NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Fosinopril is an angiotensin-converting enzyme (ACE) inhibitor used in the therapy of hypertension and heart failure. Fosinopril is associated with a low rate of transient serum aminotransferase elevations during therapy and has been linked to rare instances of acute liver injury.
Background
Fosinopril (fos sin' oh pril) is an ACE inhibitor approved for use alone or in combination with other agents as therapy of hypertension and heart failure. Like other ACE inhibitors, fosinopril inhibits the conversion of angiotensin I, a relatively inactive molecule, to angiotensin II which is the major mediator of vasoconstriction and volume expansion induced by the renin-angiotensin system. Other enzymes besides that which converts angiotensin I to II may also be inhibited, which may account for some of the dose related side effects of the ACE inhibitors. Fosinopril was approved for use in the United States in 1991 and is available in 10, 20 and 40 mg tablets in generic forms and under the trade name Monopril. The typical dose in adults is 10 mg once daily initially, with gradual adjustment based upon blood pressure response and tolerance. The usual maintenance dosage is 20 to 40 mg daily and the maximum 80 mg in one or two divided doses administered long term. Fosinopril is also available in fixed combinations with hydrochlorothiazide (Monopril HCT). Common side effects include dizziness, fatigue, headache, cough, gastrointestinal upset and skin rash.
Hepatotoxicity
Fosinopril, like other ACE inhibitors, has been associated with a low rate of serum aminotransferase elevations (<2%) that, in controlled trials, was no higher than with placebo therapy. These elevations were transient and rarely required dose modification. Rare instances of clinically apparent acute liver injury have been reported in association with fosinopril therapy, but they have been too few to characterize the pattern of injury reliably. The onset of symptoms was within 2 to 12 weeks of starting therapy and the serum enzyme pattern was cholestatic. In one instance, cholestasis was prolonged and relapsing and associated with persistent elevations in serum alkaline phosphatase and GGT, suggestive of vanishing bile duct syndrome (Case 1). In published cases, immunoallergic manifestations (rash, fever, eosinophilia) were infrequent and patients did not develop autoantibodies. Other ACE inhibitors have been occasionally associated with a hepatocellular pattern of liver injury and cases with a long latency (one or more years) have been described as well. These features have not been clearly linked to fosinopril hepatotoxicity.
Likelihood score: D (possible rare cause of clinically apparent liver injury).
Mechanism of Injury
The cause of the minor serum aminotransferase elevations with fosinopril therapy is not known. The cases of clinically apparent liver injury due to fosinopril were clearly idiosyncratic and likely due to a reaction to a metabolite. Fosinopril is hydrolyzed in the liver to its active metabolite fosinoprilat.
Outcome and Management
Most instances of acute liver injury reported with fosinopril use have been self limited, but there have been rare reports of acute liver failure due to other ACE inhibitors as well as reports of cholestatic hepatitis leading to prolonged jaundice. Patients with severe fosinopril induced acute liver injury should avoid use of other ACE inhibitors, although cross sensitivity to liver injury among the members of this class of agents has not always been shown.
References to the safety and potential hepatotoxicity of fosinopril are given in the Overview section on the Angiotensin-Converting Enzyme (ACE) Inhibitors.
Drug Class: Antihypertensive Agents, Angiotensin-Converting Enzyme Inhibitors
CASE REPORT
Case 1. Acute hepatitis due to fosinopril.
[Modified from: Nunes AC, Amaro P, Maçias F, et al. Fosinopril-induced prolonged cholestatic jaundice and pruritus: first case report. Eur J Gastroenterol Hepatol 2001; 13: 279-82.] PubMed Citation]
A 61 year old man with hypertension and a history of aortic aneurysm developed jaundice and pruritus 3 weeks after starting fosinopril (20 mg daily), metoprolol (50 mg twice daily), and diazepam (5 mg daily). Two weeks later he sought medical advice. He had no history of liver disease or risk factors for viral hepatitis. His serum enzymes had been normal on several occasions during the previous few months. He drank the equivalent of 3 to 4 alcoholic beverages daily (40 grams/day). He was taking no other medications. Physical examination showed jaundice but no fever, rash or peripheral manifestations of chronic liver disease. Laboratory testing showed marked elevation in serum bilirubin (19.1 mg/dL) and alkaline phosphatase (421 U/L), with only modest elevations in serum aminotransferase levels (ALT 70 U/L, AST 47 U/L) (Table). Tests for acute hepatitis A, B and C were negative and autoantibody tests were negative. He had no eosinophilia or elevations in immunoglobulin levels. Abdominal ultrasound and computerized tomography showed no evidence of gallstones or biliary obstruction. A liver biopsy showed severe intrahepatic cholestasis, but no bile duct damage and no changes suggestive of alcoholic liver disease. All medications were stopped on admission and he was treated with ursodiol, colestipol and hydroxyzine for the cholestasis and pruritus. He improved slowly and had multiple complications during a two month period of hospitalization (renal failure requiring dialysis, duodenal ulcer bleeding, and septicemia). He remained jaundiced for 4 months, had troublesome pruritus for 6 months, and still had marked elevations in serum alkaline phosphatase and occasional episodes of pruritus 18 months after his initial presentation.
Key Points
| Medication: | Fosinopril (20 mg daily) |
|---|---|
| Pattern: | Cholestatic (R=0.4) |
| Severity: | 4+ (jaundice, hospitalization, other organ failure) |
| Latency: | 3 weeks |
| Recovery: | Partial over 6-18 months |
| Other medications: | Metoprolol, diazepam |
Laboratory Values
| Time After Starting* | Time After Stopping | GGT* (U/L) | Alk P* (U/L) | Bilirubin* (mg/dL) | Other |
|---|---|---|---|---|---|
| 1.2 months | 0 | 73 | 421 | 19.1 | Admission |
| 2 months | 1 month | 55 | 260 | 40.0 | Liver biopsy |
| 3 months | 2 month | 40 | 230 | 13.0 | Discharge |
| 5 months | 4 months | 75 | 580 | 1.0 | Pruritus requiring therapy |
| 9 months | 8 months | 80 | 410 | 1.0 | |
| 1year | 1 year | 90 | 300 | 1.0 | |
| 1.5 years | 1.5 years | 95 | 320 | 1.0 | Minimal pruritus |
| Normal Values | <50 | <117 | <1.2 | ||
* Values and dates in Table estimated from Figure 2.
Comment
The patient developed a severe acute cholestatic hepatitis within a few weeks of starting fosinopril which worsened for a month despite stopping therapy. A liver biopsy showed severe cholestasis, but without evidence of bile duct injury. The subsequent course, however, was typical for vanishing bile duct syndrome although the amount of bile duct loss was obviously not severe enough to result in frank biliary cirrhosis or hepatic failure. Slow and sometimes incomplete recovery is typical of severe cholestatic hepatitis due to medications.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Fosinopril – Generic, Monopril®
DRUG CLASS
Angiotensin-Converting Enzyme Inhibitors
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Fosinopril | 98048-97-6 | C30-H46-N-O7-P |
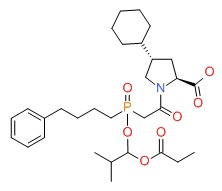 |
- PubChem SubstanceRelated PubChem Substances
- Review Angiotensin-Converting Enzyme Inhibitors.[LiverTox: Clinical and Researc...]Review Angiotensin-Converting Enzyme Inhibitors.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Ramipril.[LiverTox: Clinical and Researc...]Review Ramipril.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Captopril.[LiverTox: Clinical and Researc...]Review Captopril.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Enalapril.[LiverTox: Clinical and Researc...]Review Enalapril.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Lisinopril.[LiverTox: Clinical and Researc...]Review Lisinopril.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Fosinopril - LiverToxFosinopril - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...