NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Midostaurin is an orally available small molecule inhibitor of FMS-like tyrosine kinase 3 (FLT3) which is used as an antineoplastic agent in the treatment of acute myeloid leukemia with FLT3 mutations. Midostaurin is associated with a moderate rate of serum aminotransferase elevations during therapy and is suspected to cause rare instances of clinically apparent acute liver injury.
Background
Midostaurin (mye" doe staw' rin) is a potent small molecule multi-kinase inhibitor with specific activity against FLT3 (FMS-like tyrosine kinase 3), a tyrosine kinase receptor that is mutated in to up one-third of patients with acute myeloid leukemia (AML). The mutated FLT3 activates an intracellular signaling cascade of RAS-MEK-PI3K-AKT-STAT-5, promoting unregulated cell growth and proliferation. Midostaurin also has activity against other kinases including Kit, platelet derived growth factor receptor, vascular endothelial growth factor receptor 2 and members of the protein kinase C family. Midostaurin has been found to induce objective responses in a proportion of patients with refractory AML with detectable FLT3 mutations and in patients with advanced systemic mastocytosis. Midostaurin received accelerated approval for these indication in the United States in 2017 and is available in tablets of 25 mg under the brand name Rydapt. For newly diagnosed AML with FLT3 mutations, the recommended dose is 50 mg orally twice daily in combination with standard cytarabine and daunorubicin induction and cytarabine consolidation. For advanced systemic mastocytosis, the recommended dose is 100 mg orally twice daily, continued until progressive disease or intolerable toxicity occurs. Side effects are common and can include fatigue, myalgia, arthralgia, fever, cytopenias, diarrhea, nausea, abdominal pain, dizziness, headache, hypotension, cough and stomatitis. Potentially severe side effects include febrile neutropenia and sepsis, interstitial lung disease and embryo-fetal toxicity.
Hepatotoxicity
Elevations in serum aminotransferase levels are common during midostaurin therapy occurring in up to 71% of patients with AML also receiving standard induction therapy and rising above 5 times the upper limit of the normal range in 20%. In patients with systemic mastocytosis receiving midostaurin monotherapy, ALT elevations arose in 31% of patients and rose to above 5 times ULN in 4%. Hyperbilirubinemia was also common in these studies but instances of clinically apparent liver injury with jaundice, severe hepatoxicity and deaths from hepatic failure were not reported. However, because of the limited clinical experience with the use of midostaurin and other FLT3 inhibitors, their potential for causing liver injury is not well defined.
Likelihood score: E* (unproven but suspected cause of clinically apparent liver injury).
Mechanism of Injury
The possible cause of the liver injury due to midostaurin is not known. Midostaurin is metabolized in the liver largely by the cytochrome P450 system (largely CYP 3A4) and is susceptible to drug-drug interactions with inhibitors or inducers of the microsomal enzyme system, and strong modulators of CYP 3A4 should be avoided in patients receiving midostaurin.
Outcome and Management
Midostaurin therapy has been associated with transient serum aminotransferase elevations during therapy but has not been linked to instances of acute liver injury with jaundice or symptoms. Serum aminotransferase elevations above 5 times the upper limit of normal (if confirmed) should lead to temporary discontinuation, which should be permanent if laboratory values do not improve significantly or resolve within a few weeks or if symptoms or jaundice arise.
Drug Class: Antineoplastic Agents, Protein Kinase Inhibitors
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Midostaurin – Rydapt®
DRUG CLASS
Antineoplastic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Midostaurin | 120685-11-2 | C35-H30-N4-O |
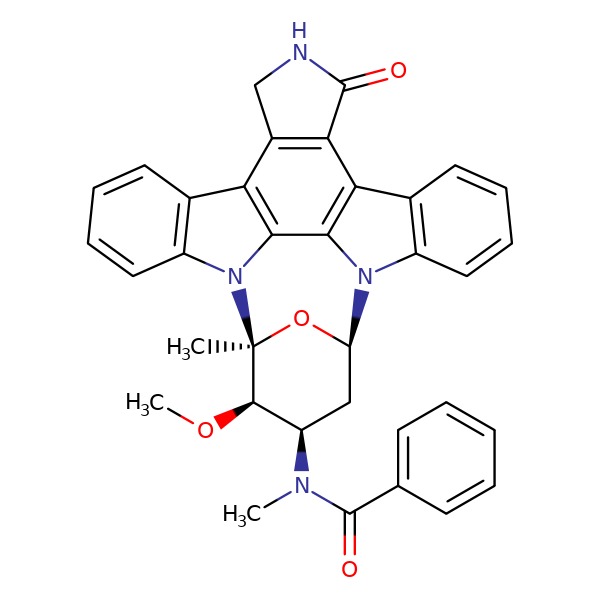 |
ANNOTATED BIBLIOGRAPHY
References updated: 10 April 2019
Abbreviations: FLT3, FMS-like tyrosine kinase-3; AML, acute myelogenous leukemia.
- Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999.(Review of hepatotoxicity published in 1999 before the availability of kinase inhibitors).
- DeLeve LD. Erlotinib. Cancer chemotherapy. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 556.(Review of hepatotoxicity of cancer chemotherapeutic agents published in 2013 before the availability of midostaurin).
- Wellstein A, Giaccone G, Atkins MB, Sausville EA. Pathway-targeted therapies: monoclonal antibodies, protein kinase inhibitors, and various small molecules. In, Brunton LL, Hilal-Danan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1203-36.(Textbook of pharmacology and therapeutics).
- https://www
.accessdata .fda.gov/scripts/cder/daf/ (FDA Drug Approvals website that has product labels [package inserts], letters of approval and full FDA scientific review of the new drug application for safety and efficacy; mentions that ALT elevations arose in similar proportions of patients receiving midostaurin as placebo during induction therapy of AML [69% vs 68%] but elevations above 5 times ULN were more frequent with midostaurin [20% vs 16%] although ALT elevations with hyperbilirubinemia were less frequent [3% vs 5%]). - Gotlib J, Kluin-Nelemans HC, George TI, Akin C, Sotlar K, Hermine O, Awan FT, et al. Efficacy and safety of midostaurin in advanced systemic mastocytosis. N Engl J Med 2016; 374: 2530-41. [PubMed: 27355533](Among 116 patients with advanced systemic mastocytosis treated with midostaurin in an open-label study, the objective response rate was 56% and adverse events were frequent including nausea [79%], diarrhea [54%] and cytopenias; no mention of ALT elevations or hepatotoxicity and no discontinuations for liver injury).
- Midostaurin (Rydapt) for AML and advanced systemic mastocytosis. Med Lett Drugs Ther 2017; 59 (1527): e140. [PubMed: 28787746](Concise review of the trials showing efficacy and safety of midostaurin in systemic mastocytosis shortly after its approval for this indication in the US mentions adverse events of febrile neutropenia, nausea, vomiting and mucositis, but not ALT elevations or hepatotoxicity).
- Perl AE, Altman JK, Cortes J, Smith C, Litzow M, Baer MR, Claxton D, et al. Selective inhibition of FLT3 by gilteritinib in relapsed or refractory acute myeloid leukaemia: a multicentre, first-in-human, open-label, phase 1-2 study. Lancet Oncol 2017; 18: 1061-75. [PMC free article: PMC5572576] [PubMed: 28645776](Among 252 adults with refractory or relapsed AML treated with different doses of gilteritinib, responses occurred in 40% and complete remission in 8%; adverse events were frequent including febrile neutropenia, sepsis, and pneumonia, while ALT elevations arose in 18% of recipients which were above 5 times ULN in 5%, but there were no instances of clinically apparent liver injury).
- Fathi AT, Chen YB. The role of FLT3 inhibitors in the treatment of FLT3-mutated acute myeloid leukemia. Eur J Haematol 2017; 98: 330-6. [PubMed: 28000291](Review of the role of mutated FLT3 in AML and efficacy of drugs with potent, specific activity against FLT3 in AML, including sorafenib, quizartinib, crenolanib and gilteritinib, as well as the nonspecific tyrosine kinase inhibitors with some activity against FLT3 such as midostaurin, sunitinib and sorafenib).
- Stone RM, Mandrekar SJ, Sanford BL, Laumann K, Geyer S, Bloomfield CD, Thiede C, et al. Midostaurin plus chemotherapy for acute myeloid leukemia with a FLT3 mutation. N Engl J Med 2017; 377: 454-64. [PMC free article: PMC5754190] [PubMed: 28644114](Among 717 patients with AML and FLT3 mutations treated with standard chemotherapy with or without midostaurin, median overall survival was longer in midostaurin treated patients [75 vs 32 months], while adverse event rates were similar in the two groups including febrile neutropenia [82% vs 82%], ALT elevations [13% vs 9%] and hyperbilirubinemia [7% vs 8%]).
- Kasamon YL, Ko CW, Subramaniam S, Ma L, Yang Y, Nie L, Shord S, et al. FDA approval summary: midostaurin for the treatment of advanced systemic mastocytosis. Oncologist 2018; 23: 1511-9. [PMC free article: PMC6292539] [PubMed: 30115735](Review of the open-label clinical trial that was the basis for approval of midostaurin for advanced systemic mastocytosis during which 56% of patients had dose interruptions and 21% discontinuation for adverse events; no mention of ALT elevations or hepatotoxicity).
- Click ZR, Seddon AN, Bae YR, Fisher JD, Ogunniyi A. New Food and Drug Administration-approved and emerging novel treatment 0ptions for acute myeloid leukemia. Pharmacotherapy 2018; 38: 1143-54. [PubMed: 30220082](Review of recently developed targeted antineoplastic agents active in treating AML including midostaurin, the first FLT3-targeted therapy for AML; no mention of ALT elevations or hepatotoxicity).
- Kim M, Williams S. Midostaurin in combination with standard chemotherapy for treatment of newly diagnosed FMS-like tyrosine kinase 3 (FLT3) mutation-positive acute myeloid leukemia. Ann Pharmacother 2018; 52: 364-9. [PubMed: 29231051](Review of the efficacy and safety of midostaurin combined with standard induction chemotherapy for AML; mentions frequency of adverse events and severe adverse events of febrile neutropenia, pulmonary fibrosis, drug-drug interactions and embryo-fetal toxicity, but not hepatotoxicity or ALT elevations).
- DeAngelo DJ, George TI, Linder A, Langford C, Perkins C, Ma J, Westervelt P, et al. Efficacy and safety of midostaurin in patients with advanced systemic mastocytosis: 10-year median follow-up of a phase II trial. Leukemia 2018; 32: 470-8. [PubMed: 28744009](Among 26 patients with advanced systemic mastocytosis treated with midostaurin for up to 10 years, no new or unexpected toxicity arose; no mention of ALT elevations or hepatotoxicity).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Gilteritinib.[LiverTox: Clinical and Researc...]Review Gilteritinib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Midostaurin in Combination With Standard Chemotherapy for Treatment of Newly Diagnosed FMS-Like Tyrosine Kinase 3 (FLT3) Mutation-Positive Acute Myeloid Leukemia.[Ann Pharmacother. 2018]Review Midostaurin in Combination With Standard Chemotherapy for Treatment of Newly Diagnosed FMS-Like Tyrosine Kinase 3 (FLT3) Mutation-Positive Acute Myeloid Leukemia.Kim M, Williams S. Ann Pharmacother. 2018 Apr; 52(4):364-369. Epub 2017 Dec 12.
- Phase IIB trial of oral Midostaurin (PKC412), the FMS-like tyrosine kinase 3 receptor (FLT3) and multi-targeted kinase inhibitor, in patients with acute myeloid leukemia and high-risk myelodysplastic syndrome with either wild-type or mutated FLT3.[J Clin Oncol. 2010]Phase IIB trial of oral Midostaurin (PKC412), the FMS-like tyrosine kinase 3 receptor (FLT3) and multi-targeted kinase inhibitor, in patients with acute myeloid leukemia and high-risk myelodysplastic syndrome with either wild-type or mutated FLT3.Fischer T, Stone RM, Deangelo DJ, Galinsky I, Estey E, Lanza C, Fox E, Ehninger G, Feldman EJ, Schiller GJ, et al. J Clin Oncol. 2010 Oct 1; 28(28):4339-45. Epub 2010 Aug 23.
- Review Midostaurin/PKC412 for the treatment of newly diagnosed FLT3 mutation-positive acute myeloid leukemia.[Expert Rev Hematol. 2017]Review Midostaurin/PKC412 for the treatment of newly diagnosed FLT3 mutation-positive acute myeloid leukemia.Luskin MR, DeAngelo DJ. Expert Rev Hematol. 2017 Dec; 10(12):1033-1045. Epub 2017 Oct 30.
- Review Midostaurin: A New Oral Agent Targeting FMS-Like Tyrosine Kinase 3-Mutant Acute Myeloid Leukemia.[Pharmacotherapy. 2017]Review Midostaurin: A New Oral Agent Targeting FMS-Like Tyrosine Kinase 3-Mutant Acute Myeloid Leukemia.Stansfield LC, Pollyea DA. Pharmacotherapy. 2017 Dec; 37(12):1586-1599. Epub 2017 Nov 23.
- Midostaurin - LiverToxMidostaurin - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...