NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Mebendazole is an anthelmintic agent used commonly for roundworm (pinworm and hookworm) infections, trichinosis, capillariasis and toxocariasis and other parasitic worm infections. Mebendazole when given for prolonged periods in high doses has been associated with elevations in serum enzyme levels, and rare instances of acute, clinically apparent liver injury have been linked to its use.
Background
Mebendazole (me ben' da zole) is a benzimidazole anthelmintic similar in structure and mechanism of action to thiabendazole and albendazole. The benzimidazoles act by selective binding to beta-tubulin of parasitic worms, causing their immobilization and death. Mebendazole and albendazole share similar anthelmintic activity, mebendazole generally being preferred for treatment of pinworm and roundworm infections, and albendazole (because it is better absorbed) for systemic parasitic infections such as echinococcosis and cysticercosis. Mebendazole was approved for use in the United States in 1974 and is indicated for therapy of common parasitic worm infections. Mebendazole is available generically and under the brand names Emverm and Vermox in 100 mg and 500 mg chewable tablets. The usual dose is 100 or 500 mg once (pinworm) or varying doses for 3 days (whipworm, hookworm and roundworm infections), or varying doses for longer periods, depending upon the indication. Side effects with single dose regimens are uncommon, but can include gastrointestinal upset, fever, headache, nausea, vomiting and diarrhea. With more extended therapy, gastrointestinal symptoms are the most frequent side effects and rare but potentially severe adverse effects include neutropenia, hypersensitivity reactions, hepatitis, angioedema, Stevens Johnson syndrome and toxic epidermal necrolysis.
Hepatotoxicity
Mebendazole when given in typical doses has not been associated with serum enzyme elevations, although the duration of therapy is usually short and monitoring for enzyme elevations has rarely been reported. With high dose therapy (which is now rarely used with the availability of albendazole), elevations in serum aminotransferase levels (2 to 10 times normal) can occur, but are usually well tolerated. There have been rare reports of acute liver injury due to mebenazole, particularly when it is given repeatedly or in higher doses. The onset is usually with fever and malaise within days of starting or restarting therapy. The pattern of serum enzyme elevations is typically hepatocellular, and jaundice is uncommon. The abnormalities usually resolve rapidly with stopping therapy. Signs of hypersensitivity (rash, fever and eosinophilia) are typical and liver biopsy may show granulomas.
Likelihood score: D (possible cause of clinically apparent liver injury with extended therapy).
Mechanism of Injury
Mebendazole acts by binding tubulin in parasitic worms, which it does with greater avidity than the tubulin in mammalian cells, but some of the toxicity of the benzimidazoles may be related to this tubulin-binding activity. In most instances of clinically apparent liver injury, hypersensitivity appears to be the cause.
Outcome and Management
Mebendazole is usually well tolerated and the liver injury reported with its use has been mild and self-limited in course. Patients with hypersensitivity and acute liver injury attributed to mebendazole should avoid repeat exposure. It is unknown whether there is cross sensitivity with other benzimidazoles (such as albendazole), but there probably is and switching to another class of anthelmintic agents is appropriate if therapy is still needed.
Drug Class: Anthelmintic Agents
CASE REPORT
Case 1. Acute liver injury due to mebendazole.(1)
A 52 year old Belgian man was treated with mebendazole (100 mg twice daily) for 3 days for suspected ascariasis. Fourteen days later the course was repeated, but within 2 days of restarting mebendazole he developed fever (39 oC), diarrhea, poor appetite and fatigue. Because of the fever, he was given a 5 day course of cefuroxime, but remained febrile and symptomatic and was then found to have elevations in serum aminotransferase levels, with normal serum bilirubin and alkaline phosphatase (Table). He had eosinophilia (18%: absolute count 2,286/μL). Tests for hepatitis A, B and C were negative. He had low levels of antinuclear antibody (ANA: 1:40) and smooth muscle antibody (SMA: 1:160), but total globulin levels were normal. Ultrasound of the abdomen was negative. Stools were negative for ova and parasites. A liver biopsy showed multiple granulomas with multinucleate cells and active inflammation. There were no ova or helminths visualized and special stains for mycobacteria were negative. He improved rapidly without further therapy and 3 months later serum enzymes were normal.
Key Points
| Medication: | Mebendazole (100 mg twice daily) for ~5 days |
|---|---|
| Pattern: | Hepatocellular (R=9.7) |
| Severity: | 1+ (enzyme elevations without jaundice) |
| Latency: | 26 days after initial course, 2 days of second course |
| Recovery: | Within 3 months |
| Other medications: | Cefuroxime (after onset of symptoms) |
Laboratory Values
| Days After Starting | Days After Stopping | ALT (U/L) | Alk P (U/L) | Bilirubin* (mg/dL) | Other |
|---|---|---|---|---|---|
| 0 | Mebendazole (100 mg twice daily for 3 days) | ||||
| 14 | Mebendazole (100 mg twice daily for 2 days) | ||||
| 16 | 0 | Fever and rash | |||
| 26 | 10 | 466 | 170 | 1.0 | Eosinophilia |
| 28 | 12 | 540 | Liver biopsy | ||
| 100 | 90 | Normal | Normal | Normal | No symptoms |
| Normal Values | <48 | <60 | <1.2 | ||
Comment
Acute hepatocellular injury arose concurrent with symptoms and signs of hypersensitivity (rash and fever) within days of starting a second course of mebendazole. This pattern is typical of immunoallergic hepatitis and usually resolves rapidly, but can be severe if there is reexposure. The ANA and SMA titers may have been stimulated by the acute injury; in the absence of hyperglobulinemia were not compatible with autoimmune hepatitis. The granulomas found on liver biopsy reflect the generalized hypersensitivity and similar granulomas are likely to be found in other organs (lymph nodes, spleen).
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Mebendazole – Generic, Vermox®
DRUG CLASS
Anthelmintic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Mebendazole | 31431-39-7 | C16-H13-N3-O3 |
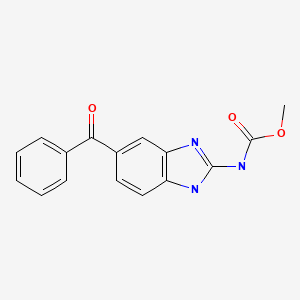
|
CITED REFERENCE
- 1.
- Colle I, Naegels S, Hoorens A, Hautekeete M. Granulomatous hepatitis due to mebendazole. J Clin Gastroenterol. 1999;28:44–5. [PubMed: 9916665]
ANNOTATED BIBLIOGRAPHY
References updated: 18 September 2021
- Zimmerman HJ. Anthelminthics. Hepatic injury from antimicrobial agents. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 626-8.(Expert review of hepatotoxicity of anthelmintics written in 1999; mebendazole produces hepatic injury in dogs and occasionally in humans by uncertain mechanisms).
- Keiser J, McCarthy J, Hotez PJ. Chemotherapy of helminth infections. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1001-7.(Textbook of pharmacology and therapeutics).
- Polzin DJ, Stowe CM, O'Leary TP, Stevens JB, Hardy RM. Acute hepatic necrosis associated with the administration of mebendazole to dogs. J Am Vet Med Assoc. 1981;179:1013–6. [PubMed: 7341557](Four of 10 Dachshunds treated with mebendazole [22 mg/kg for 3-5 days] developed acute hepatitis 8-10 days after stopping therapy [bilirubin 14.2 mg/dL, ALT 17 times ULN, Alk P 8 times ULN], and two died of multiorgan failure, autopsy showing centrolobular coagulative necrosis).
- Swanson JF, Breider MA. Hepatic failure following mebendazole administration to a dog. J Am Vet Med Assoc. 1982;181:72–3. [PubMed: 7107495](4 year old Labrador Retriever developed liver injury [bilirubin 8.1 mg/dL, ALT 8 times ULN, Alk P 5 times ULN] starting 3 days after a second course of mebendazole [22 mg/kg], autopsy showing centrolobular hepatic necrosis).
- Seitz R, Schwerk W, Arnold R. Z Gastroenterol. 1983;21:324–9. [Hepatocellular drug reaction caused by mebendazole therapy in cystic echinococcosis] German. [PubMed: 6613213](76 year old man with Echinococcal cysts of liver developed rash 49 days after starting mebendazole [~29 mg/kg/day], with ALT 250 U/L but normal bilirubin and Alk P; positive rechallenge to low dose [ALT 403 U/L]).
- Junge U, Mohr W. Z Gastroenterol. 1983;21:736–8. [Mebendazole-hepatitis] German. [PubMed: 6666188](Among 29 patients with echinococcosis treated with mebendazole, 1 developed hepatitis; 53 year old woman noted dark urine 2 months after starting therapy [bilirubin 2.1 mg/dL, ALT 475 U/L, Alk P 270 U/L]; biopsy showing spotty necrosis, resolving in 1.5 months; positive rechallenge [ALT 400 U/L, Alk P 358 U/L]).
- Mousa AM, Rudwan MA, Marafi AA, Muhtaseb SA, Dajani AI. Human cystic hydatid disease: treatment with interrupted courses of mebendazole. J Trop Med Hyg. 1986;89:257–64. [PubMed: 3795326](10 patients with echinococcal cysts were treated with high doses of mebendazole [1800 mg/day] for up to 18 weeks; a 37 year old woman with multiple cysts developed jaundice at 11 days that became cholestatic but ultimately resolved; few details given and referred to as “amoebic hepatitis”).
- Bekhti A, Pirotte J. Hepatotoxicity of mebendazole. Relationship with serum concentrations of the drug. Gastroenterol Clin Biol. 1987;11:701–3. [PubMed: 3692093](47 year old woman with hydatid cysts in the liver developed persistent elevations in ALT [60-400 U/L] and Alk P [207 U/L] without jaundice during a third course of mebendazole given in high doses [4.5-6.0 g daily], ALT levels correlated with serum mebendazole levels, normalized with stopping and rose again with rechallenge apparently without symptoms or jaundice).
- Colle I, Naegels S, Hoorens A, Hautekeete M. Granulomatous hepatitis due to mebendazole. J Clin Gastroenterol. 1999;28:44–5. [PubMed: 9916665](52 year old man treated with mebendazole for 3 days on two occasions 2 weeks apart developed fever during the second course and then found to have bilirubin 1.0 mg/dL, ALT 466 U/L, Alk P normal, 18% eosinophils and liver biopsy showing granulomas; no jaundice and rapid recovery: Case 1).
- Reuter S, Jensen B, Buttenschoen K, Kratzer W, Kern P. Benzimidazoles in the treatment of alveolar echinococcosis: a comparative study and review of the literature. J Antimicrob Chemother. 2000;46:451–6. [PubMed: 10980173](35 patients with alveolar echinococcosis were treated with either mebendazole or albendazole for 12-79 months; no severe side effects, but one patient was switched from albendazole to mebendazole because of ALT elevations).
- Keiser J, Utzinger J. Efficacy of current drugs against soil-transmitted helminth infections: systematic review and meta-analysis. JAMA. 2008;299:1937–48. [PubMed: 18430913](Systematic review of efficacy and safety of albendazole, mebendazole and pyrantel pamoate as therapy of Ascaris lumbricoides [roundworm], hookworm and whipworm; mebendazole was well tolerated in most studies, no significant adverse events were reported).
- Drugs for parasitic infections. Treat Guidel Med Lett. 2013;11 Suppl:e1–31.(Thorough description of drugs for parasitic infections in adults and children as well as a table of their major side effects; mebendazole can be used for ascariasis, pinworm, hookworm, whipworm, trichinellosis, and several less common parasitic infections; no hepatic related side effects mentioned).
- Mandal S, Mandal MD. Human cystic echinococcosis: epidemiologic, zoonotic, clinical, diagnostic and therapeutic aspects. Asian Pac J Trop Med. 2012;5:253–60. [PubMed: 22449514](Review of human enchinococcal cyst disease, its epidemiology, clinical manifestations, diagnosis, prevention and treatment which includes direct aspiration and surgery on the cysts and medical therapy with either mebendazole, albendazole or ivermectin often with praziquantel; no discussion of side effects).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, no cases were attributed to mebendazole or other anthelminthic medications).
- Silber SA, Diro E, Workneh N, Mekonnen Z, Levecke B, Steinmann P, Umulisa I, et al. Efficacy and Safety of a single-dose mebendazole 500 mg chewable, rapidly-disintegrating tablet for Ascaris lumbricoides and Trichuris trichiura infection treatment in pediatric patients: a double-blind, randomized, placebo-controlled, phase 3 study. Am J Trop Med Hyg. 2017;97:1851–1856. [PMC free article: PMC5805036] [PubMed: 29016336](Among 295 children [ages 1 to 15 years] with hookworm infection treated with mebendazole [single 500 mg chewable tablet] vs placebo, cure rates were 84% vs 11% for Ascaris lumbricoides and 34% vs 8% for Trichuris trichiuria, while adverse events arose in 6.3% vs 5.7%, mostly mild-to-moderate abdominal pain or distension, with no serious adverse events or deaths).
- Palmeirim MS, Ame SM, Ali SM, Hattendorf J, Keiser J. Efficacy and safety of a single dose versus a multiple dose regimen of mebendazole against hookworm infections in children: a randomised, double-blind trial. EClinicalMedicine. 2018 Jul;1:7–13. [PMC free article: PMC6537524] [PubMed: 31193620](Among 185 children with hookworm infestation [Ancylostoma duodenale] treated with mebendazole in a dose of 100 mg twice daily for 3 days vs a single 500 mg dose, cure rates were 98% vs 13%, while adverse events were similar consisting of mild-to-moderate abdominal pain, diarrhea and headache).
- Cañete R, Brito K, Brito I, Semper A, Gonzalez ME. Effectiveness and tolerability of 3-day mebendazole treatment of Giardia duodenalis infection in adults and children: two prospective, open-label phase IV trials. Curr Ther Res Clin Exp. 2018;89:43–47. [PMC free article: PMC6370949] [PubMed: 30792825](Among 522 children and 423 adults with giardia duodenalis infection treated in two open-label trials of a 3-day regimen of mebendazole [100 mg twice daily] in Cuba, cure rates were 86% and 93% and adverse events were abdominal pain [6% in both groups], nausea and vomiting [in 2-3% of children]).
- Palmeirim MS, Bosch F, Ame SM, Ali SM, Hattendorf J, Keiser J. Efficacy, safety and acceptability of a new chewable formulation versus the solid tablet of mebendazole against hookworm infections n children: An open-label, randomized controlled trial. EClinicalMedicine. 2020;27:100556. [PMC free article: PMC7599302] [PubMed: 33150325](Among 397 children [ages 3 to 12 years] with hookworm treated with a single dose of mebendazole in a solid vs chewable tablet form [500 mg], cure rates were similar [71% vs 69%] and adverse events were uncommon and mostly mild fever, headache, abdominal pain and nausea; no mention of hepatoxicity).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Mebendazole.[Ann Intern Med. 1979]Mebendazole.Keystone JS, Murdoch JK. Ann Intern Med. 1979 Oct; 91(4):582-6.
- Antiparasitic drugs.[Am Fam Physician. 1980]Antiparasitic drugs.Yoshikawa TT. Am Fam Physician. 1980 Mar; 21(3):132-8.
- Review Albendazole and Mebendazole as Anti-Parasitic and Anti-Cancer Agents: an Update.[Korean J Parasitol. 2021]Review Albendazole and Mebendazole as Anti-Parasitic and Anti-Cancer Agents: an Update.Chai JY, Jung BK, Hong SJ. Korean J Parasitol. 2021 Jun; 59(3):189-225. Epub 2021 Jun 21.
- Review Anthelmintic Agents.[LiverTox: Clinical and Researc...]Review Anthelmintic Agents.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- A comparative study of the effectiveness of mebendazole (Janssen) and generically equivalent mebendazole (Nordia) in intestinal helminthiasis in Papua New Guinean children.[P N G Med J. 1994]A comparative study of the effectiveness of mebendazole (Janssen) and generically equivalent mebendazole (Nordia) in intestinal helminthiasis in Papua New Guinean children.Wesche D, Barnish G. P N G Med J. 1994 Mar; 37(1):7-11.
- Mebendazole - LiverToxMebendazole - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...