described by others).
- Farber BF, Moellering RC Jr. Retrospective study of the toxicity of preparations of vancomycin from 1974 to 1981. Antimicrob Agents Chemother. 1983;23:138–41. [PMC free article: PMC184631] [PubMed: 6219616](Analysis of 100 courses of iv vancomycin in 98 patients; fever and rash occurred in 3%, phlebitis 13%, neutropenia 2%, nephrotoxicity 5%, ototoxicity 0%, creatinine rise 35%; no mention of hepatotoxicity or ALT elevations).
- Thompson CM Jr, Long SS, Gilligan PH, Prebis JW. Absorption of oral vancomycin - possible associated toxicity. Int J Pediatr Nephrol. 1983;4:1–4. [PubMed: 6853034](Low levels of vancomycin were detected in serum of an anephric child given drug orally for Clostridium difficile pseudomembranous colitis).
- Sorrell TC, Collignon PJ. A prospective study of adverse reactions associated with vancomycin therapy. J Antimicrob Chemother. 1985;16:235–41. [PubMed: 3934126](Prospective analysis of 54 courses of iv vancomycin given for 4-49 days; rash occurred in 6%, phlebitis 37%, neutropenia 0%, nephrotoxicity 8%, ototoxicity 0%, creatinine rise 50%; slight bilirubin rise in 1 patient; no mention of ALT elevations).
- Garrelts JC, Peterie JD. Vancomycin and the "red man's syndrome". N Engl J Med. 1985;312:245. [PubMed: 3155563](55 year old woman developed flushing, erythematous rash and pruritis 30 minutes into an initial infusion of vancomycin, resolving within 3 hours of stopping, and not recurring with subsequent vancomycin infusions given at a slower rate; first use of the term “red man syndrome”; the authors considered it to be an anaphylactoid reaction).
- Matzke GR, Zhanel GG, Guay DR. Clinical pharmacokinetics of vancomycin. Clin Pharmacokinet. 1986;11:257–82. [PubMed: 3530582](Extensive review of clinical pharmacology of vancomycin; major adverse events are renal toxicity and ototoxicity, skin rash, thrombophlebitis and fever; no mention of liver-related toxicity).
- Healy DP, Polk RE, Garson ML, Rock DT, Comstock TJ. Comparison of steady-state pharmacokinetics of two dosage regimens of vancomycin in normal volunteers. Antimicrob Agents Chemother. 1987;31:393–7. [PMC free article: PMC174739] [PubMed: 3579256](Among 11 healthy volunteers given 500 mg of intravenous vancomycin every 6 hours for 5 doses followed one week later by 1000 mg every 12 hours for 3 doses, the flushing syndrome occurred in 9 [89%] taking 1000 mg but in none taking 500 mg).
- Renz CL, Thurn JD, Finn HA, Lynch JP, Moss J. Oral antihistamines reduce the side effects from rapid vancomycin infusion. Anesth Analg. 1998;87:681–5. [PubMed: 9728853](Among 30 patients undergoing joint replacement surgery and receiving prophylactic infusions of vancomycin, rates of acute flushing syndrome were less in those receiving diphenhydramine and cimetidine [11 of 20: 55%] versus placebo [10 of 10: 100%]).
- Healy DP, Sahai JV, Fuller SH, Polk RE. Vancomycin-induced histamine release and "red man syndrome": comparison of 1- and 2-hour infusions. Antimicrob Agents Chemother. 1990;34:550–4. [PMC free article: PMC171642] [PubMed: 1693055](Among 10 healthy male volunteers given infusions of 1000 mg of vancomycin over 1 or 2 hours, the flushing syndrome was more frequent with the 1 hour infusion [80% vs 30%] and more severe with higher levels of plasma histamine and higher peak, but similar total concentration of vancomycin).
- Levy M, Koren G, Dupuis L, Read SE. Vancomycin-induced red man syndrome. Pediatrics. 1990;86:572–80. [PubMed: 2216623](Among 650 children who received intravenous vancomycin between 1986 and 1988 at Toronto Children’s Hospital, 11 were reported as having an acute flushing syndrome, ages from premature newborn to 8 years, arising with initial infusion, resolving within 5 minutes to 7 hours).
- Stier GR, McGory RW, Spotnitz WD, Schwenzer KJ. Hemodynamic effects of rapid vancomycin infusion in critically ill patients. Anesth Analg. 1990;71:394–9. [PubMed: 1698040](Among 16 critically ill patients after open heart surgery receiving vancomycin by rapid infusion [1000 mg over 5 minutes], plasma histamine levels were stable and unchanged in all except one patient who developed flushing and pruritus but without hemodynamic changes).
- Killian AD, Sahai JV, Memish ZA. Red man syndrome after oral vancomycin. Ann Intern Med. 1991;115:410–1. [PubMed: 1830733](67 year old woman with pseudomembranous colitis developed severe pruritus and flushing 50 minutes after an initial dose of oral vancomycin [given by nasogastric tube], which did not recur with intravenous administration but did with further oral doses, ameliorated by diphenhydramine and decreasing in severity with each subsequent dose).
- Wallace MR, Mascola JR, Oldfield EC 3rd. Red man syndrome: incidence, etiology, and prophylaxis. J Infect Dis. 1991;164:1180–5. [PubMed: 1955716](Among 33 patients monitored during the first two doses of vancomycin with or without diphenhydramine pretreatment, acute flushing syndrome arose in none of the pretreated subjects but in 8 of 17 placebo recipients, reactions recurring in 3 of 8 first dose reactors with the second dose; plasma histamine levels were elevated in patients developing the flushing syndrome).
- Wilhelm MP. Vancomycin. Mayo Clin Proc. 1991;66:1165–70. [PubMed: 1943250](Extensive review of vancomycin pharmacology, clinical efficacy and adverse events; no mention of hepatotoxicity).
- O'Sullivan TL, Ruffing MJ, Lamp KC, Warbasse LH, Rybak MJ. Prospective evaluation of red man syndrome in patients receiving vancomycin. J Infect Dis. 1993;168:773–6. [PubMed: 8354921](Among 29 patients receiving intravenous vancomycin followed prospectively, only 1 developed the acute flushing syndrome [3%] and plasma histamine levels increased minimally and did not predict flushing).
- Hauben M, Adler C. Acute hepatitis, interstitial nephritis, and eosinophilia. Ann Intern Med. 1995;122:555–6. [PubMed: 7872595](35 year old woman with HIV infection developed acute rise in ALT [from 47 to 2374 U/L] and creatinine [from 0.8 to 7.6 mg/dL] and eosinophilia with no mention of jaundice, within 4 days of starting vancomycin and aztreonam; values improved after stopping, but were still abnormal 7 days later; patient also received a day of erythromycin).
- Alexander II, Greenberger PA. Vancomycin-induced Stevens-Johnson syndrome. Allergy Asthma Proc. 1996;17:75–8. [PubMed: 8934797](36 year old man developed Stevens-Johnson syndrome after 17 days of iv vancomycin, requiring switch to piperacillin and gentamicin with accompanying mild liver injury thereafter [AST 198 U/L, Alk P 232 U/L but no jaundice]; Stevens-Johnson syndrome responded to corticosteroids).
- Martí R, Rosell M, Pou L, García L, Pascual C. Influence of biochemical parameters of liver function on vancomycin pharmacokinetics. Pharmacol Toxicol. 1996;79:55–9. [PubMed: 8878246](Retrospective analysis of 76 patients treated with vancomycin revealed no liver abnormalities).
- Elting LS, Rubenstein EB, Kurtin D, Rolston KVI, Fangtang J, Martin CG, Raad II, et al. Mississippi mud in the 1990s: risks and outcomes of vancomycin-associated toxicity in general oncology practice. Cancer. 1998;83:2597–607. [PubMed: 9874468](765 cancer patients were treated with vancomycin; significant nephrotoxicity, but no hepatotoxicity was noted).
- Renz CL, Thurn JD, Finn HA, Lynch JP, Moss J. Antihistamine prophylaxis permits rapid vancomycin infusion. Crit Care Med. 1999;27:1732–7. [PubMed: 10507591](Among 40 preoperative patients given 1000 mg of vancomycin over 10 minutes with or without premedication with diphenhydramine or cimetidine or placebo, rates of hypotension [11% vs 63%] and rash [63% vs 100%] were less with the antihistamine [anti-H1 or H2] prophylaxis).
- Hassaballa H, Mallick N, Orlowski J. Vancomycin anaphylaxis in a patient with vancomycin-induced red man syndrome. Am J Ther. 2000;7:319–20. [PubMed: 11317179](45 year old woman with systemic lupus and end-stage liver disease developed flushing, tongue swelling emesis, hypotension, and rigors, shortly after initiation of an infusion of vancomycin, progressing to coma and respiratory arrest, but responding to ventilation and supportive measures including corticosteroids and antihistamines).
- Zuliani E, Zwahlen H, Gilliet F, Marone C. Vancomycin-induced hypersensitivity reaction with acute renal failure: resolution following cyclosporine treatment. Clin Nephrol. 2005;64:155–8. [PubMed: 16114793](45 year old woman developed fever 34 days after starting vancomycin followed by rash and renal failure [bilirubin 2.4 mg/dL, ALT 462 U/L, Alk P 257 U/L], treated with prednisone with two relapses during recovery).
- Yazganoglu KD, Ozkaya E, Ergin-Ozcan P, Cakar N. Vancomycin-induced drug hypersensitivity syndrome. J Eur Acad Dermatol Venereol. 2005;19:648–50. [PubMed: 16164735](56 year old woman developed fever, rash, facial edema and eosinophilia [1396/µL] 20 days after starting vancomycin [bilirubin and Alk P not given, ALT 229 U/L], resolving after 2 months on corticosteroid therapy).
- Cadle RM, Mansouri MD, Darouiche RO. Vancomycin-induced elevation of liver enzyme levels. Ann Pharmacother. 2006;40:1186–9. [PubMed: 16720708](57 year old man with Clostridium difficile colitis and persistent diarrhea was treated with oral vancomycin on 5 occasions, developing progressively increasing elevations in ALT [~100-400 U/L] without symptoms or jaundice with each treatment; ALT returned to baseline after each course and vancomycin could not be detected in serum).
- Kwon HS, Chang YS, Jeong YY, Lee SM, Song WJ, Kim HB, Kim YK, et al. A case of hypersensitivity syndrome to both vancomycin and teicoplanin. J Korean Med Sci. 2006;21:1108–10. [PMC free article: PMC2721938] [PubMed: 17179696](50 year old man with cirrhosis developed fever, rash and eosinophilia [1605/µL] 18 days after starting iv vancomycin [liver test results not provided], resolving on stopping vancomycin, but recurring on intravenous teicoplanin [an antibiotic similar to vancomycin]).
- Tamagawa-Mineoka R, Katoh N, Nara T, Nishimura Y, Yamamoto S, Kishimoto S. DRESS syndrome caused by teicoplanin and vancomycin, associated with reactivation of human herpesvirus-6. Int J Dermatol. 2007;46:654–5. [PubMed: 17550572](52 year old woman developed fever, lymphadenopathy, rash, facial edema and eosinophilia [7%] a few days after starting iv vancomycin [bilirubin not provided, ALT 547 U/L, Alk P 2209 U/L], resolving once vancomycin was stopped and corticosteroids added; positive lymphocyte stimulation test to vancomycin and teicoplanin).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected from 2004 to 2008, none were attributed to vancomycin).
- Vauthey L, Uçkay I, Abrassart S, Bernard L, Assal M, Ferry T, Djordjevic M, et al. Vancomycin-induced DRESS syndrome in a female patient. Pharmacology. 2008;82:138–41. [PubMed: 18607115](60 year old woman developed fever, rash and facial edema 18 days after starting iv vancomycin [liver tests normal except for GGT of 224 U/L], resolving with corticosteroid therapy).
- Bailey P, Gray H. An elderly woman with 'Red Man Syndrome' in association with oral vancomycin therapy: a case report. Cases J. 2008;1:111. [PMC free article: PMC2527496] [PubMed: 18710566](82 year old woman with C. difficile diarrhea developed disseminated pruritic rash and headaches 4 days after starting oral vancomycin, responding rapidly to discontinuation and antihistamines; no mention of liver involvement).
- Mennicke M, Zawodniak A, Keller M, Wilkens L, Yawalkar N, Stickel F, Keogh A, et al. Fulminant liver failure after vancomycin in a sulfasalazine-induced DRESS syndrome: fatal recurrence after liver transplantation. Am J Transplant. 2009;9:2197–202. [PubMed: 19706026](60 year old man developed fever, rash and eosinophilia 6 weeks after starting sulfasalazine [bilirubin 2.7 mg/dL, ALT 650 U/L, Alk P 181 U/L]; started on iv vancomycin and ALT rose to 6,745 U/L two days later; emergency liver transplantation was done, after which he developed rash, fever and liver injury again while on piperacillin/tazobactam and caspofungin, dying suddenly of hemorrhage).
- Vinson AE, Dufort EM, Willis MD, Eberson CP, Harwell JI. Drug rash, eosinophilia, and systemic symptoms syndrome: Two pediatric cases demonstrating the range of severity in presentation--A case of vancomycin-induced drug hypersensitivity mimicking toxic shock syndrome and a milder case induced by minocycline. Pediatr Crit Care Med. 2010;11:e38–43. [PubMed: 20407399](14 year old boy developed fever and rash 3 weeks after starting iv vancomycin and worsened with continuation [ALT 92 rising to 436 U/L, bilirubin and Alk P not given, eosinophils 16%], responding to stopping drug and corticosteroids).
- Chen Y, Yang XY, Zeckel M, Killian C, Hornbuckle K, Regev A, Voss S. Risk of hepatic events in patients treated with vancomycin in clinical studies: a systematic review and meta-analysis. Drug Saf. 2011;34:73–82. [PubMed: 21142272](Systematic review of 20 controlled trials of iv vancomycin in 7419 patients, found rates of liver enzyme elevations ["hepatic events"] to be 1.8-1.9 times higher with vancomycin than with comparator arms; with vancomycin monotherapy rates were only 0.4% vs 0.3%, while with combination therapy rates were 6.8% vs 3.9%; no reports of clinically apparent liver disease with jaundice).
- Schnetzke U, Bossert T, Scholl S, Freesmeyer M, Hochhaus A, La Rosée P. Drug-induced lymphadenopathy with eosinophilia and renal failure mimicking lymphoma disease: dramatic onset of DRESS syndrome associated with antibiotic treatment. Ann Hematol. 2011;90:1353–5. [PubMed: 21298267](30 year old man developed fever, lymphadenopathy, atypical lymphocytosis, eosinophilia [25%] and acute renal failure while receiving several antibiotics including vancomycin [liver test results not given], resolving with corticosteroid therapy after stopping antibiotics).
- O'Meara P, Borici-Mazi R, Morton AR, Ellis AK. DRESS with delayed onset acute interstitial nephritis and profound refractory eosinophilia secondary to vancomycin. Allergy Asthma Clin Immunol. 2011;7:16. [PMC free article: PMC3198947] [PubMed: 21968185](66 year old man developed rash 4 weeks after starting iv vancomycin therapy followed by fever [40 oC] and facial edema [bilirubin 0.8 mg/dL, ALT 144 U/L, GGT 354 U/L, eosinophils 3620/µL], with subsequent respiratory and renal failure, followed by a slow, but ultimately full recovery on corticosteroid therapy).
- Fleming P, Marik PE. The DRESS syndrome: the great clinical mimicker. Pharmacotherapy. 2011;31:332. [PubMed: 21361742](44 year old woman with tracheostomy, hemorrhagic stroke and sepsis developed fever, rash and eosinophilia [25%] several days after starting iv vancomycin [bilirubin 0.2 rising to 12.8 mg/dL, ALT 127 U/L, Alk P not provided], responding to corticosteroid therapy).
- Tran NP, Katcher J, Rohman E, Hall MF, Michael CF, Miyairi I, Lew DB. Vancomycin hypersensitivity diagnosed by lymphocyte blast transformation. Case Rep Pediatr. 2011;2011:562620. [PMC free article: PMC3350173] [PubMed: 22606516](15 year old male developed rash, fever and renal disease 8-10 days after starting vancomycin [eosinophils 980/µL, liver tests not provided], with positive lymphocyte stimulation test to vancomycin and resolution on switching to other antibiotics).
- Blumenthal KG, Patil SU, Long AA. The importance of vancomycin in drug rash with eosinophilia and systemic symptoms (DRESS) syndrome. Allergy Asthma Proc. 2012;33:165–71. [PubMed: 22525393](Among 6 cases of DRESS syndrome seen at a single referral hospital over an 18 month period, 5 arose 12 days to 4 weeks after starting iv vancomycin therapy with fever, rash and eosinophilia [bilirubin 1.8 mg/dL in one patient, ALT 75-347 U/L, Alk P 181-378 U/L], 4 had history of allergies, 3 were treated with corticosteroids, 2 had at least one relapse, and all ultimately resolved).
- Müller PA, Amann K, Bröcker EB, Trautmann A. Hautarzt. 2012;63:223–5. [Maculo-papular exanthem with acute renal failure. Drug-induced hypersensitivity syndrome] German. [PubMed: 21971769](44 year old man developed fever, rash, eosinophilia [3601/µL] and renal injury 4 weeks after starting iv vancomycin [liver tests not provided], resolving with corticosteroid therapy).
- Díaz-Mancebo R, Costero-Fernández O, Vega-Cabrera C, Olea-Tejero T, Yébenes L, Picazo ML, Selgas-Gutiérrez R. Dress syndrome and acute tubulointerstitial nephritis after treatment with vancomycin and beta-lactams. Case report and literature review. Nefrologia. 2012;32:685–7. [PubMed: 23013963](74 year old woman developed rash, fever, eosinophilia and renal failure several weeks after starting vancomycin [ALT raised, values not given], with slow resolution on corticosteroid therapy).
- Kitcharoensakkul M, Ree N, Bloomberg GR, Dehner LP, Heidingsfelder JA, White AJ, Cooper MA. Vancomycin-induced DRESS with evidence of T-cell activation in a 22-month-old patient. Ann Allergy Asthma Immunol. 2012;109:280–1. [PubMed: 23010236](22 year old woman developed fever, rash and eosinophilia 17 days after starting iv vancomycin [hepatomegaly noted but no liver tests provided], improving on corticosteroid therapy, but dying suddenly 18 days after hospital discharge).
- Dauby N, Fink W, Seyler L, Luce S, Nouwynck C, Tas S, Jacobs F. Probable hypersensitivity reaction to vancomycin associating rash, fever and neutropenia. Acta Clin Belg. 2012;67:226–8. [PubMed: 22897075](54 year old woman with cancer developed fever after 7 days of vancomycin therapy followed by rash and, with restarting vancomycin, neutropenia and serum ALT elevations ["up to 3 times normal"], resolving rapidly upon stopping vancomycin).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, none of which were attributed to vancomycin).
- Song SM, Cho MS, Oh SH, Kim KM, Park YS, Kim DY, Lee SG. Liver transplantation in a child with acute liver failure resulting from drug rash with eosinophilia and systemic symptoms syndrome. Korean J Pediatr. 2013;56:224–6. [PMC free article: PMC3668204] [PubMed: 23741237](14 year old girl developed fever, rash and abnormal liver tests 5 weeks after starting vancomycin for a MRSA wound infection [bilirubin 3.3 rising to 15.5 mg/dL, ALT 263 to 1077 U/L, Alk P 440 U/L, eosinophils 3150/μL], worsening despite methylprednisone and undergoing liver transplant within 9 days of onset).
- Della-Torre E, Yacoub MR, Pignatti P, Della-Torre F, Sabbadini MG, Colombo G, Tresoldi M. Optimal management of DRESS syndrome in course of infectious endocarditis. Ann Allergy Asthma Immunol. 2013;110:303–5. [PubMed: 23535099](75 year old man developed fever and rash 27 days after starting vancomycin, gentamicin and rifampin for endocarditis [bilirubin not given, ALT 264 U/L, Alk P 247 U/L, eosinophils 6%], with resolution within 8 weeks on methylprednisone and IVIG).
- Bhardwaj N, Ishmael FT. Cytokine gene expression profiling to help identify a safe antibiotic in a patient with drug rash with eosinophilia and systemic symptoms. J Allergy Clin Immunol Pract. 2013;1:531–3. [PubMed: 24565631](53 year old man developed rash, fever, eosinophilia [36%] and creatinine elevation [liver tests not done] during week 3 of vancomycin and cefepime therapy, recovering with stopping both antibiotics but subsequent rash after single doses of each drug; follow up in vitro assays for cytokine expression after exposure to both drugs were positive).
- Young S, Ojaimi S, Dunckley H, Douglas MW, Kok J, Fulcher DA, Lin MW, et al. Vancomycin-associated drug reaction with eosinophilia and systemic symptoms syndrome. Intern Med J. 2014;44:694–6. [PubMed: 25041771](Two men and one woman, ages 24 to 59 years developed rash, fever, eosinophilia, atypical lymphocytosis and ALT elevations [113 to 337 U/L, bilirubin not provided] 2-3 weeks after starting vancomycin resolving with corticosteroid therapy; HLA testing was positive for A*32 in two of the three).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, none of which were attribute to vancomycin).
- Sultan SJ, Sameem F, Ashraf M. Drug reaction with eosinophilia and systemic symptoms: manifestations, treatment, and outcome in 17 patients. Int J Dermatol. 2015;54:537–42. [PubMed: 24738653](Among 17 patients with DRESS syndrome seen at a referral center in India over a 4 year period, most cases [65%] were due to aromatic anticonvulsants, 2 to allopurinol and 1 each for vancomycin, leflunomide, dapsone and nitrofurantoin, with ALT elevations above 100 U/L in all 17, hyperbilirubinemia in 65% and liver failure in one).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 363 [36%] were attributed to antibiotics, three of which were due to vancomycin all of them occurring after 2008).
- Korman TM, Turnidge JD, Grayson ML. Vancomycin vintage: my favourite DRESS. Intern Med J. 2015;45:233–4. [PubMed: 25650542](Letter in response to report by Young [2014] mentioning that vancomycin associated DRESS syndrome was first reported in the 1960s but was attributed to contaminants, but similar cases have been described even after improved methods of purification of vancomycin, skin rash occurring in at least 5% of patients with accompanying eosinophilia in most).
- Blumenthal KG, Youngster I, Rabideau DJ, Parker RA, Manning KS, Walensky RP, Nelson SB. Peripheral blood eosinophilia and hypersensitivity reactions among patients receiving outpatient parenteral antibiotics. J Allergy Clin Immunol. 2015;136:1288–94.e1. [PMC free article: PMC4640981] [PubMed: 25981739](Among 824 patients who underwent outpatient parenteral antibiotic therapy for at least 2 weeks, 210 [25%] developed eosinophilia [500 to 8260 cells/uL], the highest rate being among recipients of vancomycin [30%: 95 of 314], rates of DRESS syndrome and liver involvement not provided).
- Güner MD, Tuncbilek S, Akan B, Caliskan-Kartal A. Two cases with HSS/DRESS syndrome developing after prosthetic joint surgery: does vancomycin-laden bone cement play a role in this syndrome? BMJ Case Rep. 2015;2015:bcr2014207028. [PMC free article: PMC4458625] [PubMed: 26021379](Two patients who underwent orthopedic prosthesis replacement using vancomycin-laden bone cement followed by intravenous vancomycin developed fever, rash, eosinophilia and creatine elevations [one had ALT elevations as well] 2 and 4 weeks following initiation of parenteral vancomycin and both responded to high dose corticosteroid therapy).
- Adams B, Roboubi B, Henshaw R. Acute onset of vancomycin anaphylaxis with disseminated intravascular coagulation in an orthopedic patient despite prior repeated exposure. Am J Orthop (Belle Mead NJ). 2015;44:E523–5. [PubMed: 26665256](55 year old woman with a prosthetic infection and multiple previous exposures to vancomycin developed hypotension, without rash, fever or eosinophilia, during an infusion of vancomycin during surgery, responding to stopping the infusion and resuscitation thought to be due to anaphylaxis).
- McNeil BD, Pundir P, Meeker S, Han L, Undem BJ, Kulka M, Dong X. Identification of a mast-cell-specific receptor crucial for pseudo-allergic drug reactions. Nature. 2015;519:237–41. [PMC free article: PMC4359082] [PubMed: 25517090](In vitro and in vivo data demonstrate that mast cell degranulation can be induced by a range of cationic peptidergic drugs via direct engagement of G-protein linked receptors on mast cells [MRGPR] which causes release of granules with histamine, tumor necrosis factor, prostaglandin D, interleukins and other active amines).
- Kumar T, Teo I, McCormick BB. Systemic toxicity of intraperitoneal vancomycin. Case Rep Nephrol. 2016;2016:3968690. [PMC free article: PMC5093231] [PubMed: 27840751](45 year old man with end-stage renal disease on peritoneal dialysis developed rash, fever and hypotension 3 weeks after starting peritoneal doses of vancomycin with normal ALT, Alk P and bilirubin levels responding to corticosteroids; authors mention 3 other case reports of hypersensitivity to Intraperitoneal vancomycin but no mention of hepatic involvement).
- Kim KM, Sung K, Yang HK, Kim SH, Kim HY, Ban GH, Park SE, et al. Acute tubular necrosis as a part of vancomycin induced drug rash with eosinophilia and systemic symptoms syndrome with coincident postinfectious glomerulonephritis. Korean J Pediatr. 2016;59:145–8. [PMC free article: PMC4865626] [PubMed: 27186222](11 year old boy developed fever, rash and edema after a 10 day course of vancomycin and ceftriaxone with eosinophilia [24%] and proteinuria but normal serum ALT and AST, eventually improving with corticosteroid therapy but with residual nephrotic syndrome).
- Sousa JM, Nascimento H, Belfort R. Junior. DRESS syndrome in ophthalmic patients. Arq Bras Oftalmol. 2016;79:192–4. [PubMed: 27463633](Two patients with DRESS syndrome after antibiotic therapy of endophthalmitis [intravenous cephalothin and intravitreous vancomycin] and vitritis [parenteral sulfadiazine/pyrimethamine], both resolving with high dose corticosteroids and stopping the implicate antibiotics).
- Webb PS, Al-Mohammad A. Enigma: infection or allergy? vancomycin-induced DRESS syndrome with dialysis-dependent renal failure and cardiac arrest. BMJ Case Rep. 2016;2016:bcr2016215911. [PMC free article: PMC5015148] [PubMed: 27571915](73 year old man with culture negative endocarditis developed fever, rash and eosinophilia after 23 days of antibiotic therapy including intermittent use of vancomycin, ultimately resolving with stopping the implicated agents and starting corticosteroid therapy; acute renal dysfunction requiring temporary dialysis but no mention of liver test abnormalities).
- Miyazu D, Kodama N, Yamashita D, Tanaka H, Inoue S, Imakyure O, Hirakawa M, et al. DRESS syndrome caused by cross-reactivity between vancomycin and subsequent teicoplanin administration: a case report. Am J Case Rep. 2016;17:625–31. [PMC free article: PMC5012458] [PubMed: 27572807](79 year old man with a complicated wound infection after traumatic injury developed fever and erythema after 18 days of vancomycin therapy with subsequent eosinophilia and pneumonitis, improving when switched to teicoplanin and given corticosteroids, but relapsed 12 days later, improving when antibiotic was switched to linezolid suggesting cross sensitivity to DRESS syndrome of the two somewhat similar glycopeptide antibiotics).
- Evans T, Patel S. Two consecutive preoperative cardiac arrests involving vancomycin in a patient presenting for hip disarticulation: a case report. A A Case Rep. 2017;9:262–4. [PubMed: 28622151](59 year old woman receiving vancomycin in preparation of hip surgery developed sudden hypotension and cardiac arrest which successful resuscitation and had the identical response to an infusion of vancomycin given 4 weeks later, the initial episode having been attributed to another agent [midazolam]; no mention of rash, fever or pruritus).
- Mattoussi N, Ben Mansour A, Essadam L, Guedri R, Fitouri Z, Ben Becher S. Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome in children: a case report. J Investig Allergol Clin Immunol. 2017;27:144–6. [PubMed: 28398207](14 year old boy with sickle cell-thalassemia and acute septicemia developed fever and lymphadenopathy followed by rash, facial edema and eosinophilia after 2-3 weeks of intravenous vancomycin and cefotaxime [ALT 313 U/L, bilirubin 1.2 mg/dL], responding to stopping antibiotics and use of antihistamines; follow up patch tests were positive for vancomycin only).
- Maxfield L, Schlick T, Macri A, Thatcher J. Vancomycin-associated drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome: masquerading under the guise of sepsis. BMJ Case Rep. 2017;2017:bcr2017221898. [PMC free article: PMC5665279] [PubMed: 29054953](52 year old man developed fever and confusion thought to be due to sepsis, but not responding to antibiotics and arising 3 weeks after receiving vancomycin for osteomyelitis, ultimately manifested by rash, lymphadenopathy, eosinophilia and liver and renal test abnormalities [ALT 136 U/L, Alk P 240 U/L, creatinine 1.3 rising to 3.8 mg/dL], responding to high dose methylprednisolone).
- Lam BD, Miller MM, Sutton AV, Peng D, Crew AB. Vancomycin and DRESS: A retrospective chart review of 32 cases in Los Angeles, California. J Am Acad Dermatol. 2017;77:973–5. [PubMed: 29029908](Among 32 patients diagnosed with DRESS syndrome at two California hospitals over a 3 year period, vancomycin was the most frequently implicated agent [n=12: 38%]).
- Wilcox O, Hassanein M, Armstrong J, Kassis N. Case report: atypical presentation of vancomycin induced DRESS syndrome: a case report and review of the literature. BMC Pulm Med. 2017;17:217. [PMC free article: PMC5745618] [PubMed: 29282040](39 year old man with osteomyelitis developed fever and shortness of breath after 3 weeks of intravenous vancomycin therapy followed by severe respiratory distress syndrome, acute kidney injury, rash, fever and eosinophilia, responding rapidly to stopping vancomycin and use of high doses of corticosteroids).
- Azimi E, Reddy VB, Lerner EA. Brief communication: MRGPRX2, atopic dermatitis and red man syndrome. Itch (Phila). 2017;2:e5. [PMC free article: PMC5375112] [PubMed: 28367504](Mast cells can be degranulated by IgE independent pathways via engagement of specific G-protein linked receptors which are activated by vancomycin causing degranulation, an action that can be blocked by inhibition of MRGPRX2).
- Hashizume H, Kageyama R, Kaneko Y. Short course of cyclosporin A as a treatment option for drug-induced hypersensitivity syndrome: Case reports and review of the published work. J Dermatol. 2018;45:e169–e170. [PubMed: 29315746](Two adults with hypersensitivity reactions marked by rash, fever and eosinophilia attributed to medications [Case 1: lamotrigine, Case 2 vancomycin] treated successfully with a 7 day course of oral cyclosporin [3 mg/kg/day] and review of the literature of 4 similarly treated cases with successful outcomes]; no mention of hepatic involvement).
- Nagahama Y, VanBeek MJ, Greenlee JDW. Red man syndrome caused by vancomycin powder. J Clin Neurosci. 2018;50:149–50. [PubMed: 29398192](73 year old man developed intense erythema around site of vancomycin powder application during placement of a medical device, 2 days after surgery, resolving with symptomatic therapy only; no mention of liver test abnormalities).
- Lin YC, Sheu JN, Chung WH, Pan RY, Hung CJ, Cheng JJ, Hsiao YP. Vancomycin-induced Stevens-Johnson syndrome in a boy under 2 years old: an early diagnosis by granulysin rapid test. Front Pediatr. 2018;6:26. [PMC free article: PMC5859217] [PubMed: 29594082](19 month old boy developed rash after 13 days of vancomycin therapy for empyema which worsened and became generalized with blistering and oral ulcers by 30 days, with positive results using a granulysin assay; no mention of liver involvement).
- Littlehales E, Murray O, Dunsmuir R. Vancomycin-induced DRESS syndrome: an important concern in orthopedic surgery. Case Rep Orthop. 2018;2018:1439073. [PMC free article: PMC6035812] [PubMed: 30034896](62 year old man with postoperative spinal infection developed a maculopapular rash 7 weeks after starting intravenous vancomycin progressing to extensive, pruritic and painful rash and exfoliation, with fever, lymphadenopathy and eosinophilia but without hepatic or renal abnormalities treated with topical steroids and antihistamines only).
- Castellazzi ML, Esposito S, Claut LE, Daccò V, Colombo C. Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome in two young children: the importance of an early diagnosis. Ital J Pediatr. 2018;44:93. [PMC free article: PMC6094901] [PubMed: 30111350](Two cases of DRESS syndrome in children, ages 5 and 4 years with onset of rash 30 and 14 days after starting intravenous vancomycin with fever, lymphadenopathy, eosinophilia and ALT elevations [peak 132 and 311 U/L], both resolving after stopping drug, one requiring a 3 day pulse of corticosteroids and one not).
- Chamorro-Pareja N, Patel A, Youngberg G, Gonzalez-Estrada A. Case of drug reaction with eosinophilia and systemic symptoms secondary to vancomycin. BMJ Case Rep. 2018;2018:bcr2018227378. [PMC free article: PMC6194439] [PubMed: 30301733](38 year old man developed rash, fever, facial edema, lymphadenopathy, eosinophilia and atypical lymphocytosis 3 weeks after starting intravenous vancomycin for osteomyelitis, resolving with corticosteroid therapy; no mention of ALT elevations).
- Sun Y, Huskey RL, Tang L, Inaba H, Gaur AH, Ribeiro R, Rubnitz JE, Wolf J. Adverse effects of intravenous vancomycin-based prophylaxis during therapy for pediatric acute myeloid leukemia. Antimicrob Agents Chemother. 2018;62:e01838–17. [PMC free article: PMC5826122] [PubMed: 29229640](Among 116 children with acute myelogenous leukemia treated with 392 courses of chemotherapy, rates of any ALT elevations were similar in those given vancomycin prophylaxis [47%] and those given no prophylaxis [57%] while rates of C. difficile infection were less).
- Khanal S, Ghimire P, Dhamoon AS. Liver injury during treatment with rifampicin, vancomycin, and acetaminophen. Am J Ther. 2018;25:e735–e737. [PubMed: 29557806](40 year old man with osteomyelitis developed abnormal liver tests while being treated with acetaminophen, vancomycin and rifampin [ALT rising from 8 to 224 to 735 U/L, bilirubin peak 2.1 mg/dL, no mention of fever, rash or eosinophilia], resolving with stopping all three medications).
- Wolfson AR, Zhou L, Li Y, Phadke NA, Chow OA, Blumenthal KG. Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome Identified in the Electronic Health Record Allergy Module. J Allergy Clin Immunol Pract. 2019;7:633–40. [PMC free article: PMC6363826] [PubMed: 30176295](Search of electronic medical records from more than 3 million subjects identified 69 cases of DRESS syndrome [~2 per 100,000 population], the most common causes of which were vancomycin [n=29], penicillin [13], phenytoin [10], cephalosporins [7] and lamotrigine [6]).
- Madigan LM, Fox LP. Vancomycin-associated drug-induced hypersensitivity syndrome. J Am Acad Dermatol. 2019;81:123–8. [PubMed: 30738120](Among 19 cases of DRESS syndrome seen over an 8 year period at a single US referral center, 4 were attributed to vancomycin, 3 of whom had renal involvement which is typical of cases caused by vancomycin).
- Konvinse KC, Trubiano JA, Pavlos R, James I, Shaffer CM, Bejan CA, Schutte RJ, et al. HLA-A*32:01 is strongly associated with vancomycin-induced drug reaction with eosinophilia and systemic symptoms. J Allergy Clin Immunol. 2019;144:183–92. [PMC free article: PMC6612297] [PubMed: 30776417](Among patients with a history of vancomycin induced DRESS syndrome identified between 2004 and 2018, HLA typing demonstrated the A*32:01 allele in 19 of 23 [83%] of DRESS cases compared to none of 46 matched vancomycin-tolerant subjects and to a carrier rate of 6.3% in population controls, vancomycin fitting into the antigen groove of HLA-A*32:01 in molecular docking prediction analyses).
- Pirmohamed M. HLA- and immune-mediated adverse drug reactions: another hit with vancomycin. J Allergy Clin Immunol. 2019;144:44–5. [PubMed: 31029771](Editorial accompanying Konvinse [2019] discussing role that HLA associations can play in prevention, risk management and diagnosis of drug adverse events).
- Maldonado D, Lakhani J. Vancomycin-induced DRESS syndrome treated with systemic steroids in a 16-year-old male. SAGE Open Med Case Rep 2019; 7: 2050313X19841704. [PMC free article: PMC6452422] [PubMed: 31057800](16 year old adolescent boy developed fever, rash, sore throat and eosinophilia after completing a 4 week course of vancomycin for a bone infection, responding rapidly to switching to doxycycline and high dose corticosteroids).
- Roy S, Goswamy VP, Barssoum KN, Rai D. Vancomycin-induced drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome masquerading as elusive sepsis. Case Reports Immunol. 2019;2019:1625010. [PMC free article: PMC6481134] [PubMed: 31093389](37 year old woman injection drug user was admitted for therapy for septic pulmonary emboli and continued to have fever during vancomycin therapy, then developing rash, rise in ALT levels [1192 U/L], eosinophilia and renal dysfunction [creatinine 1.4 mg/dL], improving once vancomycin was stopped and corticosteroids started).
- Sim DW, Yu JE, Jeong J, Jung JW, Kang HR, Kang DY, Ye YM, et al. Korean Severe Cutaneous Adverse Reactions Consortium. Variation of clinical manifestations according to culprit drugs in DRESS syndrome. Pharmacoepidemiol Drug Saf. 2019;28:840–8. [PubMed: 31044478](Among 123 patients with DRESS syndrome enrolled in a prospective Korean adverse event registry, the most common causes were allopurinol [n=28], carbamazepine [22], antituberculosis drugs [19], vancomycin [18], cephalosporins [15], dapsone [11] and NSAIDs [10]; liver involvement was present in 56-100% [the lowest rate with vancomycin] and renal involvement in 9-79% [the highest rates with allopurinol and vancomycin], and with 6 deaths [5%], 2 due to vancomycin).
- Rwandamuriye FX, Chopra A, Konvinse KC, Choo L, Trubiano JA, Shaffer CM, Watson M, et al. A rapid allele-specific assay for HLA-A*32:01 to identify patients at risk for vancomycin-induced drug reaction with eosinophilia and systemic symptoms. J Mol Diagn. 2019;21:782–9. [PMC free article: PMC6734857] [PubMed: 31158526](Description of an allele specific PCR method for rapid detection of HLA-A*32:01 that correctly identified all 30 positive DNA samples and was negative on all 428 negative samples that had been typed using formal sequence based methods).
- Gangireddy M, Sarao MS, Shrimanker I, Nookala VK. A fatal case of vancomycin associated drug reaction with eosinophilia and systemic symptoms syndrome in a septuagenarian. Cureus. 2019;11:e5015. [PMC free article: PMC6716765] [PubMed: 31497445](79 year old woman developed abdominal pain, jaundice and rash 6 weeks after starting parenteral vancomycin and cefepime [bilirubin 14.2 rising to 22.2 mg/dL, ALT 674 U/L, Alk P 2742 U/L, creatinine 5.0 mg/dL], with progressive liver failure and death from multiorgan failure despite stopping vancomycin and use of high dose corticosteroids).
- Ercan N, Yeşillik S, Demirel F, Tırık N, Kartal Ö. Haplotype analysis in a 16-year-old boy with vancomycin-induced DRESS syndrome. Pediatr Dermatol. 2019;36:992–4. [PubMed: 31497897](16 year old boy with meningoencephalitis developed rash, fever, lymphadenopathy and periorbital edema 10 days after starting vancomycin with atypical lymphocytosis, ALT 244 U/L, but normal tests of kidney function, responding to a course of corticosteroid therapy with no residual in follow up).
- Arroyo-Mercado F, Khudyakov A, Chawla GS, Cantres-Fonseca O, McFarlane IM. Red man syndrome with oral vancomycin: a case report. Am J Med Case Rep. 2019;7:16–7.(75 year old woman with C. difficile diarrhea developed flushing, erythema and pruritis involving face, neck and upper torso after the 7th dose of oral vancomycin, responding to discontinuation and antihistamines; no mention of liver involvement).
- Swali R, Ghazarian A. The case of the magenta woman (DRESS syndrome). Proc (Bayl Univ Med Cent). 2019;33:115–6. [PMC free article: PMC6988695] [PubMed: 32063794](44 year old woman with osteomyelitis developed DRESS syndrome 1 month after starting intravenous vancomycin with disseminated rash, facial edema, eosinophilia and renal insufficiency [creatinine 5.4], responding to corticosteroid therapy; no mention of ALT elevations or hepatic involvement).
- Hewitson LJ. Vancomycin induced DRESS syndrome (drug reaction with eosinophilia and systemic symptoms) in a patient with tricuspid endocarditis. BMJ Case Rep. 2019;12:e229590. [PMC free article: PMC6754717] [PubMed: 31527200](57 year old man with infected cardiac pacemaker developed DRESS syndrome 21 days after starting vancomycin therapy with fever, rash, lymphadenopathy, eosinophilia, ALT elevations [peak 1166 U/L], epigastric pain and severe hypoxia, not improving upon stopping vancomycin but resolving rapidly with initiation of high dose prednisolone therapy).
- Zafar S, Decastro A, Pal S, Pandav J, Kanaparthy N. Vancomycin-induced DRESS syndrome. Ann Allergy Asthma Immunol. 2020;124:107–8. [PubMed: 31513907](Two cases of DRESS syndrome caused by vancomycin: 30 year old man with endocarditis and 63 year old woman with osteomyelitis developed rash, fever, and eosinophilia 4 weeks after starting vancomycin, raised ALT levels being found in one).
- Yuan K, Awan KS, Long J. Vancomycin-induced drug rash with eosinophilia and systemic symptoms (DRESS). BMJ Case Rep. 2020;13:e232302. [PMC free article: PMC7021173] [PubMed: 32024716](52 year old man with osteomyelitis developed fever, rash, and facial edema after 4 weeks of vancomycin and ertapenem therapy with subsequent eosinophilia [2026/µL], atypical lymphocytosis, elevation of serum creatinine but normal liver enzymes, responded quickly to stopping vancomycin and a course of corticosteroids).
- Mukit W, Cooper R, Moudgil H, Ahmad N. DRESS syndrome: an important differential for eosinophilia with systemic organ dysfunction. BMJ Case Rep. 2020;13:e234251. [PMC free article: PMC7222870] [PubMed: 32398248](74 year old woman with pneumonia on antibiotic therapy developed persistent fever, rash, eosinophilia, mild ALT elevations [68 U/L] and renal dysfunction starting 2 weeks after initiation of vancomycin therapy, improving with stopping and without corticosteroid therapy).
- Nakkam N, Gibson A, Mouhtouris E, Konvinse KC, Holmes N, Chua KY, Deshpande P, et al. Cross-reactivity between vancomycin, teicoplanin, and telavancin in patients with HLA-A*32:01-positive vancomycin-induced DRESS sharing an HLA class II haplotype. J Allergy Clin Immunol 2020: S0091-6749(20)30687-4. [PMC free article: PMC7674263] [PubMed: 32439433](Lymphocytes from 15 patients with a history of vancomycin induced DRESS syndrome were incubated with two different doses of vancomycin and related glycopeptide antibiotics and assessed for interferon gamma production using Elispot assays; all 15 samples had a positive response to vancomycin while only 3 reacted to telavancin and 2 to teicoplanin but none to dalbavancin, suggesting low levels of cross reactivity among the agents to inducing DRESS).
- Clark D, Alomari AK, Burton K, Rahnama-Moghadam S. A case of vancomycin-induced drug rash with eosinophilia and systemic symptoms (DRESS) syndrome with failure to respond to cyclosporine treatment. Dermatol Online J 2020;26:13030/qt1bx778dt. [PubMed: 32815686](“Young” woman with acute bacterial endocarditis being treated with vancomycin for 4 weeks underwent minimally invasive cardiac valve repair and developed facial edema the next day which worsened with high fevers and marked eosinophilia despite stopping vancomycin and starting cyclosporin, resolving rapidly when switched to methylprednisolone).
- Martel TJ, Jamil RT, King KC. Red man syndrome. 2020 Apr 27. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan–.(Review of red man syndrome, a reaction of flushing, erythema and pruritus generally arising with the first dose of vancomycin, particularly when given rapidly in high doses, probably caused by sudden degranulation of mast cells releasing bioactive amines such as histamine; the reaction may be accompanied by fatigue, back pain and angioedema but is not mediated by IgE and generally is less severe with subsequent infusions and is at least partially ameliorated by pretreatment with antihistamines).
- Austin JP, Foster BA, Empey A. Replace red man syndrome with vancomycin flushing reaction. Hosp Pediatr. 2020;10:623–4. [PubMed: 32571794](Appeal to drop the term red man syndrome, as the flushing reaction also occurs in women and in children and “red man” is an unnecessary, racially derogatory term).
- De Luca JF, Holmes NE, Trubiano JA. Adverse reactions to vancomycin and cross-reactivity with other antibiotics. Curr Opin Allergy Clin Immunol. 2020;20:352–61. [PubMed: 32590503](Review of the chemical structures, mechanisms of action and immunologic adverse reactions of vancomycin and related antibiotics, including red man syndrome, IgE mediated anaphylaxis, and T-cell mediated severe cutaneous reactions such as DRESS and SJS; there is no clear evidence for immunologic cross reactivity among the glycol- and lipoglyco-peptides).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review The use of vancomycin with its therapeutic and adverse effects: a review.[Eur Rev Med Pharmacol Sci. 2015]Review The use of vancomycin with its therapeutic and adverse effects: a review.Bruniera FR, Ferreira FM, Saviolli LR, Bacci MR, Feder D, da Luz Gonçalves Pedreira M, Sorgini Peterlini MA, Azzalis LA, Campos Junqueira VB, Fonseca FL. Eur Rev Med Pharmacol Sci. 2015 Feb; 19(4):694-700.
- Review Adverse reactions to vancomycin and cross-reactivity with other antibiotics.[Curr Opin Allergy Clin Immunol...]Review Adverse reactions to vancomycin and cross-reactivity with other antibiotics.De Luca JF, Holmes NE, Trubiano JA. Curr Opin Allergy Clin Immunol. 2020 Aug; 20(4):352-361.
- [Linezolid in the treatment of antibiotic-resistant gram-positive infections of the musculoskeletal system].[Acta Chir Orthop Traumatol Cec...][Linezolid in the treatment of antibiotic-resistant gram-positive infections of the musculoskeletal system].Jahoda D, Nyc O, Pokorný D, Landor I, Sosna A. Acta Chir Orthop Traumatol Cech. 2006 Oct; 73(5):329-33.
- Review Ceftobiprole: a review of a broad-spectrum and anti-MRSA cephalosporin.[Am J Clin Dermatol. 2008]Review Ceftobiprole: a review of a broad-spectrum and anti-MRSA cephalosporin.Zhanel GG, Lam A, Schweizer F, Thomson K, Walkty A, Rubinstein E, Gin AS, Hoban DJ, Noreddin AM, Karlowsky JA. Am J Clin Dermatol. 2008; 9(4):245-54.
- Review Ampicillin.[LiverTox: Clinical and Researc...]Review Ampicillin.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Vancomycin - LiverToxVancomycin - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...