NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Mifepristone, also known as RU-486, is a potent synthetic steroidal antiprogesterone which is used as a single dose in combination with misoprostol, a prostaglandin analogue, to induce medical abortion. Mifepristone with misoprostol have not been associated with serum enzyme elevations or with clinically apparent liver injury.
Mifepristone alone, without misoprostol, is also approved as therapy of Cushing syndrome where it is given in a higher dose and for extended periods. Long term higher doses of mifepristone have been linked to a low rate of serum enzyme elevations during therapy and rare instances of clinically apparent liver injury.
Background
Mifepristone (mif" e pris' tone) is a synthetic antiprogesterone which antagonizes the action of progesterone by competing with its binding to its receptor. The sudden loss of progesterone activity during pregnancy causes a series of intrauterine and cervical changes that result in termination of pregnancy. Misoprostol (mye" soe pros' tol) is a prostaglandin analogue that causes uterine contraction which completes the medical abortion. In multiple large prospective studies, the administration of a single dose of mifepristone followed within 24 to 48 hours by a prostaglandin agonist safely terminated early pregnancy in more than 90% of women. Mifepristone was first approved for use in France in 1988, in Great Britain in 1991, Sweden in 1992, and the United States in 2000. The current indications for this combination is for medical termination of intrauterine pregnancy through 70 days of gestation. Mifepristone is available in tablets of 200 mg under the brand name Mifeprex. The currently recommended dose of mifepristone for inducing a medical abortion is as a single 200 mg tablet followed 24 to 48 hours later by buccal administration of 800 mcg of misoprostol (a prostaglandin agonist). Mifepristone has been used off-label as a means of emergency contraception, but is not approved for that use. Side effects are common, but generally mild-to-moderate in severity and can include uterine bleeding, nausea, vomiting, abdominal cramps, weakness, fever, headache, diarrhea, and dizziness. Rare, but potentially severe adverse events include serious uterine bleeding and serious bacterial infections, failed abortion and need for hospitalization. Contraindications to use of mifepristone/misoprostol include pregnancy beyond 70 days (10 weeks), ectopic pregnancy, presence of an intrauterine device, adrenal failure, porphyria and use of anticoagulants. Because of the serious nature of these side effects, mifepristone/misoprostol is available only through a Risk Evaluation and Mitigation Strategy (REMS) program to certified prescribers.
Mifepristone (without misoprostol) is also approved for use in Cushing syndrome caused by excessive production of glucocorticoids. Mifepristone also has antiglucocorticoid receptor activity and has been found to alleviate hyperglycemia in adults with hypercortisolism and glucose intolerance or diabetes who have failed to respond or are not candidates for surgical therapy. Mifepristone was approved for this indication in 2012 and is available in 300 mg tablets under the brand name Korlym. The recommended dose is 300 mg once daily initially with subsequent increases based upon efficacy and tolerance to a maximum of 1200 mg daily. Adverse events are not uncommon but generally mild and manageable, including nausea, vomiting, anorexia, fatigue, headache, arthralgia, peripheral edema, hypertension, dizziness, and hypokalemia. Severe adverse reactions include termination of pregnancy, adrenal insufficiency, vaginal bleeding, endometrial changes and QTc interval prolongation. Mifepristone is metabolized by CYP 3A4 and 2C8/2C9 and has many drug-drug interactions.
Hepatotoxicity
In large prelicensure clinical trials, medical abortion with mifepristone/misoprostol was safe and not accompanied by abnormalities in laboratory tests or cases of hepatitis or jaundice. Since its licensure and more widescale use, there have been no published reports of liver injury attributed to mifepristone and misoprostol used to induce medical abortion.
In contrast, long term, higher dose therapy with mifepristone has been associated with an appreciable rate of serum enzyme elevations during treatment and with rare instances of clinically apparent liver injury. In one report, the onset of liver injury arose after 2 to 3 months of treatment and was characterized by marked jaundice and pruritus, with minimal serum aminotransferase and alkaline phosphatase elevations typical of bland cholestasis as occurs with estrogen or anabolic steroid use. Liver biopsy confirmed the finding of bland cholestasis. While jaundice was severe and prolonged, it ultimately resolved without evidence of residual injury.
Likelihood score: D (possible cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism by which mifepristone might cause liver injury is uncertain, but clinical features suggest that it is due to an estrogen- or androgen-like effect. The injury has been associated only with long term use of mifepristone. The single dose administration of mifepristone and misoprostol and their low doses are possible reasons why they are not hepatotoxic. Mifepristone is metabolized by the liver, largely by the cytochrome P450 isozyme CYP 3A4 and plasma levels vary if inducers or inhibitors of CYP 3A are used concurrently.
Outcome and Management
Severity of liver injury during mifepristone therapy ranges from asymptomatic elevations in serum aminotransferase levels to symptomatic liver injury with jaundice. Women on long term mifepristone therapy who develop symptoms of fatigue, itching or jaundice should be tested for routine liver tests and therapy discontinued if there is evidence of liver injury. Restarting mifepristone after acute liver injury attributed to its use should be avoided.
Drug Class: Obstetrical and Gynecological Agents, Pregnancy Termination Agents
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Mifepristone – Korlym®, Mifeprex®
DRUG CLASS
Pregnancy Termination Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULAS AND STRUCTURES
| DRUG | CAS REGISTRY NO | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Mifepristone | 84371-65-3 | C29-H35-N-O2 |
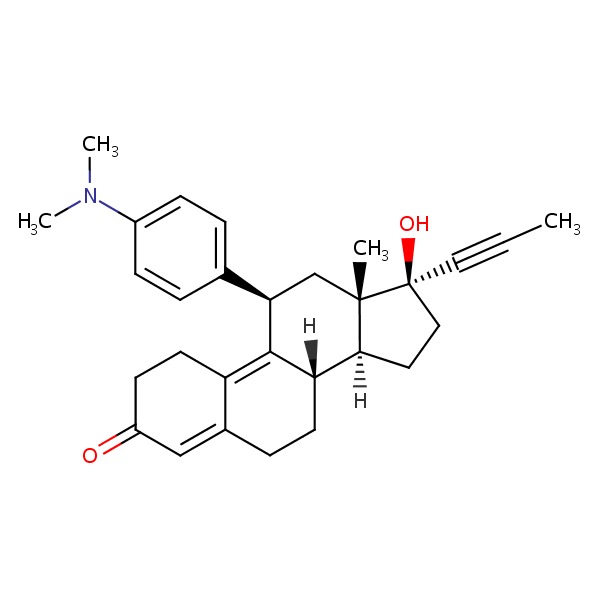 |
| Misoprostol | 59122-46-2 | C22-H38-O5 |
 |
ANNOTATED BIBLIOGRAPHY
References updated: 10 March 2018
- Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999.(Review of hepatotoxicity published in 1999 before the availability of mifepristone).
- Chitturi S, Farrell GC. Estrogen receptor antagonists. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 610-2.(Review of hepatotoxicity of hormonal agents; does not discuss mifepristone).
- Schimmer BP, Parker KL. Contraception and pharmacotherapy of obstetrical and gynecological disorders. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1833-52.(Textbook of pharmacology and therapeutics).
- https://www
.accessdata .fda.gov/scripts/cder/daf/ (FDA Drug Approvals website that has product labels [package inserts], letters of approval and full FDA scientific review of the new drug application for safety and efficacy; mentions that elevations in serum enzymes during therapy with long term mifepristone were generally mild, transient and associated with higher doses [1200 mg daily] or use of other potentially hepatotoxic medications). - Couzinet B, Le Strat N, Ulmann A, Baulieu EE, Schaison G. Termination of early pregnancy by the progesterone antagonist RU 486 (Mifepristone). N Engl J Med 1986; 315: 1565-70. [PubMed: 3785321](Among 100 women with an early, unwanted pregnancy who were treated with 1 of 3 regimens of mifepristone [400 to 800 mg total dose], 85 had a complete abortion within 8 days and “the only important side effect observed…was prolonged uterine bleeding”).
- Rodger MW, Baird DT. Induction of therapeutic abortion in early pregnancy with mifepristone in combination with prostaglandin pessary. Lancet 1987; 2 (8573): 1415-8. [PubMed: 2891991](Among 100 women requesting abortion early in pregnancy who were given oral mifepristone [400-600 mg] followed in 48 hours by a prostaglandin analog [gemeprost] by vaginal pessary, 95 had a complete abortion and adverse events included bleeding, diarrhea, pelvic pain [after prostaglandin], and incomplete abortion requiring surgical evacuation: “liver function tests” were similar before and after therapy).
- Silvestre L, Dubois C, Renault M, Rezvani Y, Baulieu EE, Ulmann A. Voluntary interruption of pregnancy with mifepristone (RU 486) and a prostaglandin analogue. A large-scale French experience. N Engl J Med 1990; 322: 645-8. [PubMed: 2304490](Among 2040 women given mifepristone followed in 36-48 hours by a prostaglandin analogue [gemeprost pessary or sulprostone intramuscularly], 96% had a complete medical abortion and adverse events included bleeding in almost all women for 1-33 days but not requiring transfusion, abdominal pain in 70-80% with 5-23% requiring analgesics, nausea and diarrhea; no mention of ALT elevations or hepatotoxicity).
- Mifepristone (RU 486). Med Lett Drugs Ther 1990; 32 (833): 112-3. [PubMed: 2247020](Concise review of the mechanism of action, efficacy, and safety of oral mifepristone for induction of medical abortion).
- Peyron R, Aubény E, Targosz V, Silvestre L, Renault M, Elkik F, Leclerc P, et al. Early termination of pregnancy with mifepristone (RU 486) and the orally active prostaglandin misoprostol. N Engl J Med 1993; 328: 1509-13. [PubMed: 8479487](Among 873 women in two open label trials of mifepristone and different doses of misoprostol 48 hours later, medical abortion was induced in 96-98% and adverse events included uterine bleeding and cramps, nausea and diarrhea; no mention of ALT elevations or hepatotoxicity).
- Cheng L, Che Y, Gülmezoglu AM. Interventions for emergency contraception. Cochrane Database Syst Rev 2012; (8): CD001324. [PubMed: 22895920](Systematic analysis of 100 randomized controlled trials of emergency contraception with 55,666 women using mifepristone, levonorgestrel, copper intrauterine device placement and ulipristal reported that all regimens were safe; no mention of ALT elevations or hepatotoxicity).
- Mifepristone for Cushing's syndrome. Med Lett Drugs Ther 2012; 54 (1392): 46-7. [PubMed: 22683927](Concise review of the mechanism of action, clinical efficacy, safety and costs of mifepristone for Cushing syndrome shortly after its approval for this indication in the US; does not mention ALT elevations or hepatotoxicity).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: the DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury collected in the United States between 2004 and 2012, no cases were attributed to mifepristone or other emergency contraception regimens).
- Mifepristone (Mifeprex) label changes. Med Lett Drugs Ther 2016; 58 (1493): 55-6. [PubMed: 27101211](Concise summary of changes in dosages of mifepristone [200 mg] and misoprostol [800 mcg] and expansion of indications [use within 70 days after first day of last menstrual period]).
- Kapur A, Angomchanu R, Dey M. Efficacy of use of long-term, low-dose mifepristone for the treatment of fibroids. J Obstet Gynaecol India 2016; 66 (Suppl 1): 494-8. [PMC free article: PMC5016456] [PubMed: 27651652](Among 36 women with uterine fibroids treated with low dose mifepristone [50 mg once weekly] for 24 weeks, fibroid volume, menorrhagia and pelvic pain improved but there was a transient rise in "mean transaminases [AST/ALT] at 6 months", which resolved within 3 months of stopping; details not provided).
- Ragucci E, Nguyen D, Lamerson M, Moraitis AG. Effects of mifepristone on nonalcoholic fatty liver disease in a patient with a cortisol-secreting adrenal adenoma. Case Rep Endocrinol 2017; 2017: 6161348. [PMC free article: PMC5733994] [PubMed: 29348947](A 49 year old woman with nonalcoholic steatohepatitis and Cushing syndrome treated with mifepristone [900 mg daily] for 24 weeks had a 16 pound weight loss and marked improvement in serum ALT levels [232 U/L to ~40 U/L], which remained normal after stopping).
- Funke K, Rockey DC. Cholestatic drug-induced liver injury caused by mifepristone. Hepatology 2018 Dec 18. [ePub ahead of print] [PubMed: 30561784](65 year old woman with Cushing syndrome developed jaundice 3 months after starting mifepristone [300 mg rising to 900 mg daily] with initial bilirubin rising from 17 to a peak of 33 mg/dL, ALT 49 to 169 U/L and Alk P 80 to 170 U/L, and liver biopsy showing bland cholestasis; jaundice persisting for 3 months but ultimately resolving; injury resembling anabolic steroid or estrogen associated cholestatic jaundice).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- The abortifacient effect of misoprostol in the second trimester. A randomized comparison with gemeprost in patients pre-treated with mifepristone (RU486).[Hum Reprod. 1993]The abortifacient effect of misoprostol in the second trimester. A randomized comparison with gemeprost in patients pre-treated with mifepristone (RU486).el-Refaey H, Hinshaw K, Templeton A. Hum Reprod. 1993 Oct; 8(10):1744-6.
- Review Medical methods for first trimester abortion.[Cochrane Database Syst Rev. 2022]Review Medical methods for first trimester abortion.Zhang J, Zhou K, Shan D, Luo X. Cochrane Database Syst Rev. 2022 May 24; 5(5):CD002855. Epub 2022 May 24.
- Unsuccessful treatment of missed abortion with a combination of an antiprogesterone and a prostaglandin E1 analogue.[Br J Obstet Gynaecol. 1997]Unsuccessful treatment of missed abortion with a combination of an antiprogesterone and a prostaglandin E1 analogue.Nielsen S, Hahlin M, Platz-Christensen JJ. Br J Obstet Gynaecol. 1997 Sep; 104(9):1094-6.
- Review Mifepristone dose in the regimen with misoprostol for medical abortion.[Contraception. 2006]Review Mifepristone dose in the regimen with misoprostol for medical abortion.Marions L. Contraception. 2006 Jul; 74(1):21-5. Epub 2006 May 19.
- The efficacy of medical abortion: a meta-analysis.[Contraception. 2000]The efficacy of medical abortion: a meta-analysis.Kahn JG, Becker BJ, MacIsaa L, Amory JK, Neuhaus J, Olkin I, Creinin MD. Contraception. 2000 Jan; 61(1):29-40.
- Mifepristone - LiverToxMifepristone - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...