NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Mechlorethamine is a nitrogen mustard and antineoplastic agent that has been in clinical use for more than 60 years, given systemically in combination with other antineoplastic agents to treat Hodgkin disease, chronic leukemias, lung cancer and polycythemia vera. Currently, however, it is used largely as a topical gel for therapy of cutaneous T-cell lymphomas and mycosis fungoides. Given parenterally in combination with other antineoplastic agents it was associated with low rates of serum enzyme elevations during therapy, but mechlorethamine has not been implicated specifically in cases of acute, clinically apparent injury.
Background
Mechlorethamine (mek" lor eth' a meen), also known as chlormethine and mustine, is a nitrogen mustard and was the first alkylating agent developed for use as an antineoplastic agent in man. It remains the most reactive in this class of agents. Because it is irritating to local tissues and causes gastrointestinal intolerance, mechlorethamine is administered intravenously. Modifications of the chemical structure of mechlorethamine has led to similarly effective, but safer and better tolerated forms of alkylating agents, such as cyclophosphamide, ifosfamide, chlorambucil and melphalan. The alkylating agents act by causing modification and cross linking of DNA, thus triggering programmed cell death (apoptosis) and inhibiting DNA, RNA and protein synthesis in rapidly dividing cells. Mechlorethamine was approved for use in the United States in 1949. The major use of mechlorethamine was in a regimen with vincristine, procarbazine and prednisone, commonly referred to as MOPP, used to treat Hodgkin disease and lymphoma. In recent years, mechlorethamine has been replaced by more stable alkylating agents such as cyclophosphamide (COPP). Current listed indications include Hodgkin's disease, lymphosarcoma, chronic leukemias, polycythemia vera, mycosis fungoides and lung cancer. Mechlorethamine was previously available in 10 mg vials generically and under the brand name Mustargen. The recommended dose varied with the indication, patient age and weight. Mechlorethamine is currently available as a topic gel for treatment of cutaneous T-cell lymphomas and mycosis fungoides, but requires special handling. Mechlorethamine shares common side effects with other alkylating agents, which include nausea, vomiting diarrhea, alopecia, pruritus, bone marrow suppression and rash.
Hepatotoxicity
Mild and transient elevations in serum aminotransferase levels were not uncommon during cycles of cancer chemotherapy regimens that included mechlorethamine, but its role in causing these abnormalities was never entirely clear. The enzyme elevations were usually mild, transient and without symptoms, so that dose modifications of mechlorethamine were rarely needed. Mechlorethamine has not been associated specifically with clinically apparent liver injury. Sinusoidal obstruction syndrome has been reported after MOPP therapy, but largely in patients with other risk factors for this complication, such as total body irradiation or previous courses of antineoplastic therapy. Topical mechlorethamine has not been associated with liver injury, although the possibility of systemic absorption continues to make hepatic adverse events mentioned as a concern. Careful analysis for bone marrow toxicity and plasma concentrations of the drug, however, have failed to demonstrate any evidence for significant absorption with proper use of the cutaneous gel.
Likelihood score: E (unlikely cause of clinically apparent liver injury).
Mechanism of Injury
The potential mechanism of hepatotoxicity from mechlorethamine is probably similar to that of other alkylating agents, a direct cytotoxic injury which is most specific to rapidly dividing cells, but in high doses can injury other cell types such as sinusoidal lining cells or hepatocytes.
Outcome and Management
Liver injury including sinusoidal obstruction syndrome are very rare after mechlorethamine therapy. The severity of sinusoidal obstruction syndrome varies considerably, from transient mild symptomatic liver injury to acute liver failure that is rapidly fatal. There is no known specific therapy for sinusoidal obstruction syndrome and management should focus on avoidance of further injury and supportive care. Rechallenge should not be done.
Drug Class: Antineoplastic Agents, Alkylating Agents
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Mechlorethamine – Mustargen®
DRUG CLASS
Antineoplastic Agents, Alkylating Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
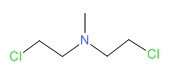
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Mechlorethamine | 51-75-2 | C5-H11-Cl2-N |
 |
ANNOTATED BIBLIOGRAPHY
References updated: 06 June 2019
- Zimmerman HJ. Oncotherapeutic and immunosuppressive agents. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 673-708.(Expert review of hepatotoxicity of cancer chemotherapeutic agents published in 1999; mentions that mechlorethamine has not been linked to significant liver injury).
- DeLeve LD. Alkylating agents. Cancer chemotherapy. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, p. 551-4.(Review of hepatotoxicity of cancer chemotherapeutic agents discusses alkylating agents but not mechlorethamine specifically; many alkylating agents, particularly if given in high doses with busulfan or irradiation, can cause sinusoidal obstruction syndrome [SOS]).
- Wellstein A, Giaccone G, Atkins MB, Sausville EA. Cytotoxic agents. Chemotherapy of neoplastic diseases. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1167-1202.(Textbook of pharmacology and therapeutics).
- Dameshek W, Weisfuse L, Stein T. Nitrogen mustard therapy in Hodgkin's disease. Blood 1949; 4: 338-79. [PubMed: 18116112](Response rates and toxicity of nitrogen mustard in 50 patients with Hodgkin's disease; one patient with preexisting jaundice worsened with therapy, with deepening jaundice, coma and death 9 days later; autopsy showed partial compression of the common bile duct, but also areas of necrosis in the liver).
- Zimmerman HJ, Alpert LK, Howe J. The effect of nitrogen mustard (bis-β-chlorethylamine) on liver function and structure in patients with neoplastic disease. J Lab Clin Med 1952; 40: 387. Not in PubMed.(Reported to show no significant worsening of liver function tests in patients with cancer during therapy with mechlorethamine).
- De Vita VT, Carbone PP, Owens AH Jr, Gold GL, Krant MJ, Edmonson J. Clinical trials with 1,3-bis(2-chloroethyl)-1-nitrosourea, NSC-409962. Cancer Res 1965; 25: 1876-81. [PubMed: 5858571](Preliminary studies of BCNU in 144 patients with malignancies including different dose schedules; AST elevations occurred in 15% after 13-63 days and were self limited in all; liver toxicity may have contributed to the death of one patient).
- Hansen HH, Selawry OS, Muggia FM, Walker MD. Clinical studies with 1-(2-chloroethyl)-3-cyclohexyl-1-nitrosourea (NSC 79037). Cancer Res 1971; 31: 223-7. [PubMed: 4926242](Preliminary studies of CCNU in 40 patients with malignancies; there was no consistent hepatic dysfunction; AST elevations occurred in one patient).
- Roth A, Cerlek S, Dominis M, Kolari. K. Liver changes induced by cytostatic drugs in patients with non Hodgkin's lymphomas. Acta Hepatogastroenterol (Stuttg) 1978; 25: 353-9. [PubMed: 726801](Minor elevations in serum enzymes and histological changes of inflammation, fat and hemosiderosis were common among 21 patients with lymphoma treated with MOPP and followed prospectively, but without a consistent pattern and the agent responsible for the changes could not be identified).
- Rollins BJ. Hepatic veno-occlusive disease. Am J Med 1986; 8: 297-306. [PubMed: 3526887](Review of the diagnosis, clinical course, histology and pathogenesis of veno-occlusive disease, now referred to as sinusoidal obstruction syndrome [SOS]).
- Jones RJ, Lee KS, Beschorner WE, Vogel VG, Grochow LB, Braine HG, Vogelsang GB, et al. Veno-occlusive disease of the liver following bone marrow transplantation. Transplantation 1987; 4: 778-83. [PubMed: 3321587](Among 235 patients undergoing bone marrow transplantation between 1982 and 1985, SOS developed in 52 [22%] of whom half died, making SOS the third most common cause of death in this population).
- Bearman SI. The syndrome of hepatic veno-occlusive disease after marrow transplantation. Blood 1995; 85: 3005-20. [PubMed: 7756636](Review of hepatic SOS after bone marrow transplantation; usually presents with painful hepatomegaly, weight gain [fluid and ascites] and jaundice within 3 weeks of myeloablation, with occlusion of central veins and sinusoids and extensive zone 3 [centrolobular] injury).
- DeLeve LD, Shulman HM, McDonald GB. Toxic injury to hepatic sinusoids: sinusoidal obstruction syndrome. Semin Liver Dis 2002; 22: 27-41. [PubMed: 11928077](Review of clinical features, pathology, etiology, prevention and treatment of sinusoidal obstruction syndrome, a better term for this condition than veno-occlusive disease; first described in association with exposure to phytotoxins [pyrrolizidine alkaloids], the most common cause now is cancer chemotherapy and particularly myeloablative conditioning regimens in preparation for bone marrow transplantation).
- McDonald GB. Hepatobiliary complications of hematopoietic cell transplantation, 40 years on. Hepatology 2010; 51: 1450-60. [PMC free article: PMC2914093] [PubMed: 20373370](Review of liver complications of bone marrow [hematopoietic cell] transplantation, which have become less frequent with better understanding of their causes and means of prevention; the rate of SOS has decreased because of avoidance of more aggressive ablative therapies [total body irradiation and high doses of cyclophosphamide] and better understanding of pharmacokinetics of the alkylating agents).
- Douros A, Bronder E, Andersohn F, Klimpel A, Thomae M, Sarganas G, Kreutz R, et al. Drug-induced liver injury: results from the hospital-based Berlin Case-Control Surveillance Study. Br J Clin Pharmacol 2015; 79: 988-99. [PMC free article: PMC4456131] [PubMed: 25444550](Among 198 patients with hepatitis of uniknown cause enrolled in a prospective database from 51 Berlin hospitals between 2002 and 2011, none were attributed to mechlorethamine).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 49 cases were attributed to antineoplastic agents, but none to mechlorethamine).
- Liner K, Brown C, McGirt LY. Clinical potential of mechlorethamine gel for the topical treatment of mycosis fungoides-type cutaneous T-cell lymphoma: a review on current efficacy and safety data. Drug Des Devel Ther 2018; 12: 241-254. 29440874. [PMC free article: PMC5798535] [PubMed: 29440874](Review of clinical efficacy and safety of mechlorethamine gel mentions that the adverse events are largely dermatologic and local and there is no evidence for its systemic absorption with cutaneous application; no mention of ALT elevations or hepatotoxicity).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Management of Mycosis Fungoides with Topical Chlormethine/Mechlorethamine Gel: A Columbia University Cutaneous Lymphoma Center Experience.[Acta Derm Venereol. 2021]Management of Mycosis Fungoides with Topical Chlormethine/Mechlorethamine Gel: A Columbia University Cutaneous Lymphoma Center Experience.Garcia-Saleem TJ, Stonesifer CJ, Khaleel AE, Geskin LJ. Acta Derm Venereol. 2021 Sep 8; 101(9):adv00544. Epub 2021 Sep 8.
- Mechlorethamine gel for the topical treatment of stage IA and IB mycosis fungoides-type cutaneous T-cell lymphoma.[Expert Rev Clin Pharmacol. 2014]Mechlorethamine gel for the topical treatment of stage IA and IB mycosis fungoides-type cutaneous T-cell lymphoma.Talpur R, Venkatarajan S, Duvic M. Expert Rev Clin Pharmacol. 2014 Sep; 7(5):591-7. Epub 2014 Jul 28.
- Topical chemotherapy in cutaneous T-cell lymphoma: positive results of a randomized, controlled, multicenter trial testing the efficacy and safety of a novel mechlorethamine, 0.02%, gel in mycosis fungoides.[JAMA Dermatol. 2013]Topical chemotherapy in cutaneous T-cell lymphoma: positive results of a randomized, controlled, multicenter trial testing the efficacy and safety of a novel mechlorethamine, 0.02%, gel in mycosis fungoides.Lessin SR, Duvic M, Guitart J, Pandya AG, Strober BE, Olsen EA, Hull CM, Knobler EH, Rook AH, Kim EJ, et al. JAMA Dermatol. 2013 Jan; 149(1):25-32.
- Review Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): part II. Prognosis, management, and future directions.[J Am Acad Dermatol. 2014]Review Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): part II. Prognosis, management, and future directions.Jawed SI, Myskowski PL, Horwitz S, Moskowitz A, Querfeld C. J Am Acad Dermatol. 2014 Feb; 70(2):223.e1-17; quiz 240-2.
- Review Topical treatment of early cutaneous T-cell lymphoma.[Hematol Oncol Clin North Am. 1...]Review Topical treatment of early cutaneous T-cell lymphoma.Ramsay DL, Meller JA, Zackheim HS. Hematol Oncol Clin North Am. 1995 Oct; 9(5):1031-56.
- Mechlorethamine - LiverToxMechlorethamine - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...