NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Fondaparinux is a synthetic inhibitor of factor Xa which given by injection and is used as an anticoagulant to treat as well as prevent venous thromboembolism. Fondaparinux has been associated with a low rate of serum aminotransferase elevations during therapy, but has not been implicated in cases of clinically apparent, idiosyncratic liver injury.
Background
Fondaparinux (fon" da par' in ux) is a synthetic inhibitor of factor Xa which blocks the activity of this clotting factor indirectly by binding to and activating antithrombin III. Fondaparinux is composed of five monomeric sugars that are identical to the sequence present in heparin that comprises the high affinity binding site for antithrombin III. Unlike standard and low molecular weight heparins, however, fondaparinux is specific for factor Xa and has no effect on thrombin or other clotting factors. As a result, fondaparinux has a more predictable and reproducible anticoagulant effect and can be administered in a fixed dose once daily and does not require monitoring for anticoagulant effect. Fondaparinux was approved for use in the United States in 2001 and current indications include prevention of deep vein thromboses in high risk individuals after hip fracture surgery, hip or knee replacement surgery or abdominal surgery and active treatment of deep vein thrombosis with or without pulmonary embolism (in combination with warfarin). Fondaparinux is available as solution for injection in prefilled syringes of 2.5, 5, 7.5 or 10 mg generically and under the brand name Arixtra. The typical dose for prophylaxis of deep vein thrombosis is 2.5 mg subcutaneously once daily for 5 to 30 days. The dose regimen for treatment of deep vein thrombosis and pulmonary embolism is 5 to 10 mg (based upon body weight) subcutaneously once daily for at least 5 days and until a stable INR is achieved with warfarin. Side effects include bleeding and thrombocytopenia, but are less common than with heparin. Noncoagulation related side effects are uncommon but can include anemia, hypokalemia, insomnia, confusion, dizziness, hypotension, rash, and purpura. Rare but potentially severe adverse reactions include severe bleeding episodes including spinal or epidural hematomas.
Hepatotoxicity
Fondaparinux therapy is associated with a low rate of serum aminotransferase elevations during therapy, with levels above 3 times the upper limit of normal occurring in 1% to 3% of patients, a lower rate than occurs with heparin (~8%) or low molecular weight heparins (4% to 12%) but higher than occurs with placebo (<1%). The liver test abnormalities during fondaparinux therapy were generally mild, not associated with jaundice or symptoms and not requiring drug discontinuation. Typically, liver test abnormalities arose during the first week of therapy and resolved quickly even without dose modification or discontinuation. The abnormalities appear to resemble those that occur with heparin and the low molecular weight heparins. A case reported of marked ALT and AST elevations without jaundice arising within 2 days of starting fondaparinux and resolving rapidly on stopping has been reported. Fondaparinux has not been in wide clinical use, but cases of idiosyncratic clinically apparent liver injury have not been reported in the literature. Thus, while mild-to-moderate serum aminotransferase elevations are common during fondaparinux therapy, clinically apparent liver injury with jaundice has not been reported.
Likelihood score: E (unlikely cause of clinically apparent liver injury).
Mechanism of Injury
Fondaparinux may cause a similar direct, self-limited hepatotoxicity as occurs with the use of natural and low molecular weight heparins. If fondaparinux causes idiosyncratic drug induced liver injury, the mechanism of this effect is not known. Fondaparinux has little hepatic metabolism and does not affect CYP 450 enzyme activity in the liver.
Outcome and Management
The serum aminotransferase elevations that occur during fondaparinux therapy are usually self-limited and do not require dose modification or discontinuation of therapy. No convincing instances of clinically apparent or severe acute liver injury have been linked to fondaparinux in the published literature. Because of its unique chemical structure, it is unlikely that there is cross sensitivity to liver injury with other factor Xa inhibitors such as rivroxaban
Drug Class: Antithrombotic Agents, Anticoagulants
Other Drugs in the Subclass, Anticoagulants, Oral Factor Xa Antagonists: Apixaban, Betrixaban, Edoxaban, Rivaroxaban
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Fondaparinux – Generic, Arixtra®
DRUG CLASS
Antithrombotic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Fondaparinux | 104993-28-4 | C31-H53-N3-O49-S8 |
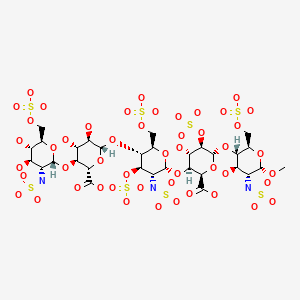
|
ANNOTATED BIBLIOGRAPHY
References updated: 22 February 2023
- Zimmerman HJ. Heparin. Drugs used in cardiovascular disease. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 639-412.(Textbook of hepatotoxicity published in 1999 before availability of fondaparinux).
- De Marzio DH, Navarro VJ. Hepatotoxicity of cardiovascular and antidiabetic drugs. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 519-40.(Review of hepatotoxicity of drugs used in cardiovascular disease; the heparins and fondaparinux are not discussed).
- Weitz JI. Blood coagulation and anticoagulant, thrombolytic, and antiplatelet drugs. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 849-76.(Textbook of pharmacology and therapeutics; fondaparinux is a synthetic five-saccharide analogue of the natural pentasaccharide sequence found in heparin).
- Fondaparinux (Arixtra), a new anticoagulant. Med Lett Drugs Ther. 2002;44(1130):43–4. [PubMed: 12011755](Concise review of the mechanism of action, clinical efficacy, safety and cost of fondaparinux shortly after its approval for use in the United States; no mention of ALT elevations or hepatotoxicity).
- Turpie AG, Bauer KA, Eriksson BI, Lassen MR. Fondaparinux vs enoxaparin for the prevention of venous thromboembolism in major orthopedic surgery: a meta-analysis of 4 randomized double-blind studies. Arch Intern Med. 2002;162:1833–40. [PubMed: 12196081](Analysis of 4 controlled trials of fondaparinux versus enoxaparin in 7237 patients after orthopedic surgery; rates of side effects were similar in the two groups, but rates of liver injury and ALT elevations were not mentioned).
- Büller HR, Davidson BL, Decousus H, Gallus A, Gent M, Piovella F, Prins MH, et al. Matisse Investigators. Fondaparinux or enoxaparin for the initial treatment of symptomatic deep venous thrombosis: a randomized trial. Ann Intern Med. 2004;140:867–73. [PubMed: 15172900](Controlled trial of fondaparinux vs enoxaparin in 2205 patients with deep venous thromboses found similar efficacy and safety; no mention of ALT elevations or hepatotoxicity).
- Fiessinger JN, Huisman MV, Davidson BL, Bounameaux H, Francis CW, Eriksson H, Lundström T, et al. THRIVE Treatment Study Investigators. Ximelagatran vs low-molecular-weight heparin and warfarin for the treatment of deep vein thrombosis: a randomized trial. JAMA. 2005;293:681–9. [PubMed: 15701909](Controlled trial of ximelagatran versus enoxaparin and warfarin in 2489 patients with deep vein thromboses; ALT elevations above 3 times ULN occurred in 9.6% of ximelagatran vs 2% of enoxaparin/warfarin treated patients, and at least one patient on ximelagatran developed clinically apparent liver injury).
- Agnelli G, Bergqvist D, Cohen AT, Gallus AS, Gent M., PEGASUS investigators. Randomized clinical trial of postoperative fondaparinux versus perioperative dalteparin for prevention of venous thromboembolism in high-risk abdominal surgery. Br J Surg. 2005;92:1212–20. [PubMed: 16175516](Among 2048 patients treated with fondaparinux or dalteparin for 5 to 9 days, side effects were similar in the two groups; no discussion of liver injury or ALT elevations).
- Turpie AG. The safety of fondaparinux for the prevention and treatment of venous thromboembolism. Expert Opin Drug Saf. 2005;4:707–21. [PubMed: 16011449](Review of clinical efficacy and safety of fondaparinux; ALT elevations above 3 times the ULN occurred in 1.3-2.6% of patients on fondaparinux compared to 0.7% on placebo, 3.9-12.3% on enoxaparin, and 8% on heparin; abnormalities were usually asymptomatic and not associated with bilirubin elevations).
- Cohen AT, Davidson BL, Gallus AS, Lassen MR, Prins MH, Tomkowski W, Turpie AG, et al. ARTEMIS Investigators. Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ. 2006;332:325–9. [PMC free article: PMC1363908] [PubMed: 16439370](Controlled trial of fondaparinux versus placebo in 849 patients 60 years or older admitted for illness requiring bed rest, no discussion of liver injury or ALT elevations).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected from 2004 to 2008, none were attributed to fondaparinux or other anticoagulants).
- Decousus H, Prandoni P, Mismetti P, Bauersachs RM, Boda Z, Brenner B, Laporte S, et al. CALISTO Study Group. Fondaparinux for the treatment of superficial-vein thrombosis in the legs. N Engl J Med. 2010;363:1222–32. [PubMed: 20860504](Among 3002 patients with superficial vein thrombosis in the legs treated with fondaparinux or placebo for 45 days, side effects were similar in the two groups; liver injury and ALT elevations not mentioned).
- Choice of drugs for heparin-induced thrombocytopenia. Med Lett Drugs Ther. 2012;54(1391):43–4. [PubMed: 22643441](Heparin therapy can cause antibody mediated thrombocytopenia because it binds to platelet factor 4 making it antigenic, a feature not shared by fondaparinux which can be used in patients needing anticoagulation who develop this complication; no mention of ALT elevations or hepatoxicity in discussion of adverse effects).
- Orostegui L, Medejel N, Kone-Paut I, Dreyfus M, Benhamou D. Fondaparinux (Arixtra *) hepatotoxicity in a 6 year-old child. J Hepatol. 2013;58:195–8. [PubMed: 23023013](5 year old child with a thrombosed vascular malformation developed marked liver test abnormalities 30 hours after starting fondaparinux [bilirubin 0.6 mg/dL, ALT 509 U/L, AST 720 U/L, Alk P 278 U/L], resolving within 5 days of stopping and later tolerating enoxaparin).
- Hosaka K, Saito S, Ishii T, Sumino T, Ryu K, Suzuki G, Suzuki T, Tokuhashi Y. Safety of fondaparinux versus enoxaparin after TKA in Japanese patients. Orthopedics. 2013;36:e428–33. [PubMed: 23590781](Among 277 Japanese patients undergoing total knee replacement treated with enoxaparin or fondaparinux, rates of deep venous thrombosis were similar in the two groups, but ALT elevations were less with fondaparinux [8% vs 30%], but all were transient and without jaundice or symptoms).
- Antithrombotic drugs. Med Lett Drugs Ther. 2014;56(1454):103–9. [PubMed: 25337986](Concise review of antithrombotic drugs including fondaparinux; discussion of its adverse side effects does not mention ALT elevations or hepatotoxicity).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients With drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 patients with clinically apparent drug induced liver injury enrolled in a US prospective study over an 8 year period, 2 were attributed to antithrombotic agents including 1 to prasugrel [platelet inhibitor] and 1 to dalteparin [low molecular weight heparin], but none to fondaparinux).
- Zhang ZH, Zhang JW, He P, Zhou Y, Sun CY. Fondaparinux is effective for acute portal vein thrombosis in decompensated cirrhotic patients. Medicine (Baltimore). 2017;96:e8256. [PMC free article: PMC5662382] [PubMed: 29049216](Among 7 patients with advanced cirrhosis who developed acute portal vein thrombosis and were treated with fondaparinux for variable periods of time, all had recanalization and "no side effects.... occurred in any of the patients").
- Yang X, Li N, Guo T, Guan X, Tan J, Gao X, Wu Y, Jia L, et al. Comparison of the effects of low-molecular-weight heparin and fondaparinux on liver function in patients with pulmonary embolism. J Clin Pharmacol. 2020;60:1671–1678. [PubMed: 32639644](Among 463 adults with pulmonary embolus treated with low molecular weight heparins or with fondaparinux, 79 [17%] developed evidence of liver injury that was generally mild and less than 3 times ULN; abnormalities arising in 15% of 377 on edoxaban, 32% of 59 on nadroparin, and 7.4% of 27 on fondaparinux).
- Ma J, Chalasani NP, Schwantes-An L, Björnsson ES. Review article: the safety of anticoagulants and antiplatelet agents in patients with cirrhosis. Aliment Pharmacol Ther. 2023;57:52–71. [PubMed: 36373544](Review of the safety of anticoagulant use in patients with cirrhosis mentions that drug induced liver injury is uncommon in patients with preexisting cirrhosis, at least in those with compensated [Child’s Class A] or mildly compensated [Child’s Class B] cirrhosis).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Fondaparinux: a Factor Xa inhibitor for antithrombotic therapy.[Expert Opin Pharmacother. 2004]Review Fondaparinux: a Factor Xa inhibitor for antithrombotic therapy.Turpie AG. Expert Opin Pharmacother. 2004 Jun; 5(6):1373-84.
- Review The synthetic pentasaccharide fondaparinux: first in the class of antithrombotic agents that selectively inhibit coagulation factor Xa.[Semin Thromb Hemost. 2002]Review The synthetic pentasaccharide fondaparinux: first in the class of antithrombotic agents that selectively inhibit coagulation factor Xa.Petitou M, Duchaussoy P, Herbert JM, Duc G, El Hajji M, Branellec JF, Donat F, Necciari J, Cariou R, Bouthier J, et al. Semin Thromb Hemost. 2002 Aug; 28(4):393-402.
- Review Factor Xa inhibition in the prevention of venous thromboembolism and treatment of patients with venous thromboembolism.[Curr Opin Pulm Med. 2002]Review Factor Xa inhibition in the prevention of venous thromboembolism and treatment of patients with venous thromboembolism.Bauer KA, Eriksson BI, Lassen MR, Turpie AG. Curr Opin Pulm Med. 2002 Sep; 8(5):398-404.
- Review Venous thromboembolism prophylaxis: role of factor xa inhibition by fondaparinux.[Surg Technol Int. 2004]Review Venous thromboembolism prophylaxis: role of factor xa inhibition by fondaparinux.Turpie AG. Surg Technol Int. 2004; 13:261-7.
- Review Pentasaccharides for the prevention of venous thromboembolism.[Cochrane Database Syst Rev. 2016]Review Pentasaccharides for the prevention of venous thromboembolism.Dong K, Song Y, Li X, Ding J, Gao Z, Lu D, Zhu Y. Cochrane Database Syst Rev. 2016 Oct 31; 10(10):CD005134. Epub 2016 Oct 31.
- Fondaparinux - LiverToxFondaparinux - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...