NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Pantoprazole is a proton pump inhibitor (PPI) and a potent inhibitor of gastric acidity which is widely used in the therapy of gastroesophageal reflux and peptic ulcer disease. Pantoprazole therapy is associated with a low rate of transient and asymptomatic serum aminotransferase elevations and is a rare cause of clinically apparent liver injury.
Background
Pantoprazole, (pan toe' pra zole) like other PPIs, blocks gastric acid production by binding to and inactivating the H+/K+-ATPase of gastric parietal cells, causing inhibition of the proton pump that transports H+ into the gastric lumen, the final common step in gastric acid production. Pantoprazole is a prodrug and is converted to the active form in the acidic secretory canaliculi of parietal cells. Because the inhibition is irreversible, acid secretion is suppressed for 24 to 48 hours, until new proton pump molecules have been synthesized and transported to the cell membrane. Pantoprazole was the fourth PPI approved for use in the United States (2000) and now is in wide use. Pantoprazole is available as delayed release tablets of 20 and 40 mg, and in 40 mg vials for parenteral use generically and under the brand name of Protonix. The typical dose of pantoprazole for peptic ulcer disease is 40 mg once daily for 4 to 8 weeks with similar long term maintenance doses. Twice daily doses are recommended for more severe cases of gastrointestinal reflux and peptic ulcer disease, and doses of up to 240 mg daily for Zollinger-Ellison syndrome. Pantoprazole is very well tolerated. Side effects are uncommon and usually mild, and include diarrhea, nausea, vomiting, abdominal discomfort, flatulence, skin rash, headaches and dizziness. Severe adverse events are rare but can include hypersensitivity reactions. Long-term use may be associated with bone fractures, acute interstitial nephritis, lupus erythematosus, vitamin B12 deficiency and hypomagnesemia.
Hepatotoxicity
Despite its wide use, pantoprazole has only rarely been associated with hepatic injury. In large scale, long term trials of pantoprazole, serum ALT elevations have occurred in less than 1% of patients and at rates similar to those that occur with placebo or comparator drugs. Only a small number of cases of clinically apparent liver disease attributed to pantoprazole have been published, but the clinical pattern of injury has resembled acute hepatic necrosis which has been described with other proton pump inhibitors. Clinically apparent liver injury due to proton pump inhibitors generally arises within the first 4 weeks of therapy and is characterized by an acute hepatocellular pattern of injury with rapid recovery upon withdrawal. Rash, fever and eosinophilia are rare, as is autoantibody formation. In large case series of drug induced liver injury, pantoprazole has accounted for few instances of symptomatic acute liver injury.
Likelihood score: C (probable rare cause of clinically apparent liver injury).
Mechanism of Injury
The acute onset and rapid recurrence of hepatic injury with proton pump inhibitors suggests a hypersensitivity reaction, but may merely reflect altered metabolism or acute toxicity of a metabolic byproduct. Pantoprazole is metabolized predominantly by hepatic CYP 2C19 with lesser metabolism by CYP 3A4. Drug interactions may occur with agents that share these pathways of metabolism.
Outcome and Management
The mild and asymptomatic elevations in serum aminotransferase that have been observed during pantoprazole therapy are usually transient and may resolve even without dose modification. Clinically apparent liver injury due to pantoprazole is rare, but calls for prompt withdrawal of the agent. Cases of acute liver failure due to proton pump inhibitors have been described, but are exceedingly rare. There is no information about cross reactivity among the various PPIs after pantoprazole hepatotoxicity, but the PPIs all share a benzimidazole structure, and caution should be used in attempting to reintroduce another PPI after clinically apparent PPI associated hepatic injury.
Drug Class: Antiulcer Agents
Other Drugs in the Subclass, Proton Pump Inhibitors: Dexlansoprazole, Esomeprazole, Lansoprazole, Omeprazole, Rabeprazole
CASE REPORT
Case 1. Acute liver injury due to pantoprazole.
[Modified from: Cordes A, Vogt W, Maier KP. [Pantoprazole-induced hepatitis]. Dtsch Med Wochenschr 2003; 128: 611-4. German. PubMed Citation]
A 46 year old woman with symptoms of gastroesophageal reflux developed epigastic pain 8 days after starting pantoprazole. She denied jaundice, dark urine, fever, rash or poor appetite. She had no history of liver disease, jaundice, alcohol abuse or risk factors for viral hepatitis. She took no other medications. Her serum aminotransferase levels had been normal 3 days previously when she underwent a routine upper endoscopy under midazolam anesthesia (which showed changes suggestive of gastroesophageal reflux disease). On examination, she had no fever, jaundice, rash, hepatomegaly or tenderness. Laboratory tests showed moderate elevations in serum aminotransferase levels and bilirubin of 1.0 mg/dL (Table). The alkaline phosphatase levels were normal, but lactic dehydrogenase was slightly elevated (LDH 686 U/L, normal <240). The white blood cell count was normal without eosinophilia. Tests for hepatitis A, B and C and for autoantibodies were negative. An ultrasound showed a gallstone without evidence of biliary obstruction. Pantoprazole was stopped. Serum bilirubin and ALT levels rose for a day and then began to fall and were near normal one week later. A liver biopsy was not done and she was not reexposed to pantoprazole or other proton pump inhibitors.
Key Points
| Medication: | Pantoprazole (dose not given) |
| Pattern: | Hepatocellular (R=37) |
| Severity: | 3+ (jaundice, hospitalization) |
| Latency: | 8 days to onset of symptoms, 9 days to jaundice |
| Recovery: | ~2 weeks |
| Other medications: | Intravenous midazolam, 3 days before onset |
Laboratory Values
* Values estimated from Figure 1.
Comment
This patient developed a mild hepatitis-like syndrome within 8-9 days of starting pantoprazole. The pattern of serum enzyme elevations was hepatocellular, but the LDH elevation suggested an acute hepatic necrosis-like clinical picture, which was further supported by the rapidity of improvement on stopping pantoprazole. Other possibilities were that the injury was due to midazolam anesthesia or to an undocumented episode of hypotension during the upper endoscopy, but both of those possibilities are unlikely. The signature pattern of short latency to onset of an acute hepatic necrosis with prompt improvement on stopping is typical of proton pump associated hepatotoxicity.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Pantoprazole – Generic, Protonix®
DRUG CLASS
Antiulcer Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Pantoprazole | 102625-70-7 | C16-H15-F2-N3-O4-S |
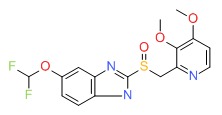 |
ANNOTATED BIBLIOGRAPHY
References updated: 15 April 2019
Abbreviations: PPI, proton pump inhibitors
- Zimmerman HJ. Proton pump inhibitors. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 720-1.(Expert review of hepatotoxicity published in 1999 states that aminotransferase elevations occur in ~1% of PPI treated patients and only 1 case of acute liver injury reported with omeprazole, none with the more recently released lansoprazole and pantoprazole).
- Sharkey KA, McNaughton WK. Pharmacotherapy of gastric acidity, peptic ulcers, and gastroesophageal reflux disease. In, Brunton LL,Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 921-44.(Textbook of pharmacology and therapeutics).
- Arnold R. Safety of proton pump inhibitors--an overview. Aliment Pharmacol Ther 1994; 8 Suppl 1: 65-70. [PubMed: 8180297](Side effects of PPIs are uncommon and no more frequent than with cimetidine and ranitidine; "Omeprazole had no clinically relevant effects on laboratory values including...liver function").
- Yusoff IF, Nairn P, Morgan CA. Multiple organ failure related to pantoprazole. Aust N Z J Med 1999; 9: 33-4. [PubMed: 10677134](68 year old with ulcer disease developed muscle aches, shortness of breath and abdominal pain 2 days after being switched from famotidine to pantoprazole [bilirubin 4.1 mg/dL, ALT 4080 U/L, Alk P 261 U/L, CPK 12,210 U/L, INR 3.1, lactate 7 mmol, creatinine 4.1 mg/dL], recovered within 2 weeks of stopping).
- Reilly JP. Safety profile of the proton-pump inhibitors. Am J Health Syst Pharm 1999; 56 (23 Suppl 4): S11-7. [PubMed: 10597119](Review of side effects of proton pump inhibitors including long term tolerance).
- Martin RM, Dunn NR, Freemantle S, Shakir S. The rates of common adverse events reported during treatment with proton pump inhibitors used in general practice in England: cohort studies. Br J Clin Pharmacol 2000; 50: 366-72. [PMC free article: PMC2014999] [PubMed: 11012560](Prescription event monitoring of common side effects of omeprazole, lansoprazole and pantoprazole from the UK found low rates of diarrhea [0.18-0.39/1000 days], abdominal pain [0.17-.21], nausea [0.16-0.22] and headache [0.10-0.17]; no analysis of liver toxicities).
- Wilton LV, Key C, Shakir SA. The pharmacovigilance of pantoprazole: the results of postmarketing surveillance on 11 541 patients in England. Drug Saf 2003; 26: 121-32. [PubMed: 12534328](Prescription event monitoring among general practitioners in the UK during 6 months after launch of pantoprazole found low rate of adverse events, most common being diarrhea, nausea, headache and dizziness; among 12,521 forms returned, were 8 cases of jaundice and 2 of abnormal liver tests, but no details provided).
- Cordes A, Vogt W, Maier KP. [Pantoprazole-induced hepatitis]. Dtsch Med Wochenschr 2003; 128: 611-4. German. [PubMed: 12649798](46 year old developed abdominal pain 8 days after starting pantoprazole [bilirubin <1.0 mg/dL, ALT 359 U/L, Alk P normal], resolving within 12 days of stopping: Case 1).
- Wellhöfer B. [Pantoprazole-induced hepatitis]. Dtsch Med Wochenschr 2003; 128: 1502; author reply 1502. German. [PubMed: 12840780](Letter in response to Cordes [2003] suggesting that the hepatic injury may have been due to cholelithiasis and would have warranted endoscopic retrograde pancreatocholangiography).
- Russo MW, Galanko JA, Shrestha R, Fried MW, Watkins P. Liver transplantation for acute liver failure from drug-induced liver injury in the United States. Liver Transpl 2004; 10: 1018-23. [PubMed: 15390328](Among ~50,000 liver transplants reported to UNOS between 1990 and 2002, 270 [0.5%] were done for drug induced acute liver failure, but none were attributed to an H2 blocker or proton pump inhibitor).
- de Abajo FJ, Montero D, Madurga M, García Rodríguez LA. Acute and clinically relevant drug-induced liver injury: a population based case-control study. Br J Clin Pharmacol 2004; 58: 71-80. [PMC free article: PMC1884531] [PubMed: 15206996](Analysis of General Practice Research Database from UK on 1.6 million persons from 1994-2000 found 128 cases of drug induced liver injury [2.4/100,000 person years]; 3 cases were attributed to cimetidine for an odds ratio of 2.0 compared to controls [n=5000] which was not statistically significant).
- Björnsson E, Jerlstad P, Bergqvist A, Olsson R. Fulminant drug-induced hepatic failure leading to death or liver transplantation in Sweden. Scand J Gastroenterol 2005; 40: 1095-101. [PubMed: 16165719](Survey of all cases of DILI with fatal outcome from Swedish Adverse Drug Reporting system from 1966-2002: 103 cases identified as highly probable, probable or possible, one case attributed to ranitidine and one to omeprazole, but none to the other antiulcer agents).
- Darabi K. Proton-pump-inhibitor-induced hepatitis. South Med J 2005; 98: 844-5. [PubMed: 16144190](39 year old developed fatigue and abdominal pain 2 weeks after starting pantoprazole [bilirubin 1.2 mg/dL, ALT 3061 U/L, Alk P 89 U/L], which gradually resolved after drug was stopped).
- Salgueiro E, Rubio T, Hidalgo A, Manso G. Safety profile of proton pump inhibitors according to the spontaneous reports of suspected adverse reactions. Int J Clin Pharmacol Ther 2006; 44: 548-56. [PubMed: 17176621](Analysis of PPI related reports to Spanish Pharmacovigilance Database during 2004 found 58 reports of liver injury from omeprazole [n=36], lansoprazole [7], pantoprazole [12], rabeprazole [2] and esomeprazole [1], correlating somewhat with relative number of prescriptions; 82% were taking other medications; most "evolved to recovery").
- Sabaté M, Ibáñez L, Pérez E, Vidal X, Buti M, Xiol X, Mas A et al. Risk of acute liver injury associated with the use of drugs: a multicentre population survey. Aliment Pharmacol Ther 2007; 25: 1401-9. [PubMed: 17539979](Population based survey of 126 cases of acute liver injury due to drugs between 1993-1999 in Spain; 8 were attributed to ranitidine alone [incidence 5.1/100,000 person-years] and 5 to omeprazole alone [2.1/100,000], no mention of pantoprazole).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J; Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008; 135: 1924-34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, 2 were attributed to ranitidine, none to cimetidine or the proton pump inhibitors).
- Sandig C, Flechtenmacher C, Stremmel W, Eisenbach C. Pantoprazole induces severe acute hepatitis. Z Gastroenterol 2011; 49: 207-10. [PubMed: 21298607](52 year old woman developed jaundice 1 month after starting pantoprazole [bilirubin 4.8 mg/dL, ALT 1276 U/L, Alk P 196 U/L], resolving within 2 months of stopping).
- Ferrajolo C, Capuano A, Verhamme KM, Schuemie M, Rossi F, Stricker BH, Sturkenboom MC. Drug-induced hepatic injury in children: a case/non-case study of suspected adverse drug reactions in VigiBase. Br J Clin Pharmacol 2010; 70: 721-8. [PMC free article: PMC2997312] [PubMed: 21039766](World wide pharmacovigilance database contained 9036 hepatic adverse drug reactions in children, no antiulcer medication was listed in the top 40 causes).
- Reuben A, Koch DG, Lee WM; Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology 2010; 52: 2065-76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, but none were linked to pantoprazole or other antiulcer medications).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 2013; 144: 1419-25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, but none were attributed to rabeprazole, despite it being among the 10 most prescribed medications in Iceland).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol 2014; 13: 231-9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, none of which were attributed to rabeprazole or other proton pump inhibitors).
- Aslan M, Celik Y, Karadas S, Olmez S, Cifci A. Liver hepatotoxicity associated with pantoprazole: a rare case report. Wien Klin Wochenschr 2014; 126 (11-12): 390-2. [PubMed: 24652021](35 year old man developed nausea and fatigue 2 months after starting pantoprazole [bilirubin 0.8 mg/dL, ALT 1541 U/L, Alk P 359 U/L], resolving within a few weeks of stopping).
- van der Schaft J, van Schaik RH, van den Broek MP, Bruijnzeel-Koomen CA, de Bruin-Weller MS. Increased liver enzyme levels during azathioprine treatment: beware of concomitant use of proton pump inhibitors. Br J Dermatol 2015; 173: 1338-9. PubMed Citation. [PubMed: 26139089](Three patients with atopic dermatitis treated with azathioprine [150 mg daily] developed ALT elevations 2-5 weeks after starting pantoprazole or omeprazole [ALT 14 to 25 U/L before rising to 42 to 254 U/L after], resolving within 1-6 months after stopping the proton pump inhibitor and despite continuation of azathioprine).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 3 [0.3%] were attributed to proton pump inhibitors, including 1 each from omeprazole, esomeprazole and lansoprazole, but none from pantoprazole or rabeprazole).
- Tsai CF, Chen MH, Wang YP, Chu CJ, Huang YH, Lin HC, Hou MC, Let al. Proton pump inhibitors increase risk for hepatic encephalopathy in patients With cirrhosis in a population study. Gastroenterology 2017; 152: 134-41. [PubMed: 27639806](Analysis of the Taiwan National Health Insurance database found a higher rate of PPI use among patients with cirrhosis who developed hepatic encephalopathy [38%: 445 of 1166] compared to a matched group with cirrhosis who did not [rate not provided]; the relative risk was raised for all agents except for rabeprazole).
- Weersink RA, Bouma M, Burger DM, Drenth JPH, Froukje Harkes-Idzinga S, Hunfeld NGM, Metselaar HJ, et al. Safe use of proton pump inhibitors in patients with cirrhosis. Br J Clin Pharmacol 2018; 84: 1806-20. [PMC free article: PMC6046475] [PubMed: 29688583](Systematic review of 69 publications in the literature suggested plasma levels of pantoprazole are more than 7-fold elevated in patients with cirrhosis and that patients with Child Pugh Class A or B should receive omeprazole and only esomeprazole be used in Child Pugh Class C cirrhosis).
- Meunier L, Ursic-Bedoya J, Pageaux GP, Larrey D. Pantoprazole-induced autoimmune chronic hepatitis. Liver Int 2018; 38: 995-9. PubMed Citation. [PubMed: 29532602](52 year old woman developed jaundice 8 weeks after starting pantoprazole [bilirubin 10.4 mg/dL, ALT 1520 U/L, Alk P 395 U/L, ANA 1:160], improving but not resolving completely after stopping pantoprazole, ultimately responding to budesonide therapy that was discontinued 2 years later without subsequent relapse but while still on ursodiol).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Lansoprazole.[LiverTox: Clinical and Researc...]Review Lansoprazole.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Rabeprazole.[LiverTox: Clinical and Researc...]Review Rabeprazole.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Omeprazole.[LiverTox: Clinical and Researc...]Review Omeprazole.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Pantoprazole: a proton pump inhibitor with oral and intravenous formulations.[Expert Rev Gastroenterol Hepat...]Review Pantoprazole: a proton pump inhibitor with oral and intravenous formulations.Devault KR. Expert Rev Gastroenterol Hepatol. 2007 Dec; 1(2):197-205.
- Pantoprazole: a new proton pump inhibitor in the management of upper gastrointestinal disease.[Drugs Today (Barc). 1999]Pantoprazole: a new proton pump inhibitor in the management of upper gastrointestinal disease.Bardhan KD. Drugs Today (Barc). 1999 Oct; 35(10):773-808.
- Pantoprazole - LiverToxPantoprazole - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...