NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Haloperidol is a conventional antipsychotic agent used in the treatment of acute and chronic psychosis. Haloperidol therapy is commonly associated with minor serum aminotransferase elevations and in very rare instances has been linked to clinically apparent acute liver injury.
Background
Haloperidol (hal" oh per' i dol) is a butyrophenone derivative which appears to act as a dopamine type 2 (D2) receptor antagonist, but has other central and peripheral effects. Haloperidol is indicated for the therapy of acute and chronic psychoses and for controlling tics and vocal utterances in Tourette syndrome. Haloperidol is also used for short-term treatment of severe behavior problems in children with hyperactivity. Haloperidol was approved for use in the United States in 1967, but is currently infrequently used, having been replaced in large part by the atypical antipsychotics, which have fewer extrapyramidal side effects. Haloperidol is available as tablets of 0.5, 1, 2, 5, 10 and 20 mg, as an oral solution and in several formulations for parenteral use in generic forms and under the brand names Haldol and Peridol. The dose of haloperidol ranges considerably based upon patient age, severity of illness and concomitant medications. The typical range of maintenance doses in adults is 0.5 to 5 mg two to three times daily. Common side effects include drowsiness, restlessness, dizziness, headache, blurred vision, tremor and weight gain. Rare, but potentially severe adverse events include cardiovascular events, QTc prolongation, tardive dyskinesia, neuroleptic malignant syndrome and embryo-fetal toxicity.
Hepatotoxicity
Liver test abnormalities have been reported to occur in 20% of patients on long term therapy with haloperidol, but elevations are uncommonly above 3 times the upper limit of normal. The aminotransferase abnormalities are usually mild, asymptomatic and transient, reversing even with continuation of medication. Instances of clinically apparent acute liver injury have been reported due to haloperidol, but they are uncommon. The onset of jaundice is within 2 to 6 weeks, and the pattern of serum enzyme elevations is typically cholestatic or mixed. Signs of hypersensitivity (fever, rash and eosinophilia) have been reported in some cases, but they are usually mild and self-limited; autoantibodies are rare.
Likelihood score: B (likely cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism by which haloperidol causes serum aminotransferase elevations is not known, but is likely due to production of a toxic intermediate of its metabolism. Haloperidol is extensively metabolized by the liver via sulfoxidation and oxidation, partially via CYP 3A4. Some instances of serum aminotransferase elevations occurring on haloperidol therapy may be due to nonalcoholic fatty liver disease caused by weight gain that occurs in at least one-quarter of treated patients, generally during the first 1 to 2 years of therapy.
Outcome and Management
The serum aminotransferase elevations that occur on haloperidol therapy are usually self-limited and do not require dose modification or discontinuation of therapy. Instances of acute liver failure and at least one case of chronic cholestasis suggestive of vanishing bile duct syndrome due to haloperidol have been reported. Patients with haloperidol induced liver injury probably do not have cross sensitivity to liver injury from the atypical antipsychotics. However, haliperidol has been associated with DRESS syndrome and features of immunoallergic hepatitis that also occur with the aromatic anticonvulsants such as phenytoin, lamotrigine and carbamazepine, making it likely that there is some cross reactivity and potential for recurrence with those agents.
Drug Class: Antipsychotic Agents
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Haloperidol – Generic, Haldol®, Peridol®
DRUG CLASS
Antipsychotic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Haloperidol | 52-86-8 | C21-H23-Cl-F-N-O2 |
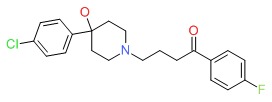 |
ANNOTATED BIBLIOGRAPHY
References updated: 25 March 2018
- Zimmerman HJ. Neuroleptic drugs. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 483-91.(Expert review of hepatotoxicity of neuroleptic drugs including haloperidol published in 1999 mentions that at least 22 cases of jaundice due to haloperidol have been reported, usually cholestatic, rarely leading to vanishing bile duct syndrome; minor enzyme elevations occur in 20% of patients on haloperidol).
- Larry D, Ripault MP. Hepatotoxicity of psychotropic drugs and drugs of abuse. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 443-62.(Review of hepatotoxicity of psychiatric agents mentions that rare cases of clinically apparent liver injury have been linked to haloperidol use, the usual clinical signature being cholestatic).
- Meyer JM. Pharmacotherapy of psychosis and mania. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 417-55.(Textbook of pharmacology and therapeutics).
- Crause J. Jaundice associated with haloperidol. Lancet 1963; 2: 890-1. Not in PubMed.(71 year old man with bronchitis and cor pulmonale developed jaundice 9 days after starting haloperidol [bilirubin not given; AST 120 U/L, Alk P 4 times ULN], jaundice resolving within 2 weeks of stopping).
- Gerle B. Clinical observations of the side effects of haloperidol. Acta Psychiatr Scand 1964; 40: 65-76. [PubMed: 14211383](Review of 70 reports of adverse events from 6500 patients receiving haloperidol; despite several published cases of suspected haloperidol induced liver injury, relationship to drug is uncertain; 3 cases described by the author are interpreted as co-incidental and unrelated to use of haloperidol with no recurrence on restarting).
- Crane GE. A review of clinical literature on haloperidol. Int J Neuropsychiat 1967; 3: Suppl 1: 110-27. [PubMed: 4860978](Review of 98 publications covering 5300 patients; liver impairment was reported in 13 cases, 9 with jaundice or severe hepatitis for a clinically apparent hepatotoxicity rate of ~1:500).
- Gerle B. European experience with haloperidol. Int J Neuropsychiat 1967; 3: S42-52.(Discussion of review by Crane [1967] mentioning that no evidence of significant liver injury was found in a retrospective review of 500 patients followed prospectively with “complete laboratory investigations”, which led the authors to conclude that routine monitoring was unnecessary).
- Fuller CM, Yassinger S, Donlon P, Imperato TJ, Ruebner B. Haloperidol-induced liver disease. West J Med 1977; 127: 515-8. [PMC free article: PMC1237937] [PubMed: 595591](Two cases; 33 year old woman developed jaundice, rash and fever 5 weeks after restarting haloperidol [bilirubin 4.2 mg/dL, ALT 130 U/L, Alk P 486 U/L, eosinophils 3%], ultimately resolving when drug was stopped; 27 year old woman developed jaundice 4 weeks after starting haloperidol [bilirubin 15.8 mg/dL, AST 85 U/L, Alk P 310 U/L], no rash or fever, resolving within 4 weeks of stopping).
- Dincsoy HP, Saelinger DA. Haloperidol-induced chronic cholestatic liver disease. Gastroenterol 1982; 83: 694-700. [PubMed: 7095372](15 year old man developed acute cholestatic hepatitis 4 weeks after starting haloperidol [bilirubin 10.8 mg/dL, ALT 99 U/L, Alk P 370 U/L, eosinophils 8%], which evolved into chronic cholestasis with jaundice and pruritus for 7 months, biopsy showing paucity of bile ducts and bridging fibrosis, but with ultimate recovery except for mild Alk P elevations 28 months later).
- Allison DB, Mentore JL, Heo M, Chandler LP, Cappelleri JC, Infante MC, Weiden PJ. Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry 1999; 156: 1686-96. [PubMed: 10553730](Systematic review of 81 articles on weight change with antipsychotics, using change after 10 weeks to compare agents: clozapine +5.7, olanzapine +4.2, chlorpromazine +4.2, risperidone +1.7, loxapine +0.6, haloperidol +0.5, ziprasidone +0.3, molindone -0.1, and pimozide -2.7 kgs).
- Gaertner I, Altendorf K, Batra A, Gaertner HJ. Relevance of liver enzyme elevations with four different neuroleptics: a retrospective review of 7,263 treatment courses. J Clin Psychopharmacol 2001; 21: 215-22. [PubMed: 11270919](Retrospective review of 233 inpatients treated with antipsychotic agents between 1980-92; some increase in ALT occurred in 78% of patients on clozapine and 50% on haloperidol; 3-fold increase occurred in ALT in 15% with clozapine and 2.4% with haloperidol; rates of 2-fold Alk P elevations were even lower [1% and 0.8%]).
- Bender S, Grohmann R, Engel RR, Degner D, Dittmann-Balcar A, Ruther E. Severe adverse drug reactions in psychiatric inpatients treated with neuroleptics. Pharmacopsychiatry 2004; 37 (Suppl 1): S46-53. [PubMed: 15052514](Severe adverse drug reactions among 35,293 inpatients; adverse events more common with atypicals [0.5-0.9%] than typical antipsychotics [0.02-0.2%]; increased liver enzymes most common adverse reaction to olanzapine, 4th in frequency to clozapine, 6th to haloperidol, 7th to risperidone; no mention of hepatitis or acute liver failure).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J; Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008; 135: 1924-34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease collected between 2004 and 2008 in the US, several antidepressants [duloxetine, sertaline, fluoxetine, amitryptilline], but none of the antipsychotic agents, were implicated).
- Torrent C, Amann B, Sanchez-Moreno J, Colom F, Feinares M, Comes M, Rosa AR, et al. Weight gain in bipolar disorder: pharmacological treatment as a contributing factor. Acta Psychiatr Scand 2008; 118: 4-18. [PubMed: 18498432](Review of frequency of weight gain in patients treated for bipolar disorders, most weight gain occurred with clozapine and olanzapine, but some weight gain also with quetiapine, risperidone, lithium, valproate and gabapentin; lesser amounts with haloperidol and not with carbamazepine or lamotrigine).
- Parsons B, Allison DB, Loebel A, Williams K, Giller E, Romano S, Siu C. Weight effects associated with antipsychotics: a comprehensive database analysis. Schizophr Res 2009; 110: 103-10. [PubMed: 19321312](Analysis of weight gain in 21 placebo controlled trials of various antipsychotics [~3300 patients]; average monthly weight gain in pounds was +0.1 with placebo, +0.8 olanzapine, +0.6 risperidone, -0.3 ziprasidone; a 5% increase in weight occurred after one year in 13% of placebo, 39% haloperidol, 20% ziprasidone, 45% risperidone and 60% olanzapine treated subjects).
- Lin CH, Kuo CC, Chou LS, Chen YH, Chen CC, Huang KH, Lane HY. A randomized, double-blind comparison of risperidone versus low-dose risperidone plus low-dose haloperidol in treating schizophrenia. J Clin Psychopharmacol 2010; 30: 518-25. [PubMed: 20814315](Controlled trial of 6 weeks of risperidone alone vs lower dose risperidone and haloperidol in 88 patients with schizophrenia; no change in mean ALT or AST levels in either group and no mention of hepatotoxicity).
- Reuben A, Koch DG, Lee WM; Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology 2010; 52: 2065-76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury including 4 due to psychotropic agents; one each for quetiapine, nefazodone, fluoxetine and venlafaxine, but none for phenothiazines or haloperidol).
- Molleston JP, Fontana RJ, Lopez MJ, Kleiner DE, Gu J, Chalasani N; Drug-induced Liver Injury Network. Characteristics of idiosyncratic drug-induced liver injury in children: results from the DILIN prospective study. J Pediatr Gastroenterol Nutr 2011; 53: 182-9. [PMC free article: PMC3634369] [PubMed: 21788760](Among 30 children with suspected drug induced liver injury, half [n=15] were due to antimicrobials [minocycline 4, INH 3, azithromycin 3] and the rest largely due to CNS agents and anticonvulsants; one case was attributed to perphenazine, but none to haloperidol).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 2013; 144: 1419-25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period including one non-fatal but icteric case due to chlorpromazine, but none were attributed to haloperidol).
- Fukata S, Kawabata Y, Fujisiro K, Katagawa Y, Kuroiwa K, Akiyama H, Terabe Y, et al. Haloperidol prophylaxis does not prevent postoperative delirium in elderly patients: a randomized, open-label prospective trial. Surg Today 2014; 44: 2305-13. [PubMed: 24532143](Among 121 elderly patients [75 years or older] undergoing surgery treated with haloperidol [2.5mg daily] or placebo for 3 days, rates of postoperative psychosis were similar as were adverse event rates; no mention of ALT elevations or hepatotoxicity).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol 2014; 13: 231-9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, but none were attributed to haloperidol).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52.e7. PubMed Citation. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 5 cases [0.6%] were attributed to antipsychotic agents including 3 to quetiapine and 12 to olanzapine, but none to haloperidol or other first generation antipsychotics).
- Douros A, Bronder E, Andersohn F, Klimpel A, Thomae M, Sarganas G, Kreutz R, et al. Drug-induced liver injury: results from the hospital-based Berlin Case-Control Surveillance Study. Br J Clin Pharmacol 2015; 79: 988-99. [PMC free article: PMC4456131] [PubMed: 25444550](Among 76 cases of suspected drug induced liver injury and 377 controls enrolled in a German, prospective hospital based registry, 6 cases [8%] but only 4 controls [1%] were receiving haloperidol, although the difference was said to be not significant).
- Drugs for psychotic disorders. Med Lett Drugs Ther 2016; 58 (1510): 160-4. [PubMed: 27960194](Concise review of medications available in the US for therapy of psychotic disorders; mentions that haloperidol is a first generation agent which are all associated with adverse events of sexual dysfunction, neuroleptic malignant syndrome, extrapyramidal symptoms, akathisia and tardive dyskinesia; no mention of ALT elevations or hepatotoxicity).
- Gründer G, Heinze M, Cordes J, Mühlbauer B, Juckel G, Schulz C, Rüther E, et al; NeSSy Study Group. Effects of first-generation antipsychotics versus second-generation antipsychotics on quality of life in schizophrenia: a double-blind, randomised study. Lancet Psychiatry 2016; 3: 717-29. [PubMed: 27265548](Among 149 patients started on either first- [haloperidol or flupentixol] or second-generation antipsychotics [olanzapine, quetiapine, aripiprazole] for 24 weeks, response rates were similar as were adverse events, weight gain being highest with olanzapine, quetiapine and haloperidol; median ALT and AST levels did not change significantly in any group).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Loxapine.[LiverTox: Clinical and Researc...]Review Loxapine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Molindone.[LiverTox: Clinical and Researc...]Review Molindone.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Quetiapine : A Review of its Use in Schizophrenia.[CNS Drugs. 1998]Quetiapine : A Review of its Use in Schizophrenia.Gunasekara NS, Spencer CM. CNS Drugs. 1998 Apr; 9(4):325-40.
- Review Lumateperone.[LiverTox: Clinical and Researc...]Review Lumateperone.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Iloperidone.[LiverTox: Clinical and Researc...]Review Iloperidone.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Haloperidol - LiverToxHaloperidol - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...