NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Sorafenib is an oral multi-kinase inhibitor that is used in the therapy of advanced renal cell, liver and thyroid cancer. Sorafenib has been associated with a low rate of transient elevations in serum aminotransferase levels during therapy that are generally mild and asymptomatic. Sorafenib has also been linked to rare instances of clinically apparent liver injury which can be severe and even fatal.
Background
Sorafenib (soe raf’ e nib) is an orally available, small molecule, multi-specific tyrosine kinase inhibitor with activity against vascular endothelial growth factors (VEGF) receptors -1, -2 and -3 as well as against the receptor for platelet derived growth factor (PDGF) and several Raf kinases. Inhibition of these kinases decreases angiogenesis, which plays an important role in the growth and spread of several forms of solid tumors. Sorafenib received approval for use in the United States in 2005 for therapy of advanced renal cell carcinoma, and indications were subsequently expanded to hepatocellular carcinoma in 2007 and refractory thyroid cancer in 2014. Sorafenib is available in tablets of 200 mg under the brand name Nexavar. The typical dose is 400 mg twice daily, continued until there is tumor progression or unacceptable toxicity. Side effects are common and can include fatigue, diarrhea, anorexia, weight loss, nausea, abdominal pain, hand-foot syndrome, rash, hair loss, pruritus, bleeding and sensory neuropathy. Uncommon, but potentially severe side effects include bone marrow suppression, bleeding, venous thrombosis, gastrointestinal perforation, QTc prolongation and Stevens Johnson syndrome.
Hepatotoxicity
In large clinical trials of sorafenib, elevations in serum aminotransferase levels were common, occurring in up to half of patients, but values greater than 5 times the upper limit of normal (ULN) occurred in only 1% to 3% of treated subjects. In addition, there have been several single case reports of clinically apparent liver injury arising during sorafenib therapy which was often severe and occasionally fatal. The onset of acute liver injury ranged from a few days to 8 weeks of starting sorafenib, and the pattern of injury was typically hepatocellular with marked elevations in serum aminotransferase levels. Immunoallergic and autoimmune features were absent. Recovery was usually rapid once sorafenib was stopped, but some cases were associated with progressive liver injury and hepatic failure. Most of the reports of severe liver injury occurred in patients being treated for hepatocellular carcinoma who also had cirrhosis or in patients receiving other potentially hepatotoxic drugs31.
Likelihood score: B (likely cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism of injury accounting for serum enzyme elevations during sorafenib therapy is not known. Sorafenib is metabolized in the liver largely through the CYP 3A4 pathway and liver injury may be related to production of a toxic intermediate. Sorafenib is susceptible to drug-drug interactions with agents that inhibit or induce hepatic CYP 3A4 activity. Sorafenib, like many tyrosine kinase inhibitors can inhibit UDP glucuronosyltransferase activity which can result in mild indirect hyperbilirubinemia and may predispose to acetaminophen toxicity.
Outcome and Management
Monitoring of routine liver tests is recommended during sorafenib therapy. Serum aminotransferase elevations above 5 times the upper limit of normal (if confirmed) or any elevations accompanied by jaundice or symptoms should lead to dose reduction or temporary cessation. Sorafenib has been implicated in cases of acute liver failure, but not in instances of chronic hepatitis or vanishing bile duct syndrome. There does not appear to be cross reactivity in risk for hepatic injury between sorafenib and other kinase inhibitors including the angiogenesis inhibitors such axitinib and sunitinib.
Drug Class: Antineoplastic Agents, Protein Kinase Inhibitors
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Sorafenib – Nexavar®
DRUG CLASS
Antineoplastic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Sorafenib | 284461-73-0 | C21-H16-Cl-F3-N4-O3 |
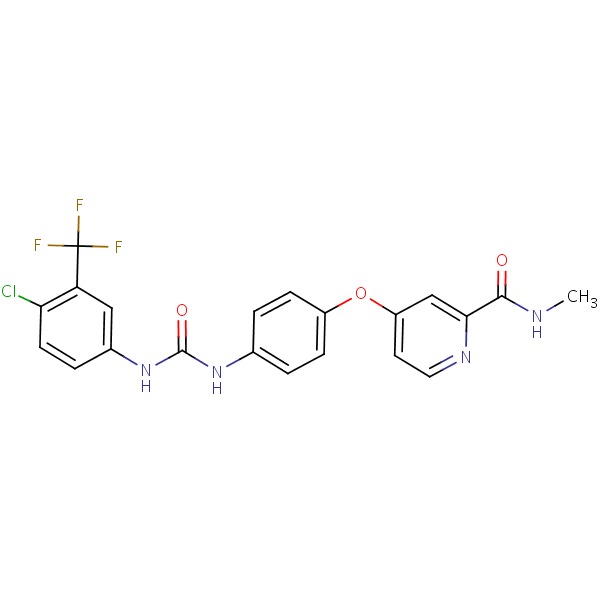 |
ANNOTATED BIBLIOGRAPHY
References updated: 22 June 2018
Abbreviations: HCC, hepatocellular carcinoma; NSCLC, non-small cell lung cancer.
- Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999.(Review of hepatotoxicity published in 1999 before the availability of tyrosine kinase receptor inhibitors such as sorafenib).
- DeLeve LD. Cancer chemotherapy. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 541-67.(Review of hepatotoxicity of cancer chemotherapeutic agents; imatinib, gefitinib, erlotinib and crizotinib are discussed, but not sorafenib).
- Chabner BA, Barnes J, Neal J, Olson E, Mujagic H, Sequist L, Wilson W, et al. Targeted therapies: tyrosine kinase inhibitors, monoclonal antibodies, and cytokines. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1731-54.(Textbook of pharmacology and therapeutics).
- Elser C, Siu LL, Winquist E, Agulnik M, Pond GR, Chin SF, Francis P, et al. Phase II trial of sorafenib in patients with recurrent or metastatic squamous cell carcinoma of the head and neck or nasopharyngeal carcinoma. J Clin Oncol 2007; 25: 3766-73. [PubMed: 17704426](Among 27 patients with refractory head and neck cancers treated with sorafenib, the median survival was 4.2 months; side effects included fatigue, stomatitis, hypertension, hand foot syndrome and neuropathy, with mild AST elevations in 26% of patients and no clinically apparent liver injury).
- Schramm C, Schuch G, Lohse AW. Sorafenib-induced liver failure. Am J Gastroenterol 2008; 103: 2162-3. [PubMed: 18796127](65 year old woman with hepatocellular cancer [HCC] and cirrhosis due to nonalcoholic steatohepatitis developed jaundice 6 weeks after starting sorafenib [bilirubin 22 mg/dL, AST 1724 U/L, INR 2.9], with progressive liver failure, but prompt resolution after initiation of prednisolone).
- Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, Luo R, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol 2009; 10: 25-34. [PubMed: 19095497](Among 271 Asian patients with HCC, median survival was 6.5 months in those treated with sorafenib vs 4.2 with placebo, and adverse events included hand-foot syndrome [45%], diarrhea [25%], fatigue [20%], rash [20%] and hypertension [19%], with no increase in "liver dysfunction" with sorafenib and no treatment related deaths).
- Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, et al.; SHARP Investigators Study Group. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008; 359: 378-90. [PubMed: 18650514](In a study of 602 patients with advanced HCC, sorafenib treatment [in comparison to placebo] increased median survival from 7.9 to 10.7 months, but was also associated with higher rate of adverse events including fatigue, anorexia, diarrhea, weight loss, alopecia, and hand-foot syndrome, but not "liver dysfunction" [<1% vs 0%]).
- Gupta-Abramson V, Troxel AB, Nellore A, Puttaswamy K, Redlinger M, Ransone K, Mandel SJ, et al. Phase II trial of sorafenib in advanced thyroid cancer. J Clin Oncol 2008; 26: 4714-9. [PMC free article: PMC2653134] [PubMed: 18541894](Among 30 patients with advanced thyroid cancer treated with sorafenib, elevated liver tests occurred in 4 patients, one of whom developed marked elevations starting at 8 weeks and died of liver failure 3 months later).
- Di Lorenzo G, Cartenì, Autorino R, Bruni G, Tudini M, Rizzo M, Aieta M, et al. Phase II study of sorafenib in patients with sunitinib-refractory metastatic renal cell cancer. J Clin Oncol 2009; 27: 4469-74. [PubMed: 19652053](Among 52 patients with refractory renal cell cancer treated with sorafenib for 1-10 months, clinical responses were infrequent, but side effects were common including fatigue, diarrhea, neutropenia, nausea, anemia, rash and thrombocytopenia; ALT elevations occurred in 6%, but all were ≤5 times ULN).
- Escudier B, Eisen T, Stadler WM, Szczylik C, Oudard S, Staehler M, Negrier S, et al. Sorafenib for treatment of renal cell carcinoma: Final efficacy and safety results of the phase III treatment approaches in renal cancer global evaluation trial. J Clin Oncol 2009; 27: 3312-8. [PubMed: 19451442](Among 903 patients with advanced renal cell cancer treated with sorafenib or placebo, the median overall survival was similar in both groups [17.8 vs 15.2 months], but side effects more common with sorafenib were diarrhea [48% vs 11%], rash [41% vs 13%], hand-foot syndrome [33% vs 8%], fatigue [29% vs 16%], nausea [19% vs 12%]; ALT elevations and hepatotoxicity were not mentioned).
- Llanos L, Bellot P, Zapater P, Perez-Mateo M, Such J. Acute hepatitis in a patient with cirrhosis and hepatocellular carcinoma treated with sorafenib. Am J Gastroenterol 2009; 104: 257-8. [PubMed: 19098892](73 year old man with recurrence of HCC after liver transplantation developed jaundice 4 days after starting sorafenib [bilirubin 2.8 rising to ~12 mg/dL, ALT 109 U/L, Alk P not given, INR 1.48], resolving within 6 weeks of onset).
- Wörns MA, Weinmann A, Pfingst K, Schulte-Sasse C, Messow CM, Schulze-Bergkamen H, Teufel A, et al. Safety and efficacy of sorafenib in patients with advanced hepatocellular carcinoma in consideration of concomitant stage of liver cirrhosis. J Clin Gastroenterol 2009; 43: 489-95. [PubMed: 19247201](Among 34 patients with advanced HCC and cirrhosis treated with sorafenib, 53% developed liver dysfunction [bilirubin elevations, asterixis, liver failure] usually within a few weeks of starting, which was more frequent and severe in those with more advanced stages of cirrhosis [Child classes B and C]).
- Stadler WM, Figlin RA, McDermott DF, Dutcher JP, Knox JJ, Miller WH Jr, Hainsworth JD, et al.; ARCCS Study Investigators. Safety and efficacy results of the advanced renal cell carcinoma sorafenib expanded access program in North America. Cancer 2010; 116: 1272-80. [PubMed: 20082451](Among 2504 patients with advanced renal cell cancer treated with sorafenib in an open access program, common side effects were hand-foot syndrome [18%], rash, hypertension and fatigue; ALT elevations and hepatotoxicity were not mentioned).
- Herden U, Fischer L, Schäfer H, Nashan B, von Baehr V, Sterneck M. Sorafenib-induced severe acute hepatitis in a stable liver transplant recipient. Transplantation 2010; 90: 98-9. [PubMed: 20606568](58 year old man with HCC after liver transplant developed nausea and fever 5 days after starting sorafenib [bilirubin 12.0, ALT 893 U/L, GGT 726 U/L], with resolution within 8 weeks of stopping).
- Hutson TE, Bellmunt J, Porta C, Szczylik C, Staehler M, Nadel A, Anderson S, et al.; Sorafenib TARGET Clinical Trial Group. Long-term safety of sorafenib in advanced renal cell carcinoma: follow-up of patients from phase III TARGET. Eur J Cancer 2010; 46: 2432-40. [PubMed: 20656473](Analysis of patients with advanced renal cancer who were treated with sorafenib for more than one year found adverse events were most frequent during the first 3 months of treatment [particularly rash and hand-foot syndrome]; ALT elevations and hepatotoxicity were not mentioned).
- Rini BI, Escudier B, Tomczak P, Kaprin A, Szczylik C, Hutson TE, Michaelson MD, et al. Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (AXIS): a randomised phase 3 trial. Lancet 2011; 378 (9807): 1931-9. [PubMed: 22056247](Among 723 patients with advanced renal cell carcinoma, progression free survival was longer with axitinib [6.7 months] than sorafenib [4.7 months] and side effects were common, although rates of hepatotoxicity or ALT elevations were not provided).
- Beck J, Procopio G, Bajetta E, Keilholz U, Negrier S, Szczylik C, Bokemeyer C, et al. Final results of the European Advanced Renal Cell Carcinoma Sorafenib (EU-ARCCS) expanded-access study: a large open-label study in diverse community settings. Ann Oncol 2011; 22: 1812-23. [PubMed: 21324953](Among 1159 patients with advanced renal cell cancer treated with sorafenib in an open access program, adverse events occurred in 94% of patients, most frequently hand-foot syndrome [56%], rash [33%], alopecia [33%], fatigue [34%], diarrhea [55%] and hypertension [20%]; rates of ALT elevations and hepatotoxicity were not mentioned).
- Fairfax BP, Pratap S, Roberts IS, Collier J, Kaplan R, Meade AM, Ritchie AW, et al. Fatal case of sorafenib-associated idiosyncratic hepatotoxicity in the adjuvant treatment of a patient with renal cell carcinoma. BMC Cancer 2012; 12: 590. [PMC free article: PMC3575366] [PubMed: 23231599](62 year old man with renal cell cancer developed fatigue at 4 and jaundice by 7 weeks after starting sorafenib [bilirubin 16.8 mg/dL, ALT 6935 U/L, Alk P 577 U/L], with progressive liver failure and death).
- Raoul JL, Bruix J, Greten TF, Sherman M, Mazzaferro V, Hilgard P, Scherubl H, et al. Relationship between baseline hepatic status and outcome, and effect of sorafenib on liver function: SHARP trial subanalyses. J Hepatol 2012; 56: 1080-8. [PubMed: 22245896](Among 602 patients with HCC treated with sorafenib or placebo, survival was shorter among those with raised baseline levels liver tests, but levels were not altered by sorafenib therapy compared to placebo, although total and direct serum bilirubin levels with increased during the second month of sorafenib therapy).
- Motzer RJ, Escudier B, Tomczak P, Hutson TE, Michaelson MD, Negrier S, Oudard S, et al. Axitinib versus sorafenib as second-line treatment for advanced renal cell carcinoma: overall survival analysis and updated results from a randomised phase 3 trial. Lancet Oncol 2013; 14: 552-62. [PubMed: 23598172](Among 723 patients with metastatic renal cell cancer treated with either axitinib or sorafenib, median overall survivals were similar with both agents [20.1 vs 19.2 months] and side effects common; no mention of ALT elevations or hepatotoxicity).
- Herzog TJ, Scambia G, Kim BG, Lhommé C, Markowska J, Ray-Coquard I, Sehouli J, et al. A randomized phase II trial of maintenance therapy with Sorafenib in front-line ovarian carcinoma. Gynecol Oncol 2013; 130: 25-30. [PubMed: 23591401](Among 246 women with ovarian carcinoma treated with sorafenib or placebo, progression free survival was similar in both groups, whereas side effects were more common with sorafenib [67% vs 15%]; ALT elevations and hepatotoxicity were not mentioned).
- Hutson TE, Lesovoy V, Al-Shukri S, Stus VP, Lipatov ON, Bair AH, Rosbrook B, et al. Axitinib versus sorafenib as first-line therapy in patients with metastatic renal-cell carcinoma: a randomised open-label phase 3 trial. Lancet Oncol 2013; 14: 1287-94. [PubMed: 24206640](Among 288 patients with metastatic renal cell carcinoma treated with either axitinib or sorafenib, progression free survival was similar in the two groups; side effects of diarrhea, hypertension, anorexia, weight loss and hoarseness were more common with axitinib; rates of ALT elevations and hepatotoxicity were not reported).
- Shah RR, Morganroth J, Shah DR. Hepatotoxicity of tyrosine kinase inhibitors: clinical and regulatory perspectives. Drug Saf 2013; 36: 491-503. [PubMed: 23620168](Review of the hepatotoxicity of 18 tyrosine kinase inhibitors approved for use in cancer in the US as of 2013; sorafenib has been reported to cause ALT elevations in 21-24% of patients [≥5 times ULN in 2%] and has been linked to clinically apparent liver injury is several isolated case reports).
- Brose MS, Nutting CM, Jarzab B, Elisei R, Siena S, Bastholt L, de la Fouchardiere C, et al.; on behalf of the DECISION investigators. Sorafenib in radioactive iodine-refractory, locally advanced or metastatic differentiated thyroid cancer: a randomised, double-blind, phase 3 trial. Lancet 2014; 384: 319-28. [PMC free article: PMC4366116] [PubMed: 24768112](Among 417 patients with advanced thyroid cancer, median progression free survival was 10.8 months in sorafenib- vs 5.8 months in placebo-treated patients, but side effects occurred in 99%, including hand-foot syndrome [76%], diarrhea [69%], rash [50%]; rates of ALT elevations and hepatotoxicity were not provided).
- Sorafenib (Nexavar) for thyroid cancer. Med Lett Drugs Ther 2014; 56 (1443): 43-4. [PubMed: 24869715](Concise review of the efficacy, safety and costs of sorafenib in advanced thyroid cancer shortly after its approval for this use in the US, mentions that sorafenib can cause severe liver injury).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 49 [6%] were attributed to antineoplastic agents including 9 to kinase inhibitors including imatinib [n=5], lapatinib [n=2] and regorafinib [n=1], but none were attributed to sorafenib).
- Paz-Ares L, Hirsh V, Zhang L, de Marinis F, Yang JC, Wakelee HA, Seto T, et al. Monotherapy administration of sorafenib in patients with non-small cell lung cancer (MISSION) trial: a phase III, multicenter, placebo-controlled trial of sorafenib in patients with relapsed or refractory predominantly nonsquamous non-small-cell lung cancer after 2 or 3 previous treatment regimens. J Thorac Oncol 2015; 10: 1745-53. [PubMed: 26743856](Among 703 patients with advanced refractory or relapsed NSCLC who were treated with sorafenib vs placebo, median overall survival was similar in the two groups [8.2 vs 8.3 months] and side effects were more common with sorafenib [88% vs 49%], including rash [41% vs 4%] fatigue [36% vs 8%], diarrhea [36% vs 3%]; ALT elevations and liver related adverse events not mentioned).
- Bruix J, Takayama T, Mazzaferro V, Chau GY, Yang J, Kudo M, Cai J, et al.; STORM investigators. Adjuvant sorafenib for hepatocellular carcinoma after resection or ablation (STORM): a phase 3, randomised, double-blind, placebo-controlled trial. Lancet Oncol 2015; 16: 1344-54. [PubMed: 26361969](Among 1114 patients with HCC, after successful resection or ablation, who were treated with sorafenib vs placebo for up to 4 years, recurrence free survival was simliar in the 2 groups [33 vs 34 months], while side effects were greater with sorafenib including hand-foot skin reaction [28% vs <1%], and ALT elevations [9% vs 7%] which were above 5 times ULN in 5% vs 2% and were associated with fatalities in 3 vs no patients [<1% vs 0%]).
- Shantakumar S, Nordstrom BL, Djousse L, Hall SA, Gagnon DR, Fraeman KH, van Herk-Sukel M, et al. Occurrence of hepatotoxicity with pazopanib and other anti-VEGF treatments for renal cell carcinoma: an observational study utilizing a distributed database network. Cancer Chemother Pharmacol 2016; 78: 559-66. [PMC free article: PMC5010603] [PubMed: 27438066](Review of hepatotoxicity associated with anti-VEGF treatments of renal cell cancer from two large US health care databases, highest rates of ALT elevations were found with first line treatment with pazopanib [n=180] and slightly lower rates for sorafenib [n=160], sunitinib [n=721] and bevacizumab [n=83], but clinically apparent injury with jaundice was rare [1 case with sorafenib, 2 with sunitinib]).
- Meyer T, Fox R, Ma YT, Ross PJ, James MW, Sturgess R, Stubbs C, et al. Sorafenib in combination with transarterial chemoembolisation in patients with unresectable hepatocellular carcinoma (TACE 2): a randomised placebo-controlled, double-blind, phase 3 trial. Lancet Gastroenterol Hepatol 2017; 2: 565-75. [PubMed: 28648803](Among 313 patients with unresectable HCC who were treated with sorafenib or placebo combined with transarterial chemoembolization, median progression free survival was similar in the 2 groups [238 vs 235 days] while adverse event rates were greater with sorafenib, including 3 treatment related deaths, two due to liver failure).
- Bunchorntavakul C, Reddy KR. Drug hepatotoxicity: newer agents. Clin Liver Dis 2017; 21: 115-34. [PubMed: 27842767](Overview of hepatotoxicity of newer agents including tyrosine kinase inhibitors such as imatinib, bosutinib, nilotinib, ponatinib and sorafenib, all of which have been implicated in causing ALT and AST elevations [in 23-50% of patients] as well as clinically apparent liver injury).
- Kudo M, Ueshima K, Yokosuka O, Ogasawara S, Obi S, Izumi N, Aikata H, et al.; SILIUS study group. Sorafenib plus low-dose cisplatin and fluorouracil hepatic arterial infusion chemotherapy versus sorafenib alone in patients with advanced hepatocellular carcinoma (SILIUS): a randomised, open label, phase 3 trial. Lancet Gastroenterol Hepatol 2018; 3: 424-32. [PubMed: 29631810](Among 206 patients with advanced HCC treated with sorafenib alone vs sorafenib with hepatic arterial infusions with cisplatin and fluorouracil, mean overall survival was similar in the two groups [11.8 vs 11.5 months] and adverse event rates were similar, ALT elevations arising in 67% vs 68% and to above 5 times ULN in 30% vs 29%).
- Kudo M, Finn RS, Qin S, Han KH, Ikeda K, Piscaglia F, Baron A, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet 2018; 391: 1163-73. [PubMed: 29433850](Among 954 patients with unresectable HCC treated with sorafenib vs lenvatinib, median survival times were similar [12.3 vs 13.6 months] while adverse event profiles were different, but serious treatment related events were less with sorafenib [10% vs 18%] as were treatment related fatalities [4, 1% vs 11, 2%], of which 3 lenvatinib but no sorafenib related deaths were due to hepatic failure).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Axitinib.[LiverTox: Clinical and Researc...]Review Axitinib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Pazopanib.[LiverTox: Clinical and Researc...]Review Pazopanib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Crizotinib.[LiverTox: Clinical and Researc...]Review Crizotinib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Regorafenib.[LiverTox: Clinical and Researc...]Review Regorafenib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Sunitinib.[LiverTox: Clinical and Researc...]Review Sunitinib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Sorafenib - LiverToxSorafenib - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...