NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
The first generation sulfonylureas include acetohexamide, chlorpropamide, tolazamide and tolbutamide, oral hypoglycemic agents that are used in therapy of type 2 diabetes. They are well known, but rare causes of clinically apparent liver injury.
Background
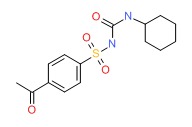
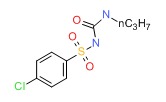
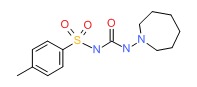
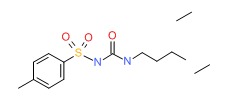
The sulfonylureas are substituted arylsulfonylureas, their differences being in the types of substitutions at the two ends of the molecule. The sulfonylureas lower blood glucose through an increase in secretion of insulin from the pancreatic beta cells. They may also have other extra-pancreatic hypoglycemic actions that are important during prolonged therapy. The first generation sulfonylureas have been largely replaced in routine use by the second generation agents, which are more potent and administered in lower doses largely on a once daily basis. Nevertheless, some patients are still maintained on first generation agents. Chlorpropamide (klor proe' pa mide) is available in generic forms and previously under the brand name of Diabinese in tablets of 100 and 250 mg, the recommended dose initially being 100 to 250 mg daily with increases every 5 to 7 days to a maximum of 750 mg daily. Tolazamide (tol az' a mide) is available in generic forms and under the brand name of Tolinase in tablets of 100, 250 and 500 mg, the recommended dose initially being 100 to 250 mg once daily, with increases thereafter to a maximum of 1000 mg daily. Tolbutamide (tol bue' ta mide) is available in generic forms and previously under the brand name of Orinase in tablets of 500 mg, the recommended dose initially being 1000 to 2000 mg daily in two divided doses, with increases thereafter to a maximum of 3000 mg daily. Acetohexamide (a seet" oh hex' a mide) was previously available in generic forms and under the brand name of Dymelor in tablets of 250 and 500 mg, the recommended dose initially being 250 to 500 mg daily with increases thereafter to a maximum of 1500 mg daily. Acetahexamide has been withdrawn from use and is no longer available. Common side effects of the first generation sulfonylureas include headache, dizziness, paresthesias, abdominal discomfort, and nausea. These agents are also associated with an “antabuse” like response to alcohol (flushing, nausea, palpitations, hypotension and dizziness) and patients should be advised not to drink alcoholic beverages while on these agents. All sulfonylureas can cause hypoglycemia.
Hepatotoxicity
Minor enzyme elevations have been reported to occur during sulfonylurea therapy in less than 1% of patients, rates that are similar to what occurs with placebo therapy. Clinically apparent liver injury from the sulfonylureas is rare, but has been reported for virtually all of the currently available forms and appears to represent a class effect, the pattern of injury being similar with the different agents. The liver injury usually appears within 2 to 12 weeks of starting the medication, usually with symptoms of fatigue, nausea and abdominal discomfort, followed by dark urine, itching and jaundice. Various combinations of hepatocellular and cholestatic injury have been described with sulfonylurea induced liver injury, and many cases are reported to be mixed. Allergic manifestations (fever, rash, eosinophilia) are found in up to half of cases, but autoantibody formation is not typical. Because this agent is usually given in combination with other hypoglycemic agents, many of which also cause liver injury, it can be difficult to establish whether the injury is due to the sulfonylurea or another agent. The timing of injury is perhaps most characteristic, although in some instances the hepatic injury has arisen many months to years after starting treatment, particularly after a recent increase in dosage. Recovery is usually rapid after the medication is stopped. Interestingly, the occurrence of hepatotoxicity with one sulfonylurea does not mean that similar liver injury will arise with another; many instances of a lack of recurrence with rechallenge (at lower doses) have been published. If toxicities arise, the second generation sulfonylureas should be preferred over the first generation agents. In recent summary recommendations on therapy of type 2 diabetes, the first generation sulfonylureas are usually not mentioned.
Likehood score: B (likely cause of liver injury as a class, most cases linked to chlorpropamide which was also the most commonly used in the past).
Mechanism of Injury
The mechanism of liver injury due to sulfonylureas is unknown, but suspected to be due to hypersensitivity. Cross reactivity to reactions to sulfonamides can occur, but not invariably, and the overall pattern of injury and outcome of sulfonylurea associated hepatic injury does not resemble the acute, immunoallergic pattern that is common with the sulfonamides. Nevertheless, the sulfonylureas should be used with caution in patients with sulfonamide hypersensitivity or a history of sulfonamide hepatotoxicity. In either case, rechallenge can lead to recurrence and should be avoided.
Outcome and Management
The liver injury from the sulfonylureas usually resolves rapidly once the agent is stopped, but chronic injury has been described in rare cases. Despite the usual cholestatic form of injury, cases of progressive hepatic failure and death have been described, particularly in the elderly or patients with multiple other medical problems and when the medication is not promptly withdrawn. There can be cross sensitivity between the different first generation sulfonylureas, and even switching to a second generation agent should be done with caution and appropriate monitoring. In cases in which multiple hypoglycemic agents are being used when the liver injury appears, rechallenge with the agent least likely associated with the injury is appropriate.
References to the first generation sulfonylureas and a representative case of hepatotoxicity due to their use are given in the Overview section on the Sulfonylureas (updated March 2018).
Drug Class: Antidiabetic Agents
Other Drugs in the Subclass, Sulfonylureas: Second Generation Sulfonylureas
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Acetohexamide – Dymelor®
Chlorpropamide – Diabinese®
Tolazamide – Tolinase®
Tolbutamide – Orinase®
DRUG CLASS
Antidiabetic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
- PubChem SubstanceRelated PubChem Substances
- METABOLISM OF ANTIDIABETIC SULFONYLUREAS IN MAN. I. BIOLOGICAL HALF-LIVES OF THE P-ACETYLBENZENESULFONYLUREAS, U-18536 AND ACETOHEXAMIDE AND THEIR METABOLITES.[Metabolism. 1965]METABOLISM OF ANTIDIABETIC SULFONYLUREAS IN MAN. I. BIOLOGICAL HALF-LIVES OF THE P-ACETYLBENZENESULFONYLUREAS, U-18536 AND ACETOHEXAMIDE AND THEIR METABOLITES.SMITH DL, VECCHIO TJ, FORIST AA. Metabolism. 1965 Mar; 14:229-40.
- The pharmacology of sulfonylureas.[Am J Med. 1981]The pharmacology of sulfonylureas.Skillman TG, Feldman JM. Am J Med. 1981 Feb; 70(2):361-72.
- A quantum chemical study with special reference to the sulfamyl group of sulfonylureas.[Jpn Circ J. 1970]A quantum chemical study with special reference to the sulfamyl group of sulfonylureas.Orita Y, Ando A, Takamitsu Y, Urakabe S, Shirai D. Jpn Circ J. 1970 Sep; 34(9):775-8.
- Review Glyburide and glipizide, second-generation oral sulfonylurea hypoglycemic agents.[Clin Pharm. 1984]Review Glyburide and glipizide, second-generation oral sulfonylurea hypoglycemic agents.Prendergast BD. Clin Pharm. 1984 Sep-Oct; 3(5):473-85.
- Review Sulfonylureas.[LiverTox: Clinical and Researc...]Review Sulfonylureas.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Sulfonylureas, First Generation - LiverToxSulfonylureas, First Generation - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...