NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Thiotepa is an intravenously or locally applied alkylating agent which is currently used in the therapy of breast, ovarian and bladder cancer. Thiotepa therapy has been associated with low rates of serum enzyme elevations during therapy and rare instances of acute, clinically apparent injury.
Background
Thiotepa (thye' oh tep' a) is an ethylenimine similar in structure and activity to altretamine and is believed to act as an alkylating agent. The alkylating agents act by causing modification and cross linking of DNA, thus inhibiting DNA, RNA and protein synthesis and causing programmed cell death (apoptosis) in rapidly dividing cells. Thiotepa was approved for use in the United States in 1959. Current indications include ovarian and breast cancer and Hodgkin disease. Thiotepa is also administered locally for bladder cancer, neoplastic effusions and malignant meningeal neoplasms. Thiotepa is available generically in vials of 15 mg. The recommended dose varies by indications, route of administration, and body weight. Thiotepa shares common side effects with other alkylating agents such as nausea, vomiting, diarrhea, alopecia, mucositis, bone marrow suppression, rash and hypersensitivity reactions. Uncommon but potentially serious adverse events include severe myelosuppression, severe infections, sepsis, bleeding, and embryo-fetal toxicity.
Hepatotoxicity
Thiotepa is associated with an appreciable rate of serum enzyme elevations during therapy, but these are generally mild and self-limited, not requiring dose adjustment. Rare instances of clinically apparent acute liver injury attributed to thiotepa have been reported, particularly with high doses. In most instances, thiotepa was administered in combination with other agents known to cause liver injury and the specific role of thiotepa was not clear.
Thiotepa is often used in combination with other alkylating agents in conditioning regimens for bone marrow ablation in preparation for hematopoietic cell transplantation and as such has been linked to instances of sinusoidal obstruction syndrome. Onset of sinusoidal obstruction syndrome is usually within 1 to 3 weeks of myeloablative or high dose therapy and is characterized by the sudden development of abdominal pain, hepatomegaly, weight gain and ascites followed by jaundice. The pattern of serum enzyme elevations is usually hepatocellular, with marked increases in serum aminotransferase and lactic dehydrogenase levels and minimal increase in alkaline phosphatase. In severe instances, there are elevations in prothrombin time and progressive hepatic failure. Immunoallergic and autoimmune features are uncommon. The fatality rate is high. Liver biopsy shows centrolobular necrosis and congestion with occlusion of small veins and red cells in sinusoids.
Likelihood score: D (possible, rare cause of clinically apparent liver injury).
Mechanism of Injury
The potential mechanism of hepatotoxicity from thiotepa is probably similar to that of other alkylating agents, a direct cytotoxic injury to rapidly dividing cells. High doses are likely to injure other cells such as sinusoidal endothelial cells and hepatocytes. The cause of the idiosyncratic liver injury associated with thiotepa is not known.
Outcome and Management
Liver injury is not uncommon with high doses of thiotepa. The severity of injury in reported cases has generally been mild-to-moderate and self-limited in course, although fatalities attributed to hepatotoxicity have been reported. The sinusoidal obstruction syndrome associated with thiotepa and other alkylating agents can be severe and lead to acute liver failure. There have been no instances of chronic hepatitis or vanishing bile duct syndrome definitely linked to thiotepa therapy. In situations of acute liver injury after thiotepa use, rechallenge should be avoided.
Drug Class: Antineoplastic Agents, Alkylating Agents
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Thiotepa – Generic, Thioplex®
DRUG CLASS
Antineoplastic Agents, Alkylating Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Thiotepa | 52-24-4 | C6-H12-N3-P-S |
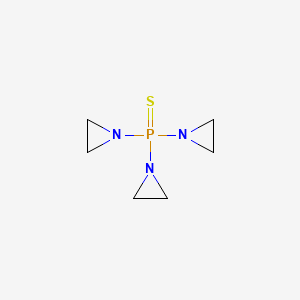
|
ANNOTATED BIBLIOGRAPHY
References updated: 12 September, 2020
- Zimmerman HJ. Oncotherapeutic and immunosuppressive agents. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 673-708.(Expert review of hepatotoxicity of cancer chemotherapeutic agents published in 1999; thiotepa has been implicated in at least one case of acute liver failure).
- DeLeve LD. Cancer chemotherapy. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 549-68.(Review of hepatotoxicity of cancer chemotherapeutic agents).
- Wellstein A, Giaccone G, Atkins MB, Sausville EA. Cytotoxic agents. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1167-201.(Textbook of pharmacology and therapeutics).
- Rollins BJ. Hepatic veno-occlusive disease. Am J Med. 1986;81:297–306. [PubMed: 3526887](Review of the diagnosis, clinical course, histology and pathogenesis of veno-occlusive disease).
- Lazarus HM, Reed MD, Spitzer TR, Rabaa MS, Blumer JL. High-dose i.v. thiotepa and cryopreserved autologous bone marrow transplantation for therapy of refractory cancer. Cancer Treat Rep. 1987;71:689–95. [PubMed: 3111687](Among 25 patients with refractory cancers treated with escalating doses of thiotepa followed by autologous bone marrow transplantation, toxicity was dose limiting and 2 had hepatotoxicity, one being fatal, but no details given).
- Jones RJ, Lee KS, Beschorner WE, Vogel VG, Grochow LB, Braine HG, Vogelsang GB, et al. Veno-occlusive disease of the liver following bone marrow transplantation. Transplantation. 1987;44:778–83. [PubMed: 3321587](Among 235 patients undergoing hematopoietic cell transplantation between 1982 and 1985, sinusoidal obstruction syndrome [SOS] developed in 52 [22%] of whom half died, making SOS the third most common cause of death in this population).
- Bearman SI. The syndrome of hepatic veno-occlusive disease after marrow transplantation. Blood. 1995;85:3005–20. [PubMed: 7756636](Review of SOS after hematopoietic cell transplantation; usually presents with painful hepatomegaly, weight gain [fluid and ascites] and jaundice within 3 weeks of myeloablation with occlusion of central veins and sinusoids and extensive zone 3 [centrolobular] injury).
- Przepiorka D, Nath R, Ippoliti C, Mehra R, Hagemeister F, Diener K, Dimopoulos M, et al. A phase I-II study of high-dose thiotepa, busulfan and cyclophosphamide as a preparative regimen for autologous transplantation for malignant lymphoma. Leuk Lymphoma. 1995;17:427–33. [PubMed: 7549833](Among 34 patients with lymphoma treated with high dose thiotepa, busulfan and cyclophosphamide with autologous hematopoietic cell transplantation, liver toxicity was common at high doses, 3 developing "centrilobular necrosis" without SOS).
- Papadakis V, Dunkel IJ, Cramer LD, Kramer E, Papadopoulos E, Goldman S, Packer RJ, et al. High-dose carmustine, thiotepa and etoposide followed by autologous bone marrow rescue for the treatment of high risk central nervous system tumors. Bone Marrow Transplant. 2000;26:153–60. [PubMed: 10918425](Among 42 patients with brain tumors who were treated with high dose carmustine, thiotepa and etoposide and autologous hematopoietic cell transplantation, 2 developed SOS and 5 had transient elevations in ALT levels).
- Lee JL, Gooley T, Bensinger W, Schiffman K, McDonald GB. Veno-occlusive disease of the liver after busulfan, melphalan, and thiotepa conditioning therapy: incidence, risk factors, and outcome. Biol Blood Marrow Transplant. 1999;5:306–15. [PubMed: 10534061](Among 253 patients who received a regimen of busulfan, melphalan and thiotepa in preparation for hematopoietic stem cell transplantation, 70 [28%] developed SOS, which was severe in 11 and fatal in 9).
- DeLeve LD, Shulman HM, McDonald GB. Toxic injury to hepatic sinusoids: sinusoidal obstruction syndrome. Semin Liver Dis. 2002;22:27–42. [PubMed: 11928077](Review of clinical features, pathology, etiology, prevention and treatment of sinusoidal obstruction syndrome, a better term for this condition than veno-occlusive disease; first described in association with exposure to phytotoxins [pyrrolizidine alkaloids], the most common cause now is cancer chemotherapy and particularly myeloablative conditioning regimens in preparation for bone marrow transplantation).
- McDonald GB. Hepatobiliary complications of hematopoietic cell transplantation, 40 years on. Hepatology. 2010;51:1450–60. [PMC free article: PMC2914093] [PubMed: 20373370](Review of liver complications of bone marrow [hematopoietic cell] transplantation, which have become less frequent with better understanding of their causes and means of prevention; the rate of sinusoidal obstruction syndrome has decreased because of avoidance of more aggressive ablative therapies [total body irradiation and high doses of cyclophosphamide] and better understanding of pharmacokinetics of the alkylating agents).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 363 [36%] were attributed to antibiotics, but none were attributed to thiotepa).
- Ferreri AJ, Cwynarski K, Pulczynski E, Ponzoni M, Deckert M, Politi LS, Torri V, et al. International Extranodal Lymphoma Study Group (IELSG). Chemoimmunotherapy with methotrexate, cytarabine, thiotepa, and rituximab (MATRix regimen) in patients with primary CNS lymphoma: results of the first randomisation of the International Extranodal Lymphoma Study Group-32 (IELSG32) phase 2 trial. Lancet Haematol. 2016;3:e217–27. [PubMed: 27132696](Among 219 patients with primary CNS lymphoma treated with methotrexate and cytarabine alone, or combined with rituximab or with rituximab and thiotepa, remission rates and survival were greatest with thiotepa while rates of hepatoxicity were slightly less [35% vs 44%]).
- Maximova N, Sonzogni A, Matarazzo L, Ghirardi A, D'Antiga L. Vanishing bile ducts in the long term after pediatric hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2018;24:2250–8. [PubMed: 30026108](Among 47 children undergoing 50 hematopoietic cell transplant [HCT] with various conditioning regimens including thiotepa [n=29], hepatic graft-vs-host disease arose in 12 [24%] overall and long term follow up with liver biopsies found bile duct loss [ductopenia] in 94% which was severe [less than 20% of portal areas with bile ducts] in 74%, slightly higher rates found in those who had received thiotepa).
- Sheth V, Nachmias B, Grisariu S, Avni B, Or R, Shapira M. Augmented myeloablative conditioning with thiotepa in acute myeloid leukemia – improved outcomes with similar toxicity. Leuk Lymphoma. 2019;60:726–33. [PubMed: 30277100](Among 89 patients with acute myelogenous leukemia undergoing HCT using conditioning regimens with busulfan and fludarabine with or without thiotepa, use of thiotepa was associated with improved 5-year survival [62% vs 38%] and lower relapse rates [8% vs 31%], but similar rates of toxicity including sinusoidal obstruction syndrome [11% vs 18%]).
- Duque-Afonso J, Ihorst G, Waterhouse M, Zeiser R, Wäsch R, Bertz H, Yücel M, et al. Comparison of reduced-toxicity conditioning protocols using fludarabine, melphalan combined with thiotepa or carmustine in allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2020 Jun 26;:1–11. Epub ahead of print. [PMC free article: PMC7319212] [PubMed: 32591641](Among 241 patients undergoing HCT for malignant disease using reduced-toxicity conditioning regimens of fludarabine and melphalan with either carmustine [BCNU] or thiotepa, long term survival rates were similar in the two groups as were rates of liver toxicity during the first 30 days [51% vs 49%]).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Altretamine.[LiverTox: Clinical and Researc...]Review Altretamine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Interaction of ultrasonic hyperthermia with two alkylating agents in a murine bladder tumor.[Cancer Res. 1983]Interaction of ultrasonic hyperthermia with two alkylating agents in a murine bladder tumor.Longo FW, Tomashefsky P, Rivin BD, Tannenbaum M. Cancer Res. 1983 Jul; 43(7):3231-5.
- Review Carboplatin.[LiverTox: Clinical and Researc...]Review Carboplatin.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Gemcitabine.[LiverTox: Clinical and Researc...]Review Gemcitabine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Protection of mammalian cells against chemotherapeutic agents thiotepa, 1,3-N,N'-bis(2-chloroethyl)-N-nitrosourea, and mafosfamide using the DNA base excision repair genes Fpg and alpha-hOgg1: implications for protective gene therapy applications.[J Pharmacol Exp Ther. 2001]Protection of mammalian cells against chemotherapeutic agents thiotepa, 1,3-N,N'-bis(2-chloroethyl)-N-nitrosourea, and mafosfamide using the DNA base excision repair genes Fpg and alpha-hOgg1: implications for protective gene therapy applications.Xu Y, Hansen WK, Rosenquist TA, Williams DA, Limp-Foster M, Kelley MR. J Pharmacol Exp Ther. 2001 Mar; 296(3):825-31.
- Thiotepa - LiverToxThiotepa - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...