NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Pramipexole is a selective dopamine receptor agonist used in the therapy of Parkinson disease. Pramipexole therapy is associated with a low rate of transient serum enzyme elevations during treatment, but has not been implicated in cases of clinically apparent acute liver injury.
Background
Pramipexole (pram" i pex' ole) is synthetic, nonergot derivative and dopamine receptor agonist that has selective activity for the D2 class of dopamine receptors and little agonist activity for the D1 class. For this reason, pramipexole may be better tolerated than bromocriptine or pergolide which have activity for both D1 and D2 receptors. Pramipexole was approved for use in the United States in 1997 for the therapy of symptomatic Parkinson disease. Pramipexole is available in tablets of 0.125, 0.25, 0.5, 1 and 1.5 mg generically and under the brand name of Miraplex. It is used often, but not always in combination with levodopa/carbidopa. Pramipexole is typically initiated in low doses (0.375 mg in 3 divided doses daily), with adjustment upwards based upon tolerance and clinical effects. The typical maintenance dose for Parkinson disease is 1.5 to 4.5 mg daily in three divided doses. Pramipexole can be initiated more quickly than bromocriptine or pergolide, and does not cause the profound hypotension and nausea that are typical of the ergot derivatives. Common side effects include somnolence, fatigue, vivid dreams, anxiety, confusion, depression, dizziness, headache and gastrointestinal upset.
Hepatotoxicity
Pramipexole has been reported to cause serum aminotransferase elevations in a small proportion of patients, but these abnormalities are usually mild, asymptomatic and self-limiting even without dose adjustment. Pramipexole has not been implicated in cases of clinically apparent acute liver injury which must be rare, if it occurs at all.
Likelihood score: E (unlikely cause of clinically apparent liver injury).
Mechanism of Injury
Pramipexole is minimally metabolized by the liver and is excreted largely unchanged in the urine.
Outcome and Management
Instances of liver injury attributed to pramipexole have been mild, asymptomatic and self-limiting. No instances of acute liver failure or chronic injury have been reported.
Drug Class: Antiparkinson Agents
Other Drugs in the Subclass, Dopamine Receptor Agonists: Apomorphine, Bromocriptine, Pergolide, Ropinirole, Rotigotine
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Pramipexole – Generic, Mirapex®
DRUG CLASS
Antiparkinson Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Pramipexole | 104632-26-0 | C10-H17-N3-S |
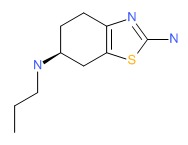 |
REFERENCES
References updated: 20 July 2017
- Zimmerman HJ. Antiparkinsonism drugs. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 715-7.(Expert review of hepatotoxicity published in 1999; among anticholinergic agents, "only trihexyphenidyl has been incriminated in hepatic injury"; other antiparkinsonism drugs discussed include levodopa, lergotrile [no longer available], pergolide and bromocriptine).
- Larrey D, Ripault MP. Hepatotoxicity of psychotropic drugs and drugs of abuse. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier Inc, 2013, pp. 443-62.(Review of hepatotoxicity of agents acting on the central nervous system).
- Standaert DG, Roberson ED. Treatment of central nervous system degenerative disorders. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 609-28.(Textbook of pharmacology and therapeutics).
- McDowell F. Symposium on levodopa in Parkinson's disease. Clinical and pharmacological aspects. Clinical laboratory abnormalities. Clin Pharmacol Ther 1971; 12: 335-9. [PubMed: 4102803](Retrospective analysis of laboratory abnormalities arising in 974 patients with Parkinson disease treated with levodopa; AST elevations occurred in 9% of 5427 determinations, but were usually mild and transient returning to normal in 1-2 months without dose adjustment; AST levels rose to 1600 U/L in one patient who later died of complications of diabetes).
- Hubble JP, Koller WC, Cutler NR, Sramek JJ, Friedman J, Goetz C, Ranhosky A, et al. Pramipexole in patients with early Parkinson's disease. Clin Neuropharmacol 1995; 18: 338-47. [PubMed: 8665547](55 patients with early Parkinson disease where treated with selegiline and either pramipexole or placebo for 9 weeks; one patient in each group had an asymptomatic, isolated elevation in AST).
- Lieberman A, Ranhosky A, Korts D. Clinical evaluation of pramipexole in advanced Parkinson's disease: results of a double-blind, placebo-controlled, parallel-group study. Neurology 1997; 49: 162-8. [PubMed: 9222185](Among 360 patients with advanced Parkinson disease on levodopa/carbidopa treated with pramipexole or placebo, side effects were similar in the two groups; no mention of ALT abnormalities or hepatotoxicity).
- Shannon KM, Bennett JP Jr., Friedman JH. Efficacy of pramipexole, a novel dopamine agonist, as monotherapy in mild to moderate Parkinson's disease. The Pramipexole Study Group. Neurology 1997; 49: 724-8. [PubMed: 9305331](In a controlled trial of pramipexole vs placebo in 335 patients with early Parkinson disease not receiving levodopa, there were no significant changes in serum chemistry test results in either group).
- Lambert D, Waters CH. Comparative tolerability of the newer generation antiparkinsonian agents. Drugs Aging 2000; 16: 55-65. [PubMed: 10733264](Review of mechanism of action, tolerability and safety of selegiline, pramipexole, ropinirole, tolcapone and entacapone in Parkinson disease).
- Reuben A, Koch DG, Lee WM; Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology 2010; 52: 2065-76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, but none were attributed to agents used for Parkinson disease).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation, and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 2013; 144: 1419-25,1425. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, but none of the 96 were attributed to an agent used to treat Parkinson disease).
- Drugs for Parkinson's disease. Treat Guidel Med Lett 2013; 11 (135): 101-6. [PubMed: 24165688](Concise review of recommendations for therapy of Parkinson disease with description of mechanisms of action, efficacy and adverse events).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America: an analysis of published reports. Ann Hepatol 2014; 13: 231-9. [PubMed: 24552865](Among 176 reports of drug induced liver injury from Latin America published between 1996 and 2012, none were attributed to an agent to treat Parkinson disease).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury from the US enrolled in a prospective database between 2004 and 2012, none were attributed to an agent used to treat Parkinson disease).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Novel neuroprotective mechanisms of pramipexole, an anti-Parkinson drug, against endogenous dopamine-mediated excitotoxicity.[Eur J Pharmacol. 2007]Novel neuroprotective mechanisms of pramipexole, an anti-Parkinson drug, against endogenous dopamine-mediated excitotoxicity.Izumi Y, Sawada H, Yamamoto N, Kume T, Katsuki H, Shimohama S, Akaike A. Eur J Pharmacol. 2007 Feb 28; 557(2-3):132-40. Epub 2006 Nov 14.
- Switching from pergolide to pramipexole in patients with Parkinson's disease.[J Neural Transm (Vienna). 2001]Switching from pergolide to pramipexole in patients with Parkinson's disease.Hanna PA, Ratkos L, Ondo WG, Jankovic J. J Neural Transm (Vienna). 2001; 108(1):63-70.
- Review Pramipexole--a new dopamine agonist for the treatment of Parkinson's disease.[J Neurol Sci. 1999]Review Pramipexole--a new dopamine agonist for the treatment of Parkinson's disease.Bennett JP Jr, Piercey MF. J Neurol Sci. 1999 Feb 1; 163(1):25-31.
- Review Parkinson's disease treatment may cause impulse-control disorder via dopamine D3 receptors.[Synapse. 2015]Review Parkinson's disease treatment may cause impulse-control disorder via dopamine D3 receptors.Seeman P. Synapse. 2015 Apr; 69(4):183-9. Epub 2015 Feb 3.
- Low dose pramipexole is neuroprotective in the MPTP mouse model of Parkinson's disease, and downregulates the dopamine transporter via the D3 receptor.[BMC Biol. 2004]Low dose pramipexole is neuroprotective in the MPTP mouse model of Parkinson's disease, and downregulates the dopamine transporter via the D3 receptor.Joyce JN, Woolsey C, Ryoo H, Borwege S, Hagner D. BMC Biol. 2004 Oct 11; 2:22. Epub 2004 Oct 11.
- Pramipexole - LiverToxPramipexole - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...