NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Etodolac is a nonsteroidal antiinflammatory drug (NSAID) that is available by prescription only and is used long term for therapy of chronic arthritis and short term for acute pain. Etodolac has been linked to rare instances of clinically apparent drug induced liver disease.
Background
Etodolac (e toe' doe lak) belongs to the acetic acid derivative class of NSAIDs similar to diclofenac, sulindac, ketorolac and indomethacin. Like other NSAIDs, etodolac is a potent cyclo-oxygenase (Cox-1 and -2) inhibitor which blocks the formation of prostaglandins that are important in pain and inflammatory pathways. It has analgesic as well as antipyretic and antiinflammatory activity. Etodolac was approved in the United States in 1991 and is available by prescription only. Currently more than 3 million prescriptions are filled yearly. Current indications include treatment of osteoarthritis and rheumatoid arthritis and for short term treatment of acute pain. Etodolac is available as capsules or tablets in doses of 200, 300, 400 and 500 mg generically and under the trade name Lodine. Extended release formulations of 400, 500 and 600 mg are also available for once or twice daily dosing. The recommended dose is 400 to 1200 mg in 2 to 4 divided doses daily, based upon response and tolerance. Like other NSAIDs, etodolac is generally well tolerated, but side effects can include headache, dizziness, somnolence, dyspepsia, nausea, abdominal discomfort, heartburn, diarrhea, peripheral edema, pruritus and hypersensitivity reactions.
Hepatotoxicity
Prospective studies show that 1% to 2% of patients taking etodolac experience at least transient serum aminotransferase elevations. These may resolve even with drug continuation. Marked aminotransferase elevations (>3 fold elevated) occur in <1% of patients. Clinically apparent liver injury with jaundice from etodolac is rare but several convincing cases have been published. The latency to onset ranged a few days to several months and the pattern of enzyme elevations has been described as cholestatic, hepatocellular and mixed. Perhaps the most typical presentation is with jaundice 3 to 6 months after starting etodolac with a mixed or hepatocellular pattern of injury, and fairly rapid recovery on stopping. Immunoallergic and autoimmune features are uncommon. These features are also typical of diclofenac hepatotoxicity. Several cases of fatal acute liver failure in patients taking etodolac have been described, some of which demonstrate a pattern of hyperacute hepatic necrosis resembling acetaminophen overdose or acute hepatic ischemia. Interestingly, etodolac causes a false positive reaction on dipstick testing for bilirubin in urine.
Likelihood score: C (probable rare cause clinically apparent liver injury).
Mechanism of Injury
The mechanism of etodolac hepatotoxicity is not known, but likely to be due to an idiosyncratic reaction to an intermediate of its metabolism. Etodolac is extensively metabolized by the liver.
Outcome and Management
Severity ranges from asymptomatic elevations in serum aminotransferase levels, to symptomatic hepatitis with or without jaundice. A single fatal case has been described. Patients with etodolac induced clinically apparent liver injury should avoid other acetic acid derivatives such as sulindac, diclofenac, ketorolac, tolmetin and indomethacin.
Drug Class: Nonsteroidal Antiinflammatory Drugs
CASE REPORTS
Case 1. Acute hepatitis attributed to etodolac.
[Modified from Schmeltzer PA, Kosinski AS, Kleiner DE, Hoofnagle JH, Stolz A, Fontana RJ, Russo MW; Drug-Induced Liver Injury Network (DILIN). Liver injury from nonsteroidal anti-inflammatory drugs in the United States. Liver Int 2016; 36: 603-9. PubMed Citation]
A 55 old year woman developed anorexia followed by skin rash 7 months after starting etodolac (400 mg twice daily) for osteoarthritis. She stopped the etodolac, but went on to develop dark urine and jaundice. She had no history of liver disease, alcohol abuse, risk factors for viral hepatitis or drug allergieis. Her other medical conditions included hypothyroidism for which she took levothyroxine and reactive airway disease for which she had taken montelukast daily for several years. She also took multivitamins, but denied exposure to other over-the-counter or herbal products. On examination, she had an erythematous rash over the thorax, but no fever or lymphadenopathy, and no signs of chronic liver disease. Laboratory tests showed total serum bilirubin of 4.0 mg/dL, ALT 661 U/L, AST 501 U/L, alkaline phosphatase 128 U/L and albumin 4.0 g/dL. Tests for hepatitis A, B, C (including HCV RNA) and E were negative as were ANA and SMA. An abdominal ultrasound showed gallstones, but no evidence of biliary obstruction. She was monitored as an outpatient and improved rapidly. Her symptoms resolved within one month and all liver tests were normal within two months of the initial presentation (Table). She did not restart etodolac.
Key Points
| Medication: | Etodolac |
| Pattern: | Hepatocellular (R=19.3) |
| Severity: | 2+ (jaundiced but not hospitalized) |
| Latency: | 7 months |
| Recovery: | 7 weeks |
| Other medications: | Montelukast, levothyroxine, multivitamins |
Laboratory Values
Comment
This woman developed a mild, but clinically apparent acute hepatitis 7 months after starting daily etodolac therapy for osteoarthritis. Immunoallergic features were present (rash), but not prominent (eosinophil counts were not available). Other causes of acute hepatitis were excluded. Montelukast can cause acute liver injury, but she had been on this medication for several years. Rechallenge with motelukast with careful monitoring would have been appropriate.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Etodolac – Generic, Lodine®
DRUG CLASS
Nonsteroidal Antiinflammatory Drugs
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Etodolac | 41340-25-4 | C17-H21-N-O3 |
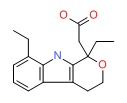 |
ANNOTATED BIBLIOGRAPHY
References updated: 05 April 2018
- Zimmerman HJ. Drugs used to treat rheumatic and musculospastic disease. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 517-553.(Expert review of hepatotoxicity published in 1999; mentions that etodolac is associated with a low rate of serum aminotransferase elevations and has been implicated in a few cases of acute liver injury with jaunidce).
- Lewis JH, Stine JG. Nonsteroidal anti-inflammatory drugs and leukotriene receptor antagonists. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 369-401. (Review of hepatotoxicity of NSAIDs;mentions that ALT elevations occur in <1% of patients on etodolac and discusses a case report of acute liver failure [Mabee et al 1995]).
- Grosser T, Smyth E, FitzGerald GA. Anti-inflammatory, antipyretic, and analgesic agents: pharmacotherapy of gout. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 959-1004.(Textbook of pharmacology and therapeutics).
- Boldy DA, Hale KA, Vale JA. Etodolac overdose. Hum Toxicol 1988; 7: 203-4. [PubMed: 2967796](53 year old woman took an overdose of etodolac [44 tablets] and underwent gastric lavage 2 hours later, remaining asymptomatic and with no abnormalities in "biochemical profile", testing showing therapeutic plasma levels, suggesting that gastric lavage had been highly effective).
- Karbowski A. A global safety evaluation of etodolac. Clin Rheumatol 1989; 8 (Suppl 1): 73-9. [PubMed: 2525986](Review of the literature and data on file with sponsor on safety of etodolac: liver test abnormalities occurred in 1-2% of treated patients, but none withdrew because of laboratory abnormalities. In clinical practice studies on 543 patients there were no reports of hepatitis or liver function test abnormalities).
- Zimmerman HJ. Update of hepatotoxicity due to classes of drugs in common clinical use: non-steroid drugs, anti-inflammatory drugs, antibiotics, antihypertensives, and cardiac and psychotropic agents. Semin Liver Dis 1990; 10: 322-8. [PubMed: 2281340](Extensive review article on liver injury due to NSAIDs; mentions that etodolac has “led to little or no hepatic injury”).
- Schattenkirchner M. An update safety profile of etodolac in several thousand patients. Eur J Rheumatol Inflamm 1990; 10: 56-65. [PubMed: 2146132](In clinical trials, 31 of 3,302 [0.9%] patients on etodolac stopped treatment because of elevated liver enzymes [ALT, AST or Alk P] or bilirubin, compared to 0.4% of placebo- and 4% of aspirin-recipients).
- Serni U. Global safety of etodolac: reports from worldwide postmarketing surveillance studies. Rheumatol Int 1990; 10 (Suppl): 23-7. [PubMed: 2150568](Summary of 4 postmarketing studies of safety of etodolac from Europe in over 8000 patients; in a French study of 1269 patients, 2 cases of hepatoxicity were reported, one with jaundice only and one with cholestatic hepatitis).
- Benhamou CL. Large-scale open trials with etodolac (Lodine) in France: an assessment of safety. Rheumatol Int 1990; 10 Suppl: 29-34. [PubMed: 2150569](Analysis of safety in 4997 patients in randomized clinical trials of 30 day course of etodolac in rheumatoid arthritis and osteoarthritis, found one patient with marked ALT elevations at 15 days and one case of cholestatic hepatitis, both resolving; in 51,355 patients in postmarketing surveillance, only 2 hepatic adverse reactions were reported, but no details given).
- Schattenkirchner M. Double-blind comparison of etodolac and piroxicam in patients with rheumatoid arthritis. Curr Med Res Opin 1991; 12: 497-50. [PubMed: 1837260](60 patients given etodolac [200 mg twice daily] or piroxicam [20 mg once daily] for 12 weeks with blood chemistries done at start and stop of therapy; “There were no clinically significant changes in laboratory parameters in either treatment group”).
- Etodolac. Medical Letter 1991; 33: 79-80. [PubMed: 1830919](Short review of etodolac indicating that it is as effective as other NSAIDs but unlikely to be more safe; also mentions that drug associated hepatic dysfunction has been reported).
- Latrive JP, Combaux D, Crepin P, Brbara JC. Acute hepatitis associated with etodolac therapy. Therapie 1992; 47: 82. [PubMed: 1387992](32 year old woman with anklyosing spondylitis developed jaundice 5 days after starting etodolac [bilirubin 6.3 mg/dL, ALT 8 times and Alk P 2.7 times ULN] with complete resolution in 2 months).
- Schattenkirchner M. The safety profile of sustained-release etodolac. Rheumatol Int 1993; 13 (Suppl 2): S31-5. [PubMed: 8210923]PubMed Citation (Among 539 patients with osteoarthritis or rheumatoid arthritis given once daily sustained release etodolac in 4 open-label studies for up to 1 year; “most laboratory abnormalities were transient and did not affect the patient’s health status.” 6 patients withdrew because of laboratory abnormalities, all of which resolved except for one patient with preexisting liver test abnormalities; no mention of hepatitis or jaundice).
- García Rodríguez LA, Williams R, Derby LE, Dean AD, Jick H. Acute liver injury associated with nonsteroidal anti-inflammatory drugs and the role of risk factors. Arch Intern Med 1994; 154: 311-6. PubMed Citation . [PubMed: 8297198](Population based study of 625,307 UK subjects who received at least one prescription for one of 12 NSAIDs [etodolac not mentioned], of whom 35 subsequently had liver injury: 12 only liver tests abnormal, 23 acute symptomatic injury for and overall incidence of 1 per 100,000 prescriptions or 4 per 100,000 users).
- Schnitzer TJ, Ballard IM, Constantine G, McDonald P. Double-blind, placebo-controlled comparison of the safety and efficacy of orally administered etodolac and nabumetone in patients with active osteoarthritis of the knee. Clin Therapeut 1995; 17: 602-12. [PubMed: 8565024](In a prospective controlled trial, mild ALT elevations occurred in 3 of 89 nabumetone-, none of 90 etodac-, and 2 of 90 placebo treated patients; no mention of outcome or symptoms).
- Mabee CL, Mabee SW, Baker PB, Kirkpatrick RB, Levine EJ. Fulminant hepatic failure associated with etodolac use. Am J Gastroenterol 1995; 90: 660-2. [PubMed: 7717333](67 year old woman developed an acute hepatitis 4 months after starting etodolac for osteoarthritis [bilirubin 11.8 mg/dL, ALT 1554 U/L, Alk P 193 U/L, protime 21.4 sec], progressing to hepatic failure and death within 3 weeks of onset).
- Neustadt DH. Double blind evaluation of the long-term effects of etodolac versus ibuprofen in patients with rheumatoid arthritis. J Rheumatol Suppl 1997; 47: 17-22. [PubMed: 9035016](Randomized trial of 2 doses of etodolac vs ibuprofen in 1446 patients with rheumatoid arthritis treated for up to 3 years; similar efficacy; “Changes in hepatic and renal function were similar across treatment groups” and “rates… were low”, but higher dose of etodolac had higher rate of Alk P elevations; all resolved with stopping).
- Cunha PD, Lord RS, Johnson ST, Wilker PR, Aster RH, Bougie DW. Immune hemolytic anemia caused by sensitivity to a metabolite of etodolac, a nonsteroidal anti-inflammatory drug. Transfusion 2000; 40: 663-8. [PubMed: 10864985](41 year old woman developed jaundice after intermittent use of etodolac [total bilirubin 17.6 mg/dL, direct 6.8 mg/dL, AST 284 U/L, Alk P 125 U/L, protime 19.8 sec] with hemolytic anemia [hematocrit 18%, positive direct Coombs test], resolving within 2 months but with recurrence of hemolysis on restarting etodolac).
- Rubenstein JH, Laine L. Systematic review: the hepatotoxicity of non-steroidal anti-inflammatory drugs. Aliment Pharmacol Ther 2004; 20: 373-80. [PubMed: 15298630](NSAIDs are the most commonly used drugs in the U.S. and account for a large proportion of cases of hepatic injury, but the frequency is quite rare. Among 7 population based studies, hospitalization occurred in 22.4 per 100,000 patient-years [rate ratio 1.5], and ~1 death per 100,000 patient-years was due to liver injury; rate of injury did not increase with age or vary by gender; in case controlled studies, higher odds ratios were found with sulindac, indomethacin, piroxicam and diclofenac; analysis dealt largely with commonly used NSAIDs and did not mention etodolac).
- Rostom A, Goldkind L, Laine L. Nonsteroidal anti-inflammatory drugs and hepatic toxicity: a systematic review of randomized controlled trials in arthritis patients. Clin Gastroenterol Hepatol 2005; 3: 489-98. [PubMed: 15880319](Review of randomized clinical trials of NSAIDS for frequency of adverse events; ALT above 3 times ULN in 0.43% of ibuprofen, 0.43% naproxen, 0.42% celecoxib, 1.8% rofecoxib, 3.55% diclofenac and 0.29% of placebo recipients, rare liver-related serious adverse effects or deaths with any; dealt largely with commonly used NSAIDs and did not mention etodolac).
- Björnsson E, Jerlstad P, Bergqvist A, Olsson R. Fulminant drug-induced hepatic failure leading to death or liver transplantation in Sweden. Scand J Gastroenterol 2005; 40: 1095-101. [PubMed: 16165719](Survey of all cases of drug induced liver injury with fatal outcome from Swedish Adverse Drug Reporting system from 1966-2002: among 103 cases, none were attributed to etodolac).
- Griffin A. Case of the month. Chronic hepatitis. JAAPA 2006; 19: 70. [PubMed: 17124794](54 year old man taking etodolac for low back pain was found to have 3+ bilirubin in urine by dipstick, but serum ALT, AST and bilirubin were normal; the reaction because negative 10 days after stopping and was positive again 2 weeks after restarting, due to false-positive reaction of the diazo reagent).
- Lapeyre-Mestre M, de Castro AM, Bareille MP, Del Pozo JG, Requejo AA, Arias LM, et al. Non-steroidal anti-inflammatory drug-related hepatic damage in France and Spain: analysis from national spontaneous reporting systems. Fundam Clin Pharmacol 2006; 20: 391-5. [PubMed: 16867024](Analysis of reports of liver injury from NSAIDs from France and Spain from 1982-2001; etodolac is not listed in tables of adverse event reports from NSAIDs).
- Arellano FM, Yood MU, Wentworth CE, Oliveria SA, Rivero E, Verma A, et al. Use of cyclo-oxygenase 2 inhibitors(COX-2) and prescription non-steroidal anti-inflammatory drugs (NSAIDS) in UK and USA populations Implications for COX-2 cardiovascular profile. Pharmacoepidemiol Drug Saf 2006; 15 :861-72. [PubMed: 17086563](Survey of NSAID use in UK and USA indicates ibuprofen, naproxen and diclofenac are the most commonly used; etodolac was not among the top 10 agents used).
- Jensen M, Engert A, Weissinger F, Knauf W, Kimby E, Poynton C, et al. Phase I study of a novel pro-apoptotic drug R-etodolac in patients with B-cell chronic lymphocytic leukemia. Invest New Drugs 2008; 26: 139-49. [PubMed: 18094935](Use of high doses of a R-enanomer of etodolac [1.2 to 4.8 g/day] was associated with decrease in lymphocyte counts in patients with chronic lymphocytic leukemia; the activity was separate from Cox inhibition and not shared by other NSAIDs; in this phase I trial, ALT elevations occurred in 11 of 45 patients [26%], were unrelated to dose, and led to drug withdrawals in 3 [7%]; no mention of hepatitis).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J; Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008; 135: 1924-34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected from 2004 to 2008, NSAIDs were implicated as a sole agent in 8 cases [4 diclofenac, 2 celecoxib, 1 meloxicam and 1 oxaprozin] and as one of several agents in 3 cases [1 diclofenac, 1 celecoxib, 1 ibuprofen]; no cases were attributed to etodolac).
- Reuben A, Koch DG, Lee WM; Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology 2010; 52: 2065-76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, of which 7 were due to NSAIDs, including 4 attributed to bromfenac, 2 to diclofenac and 1 to etodolac).
- Bessone F. Non-steroidal anti-inflammatory drugs: What is the actual risk of liver damage? World J Gastroenterol 2010; 16: 5651-61. [PMC free article: PMC2997980] [PubMed: 21128314](Review of estimated frequency of drug induced liver injury due to NSAIDs from large published epidemiological studies; mentions that etodolac has been associated with various hepatic reactions).
- Mehta P, Lukacs M, Abraham SM. Normal in the blood, abnormal in the urine. QJM 2012; 105: 1001-2. [PubMed: 21880696](67 year old woman with rheumatoid arthritis on etodolac had persistent positive urine dipstick reaction for bilirubin despite normal serum bilirubin and liver tests; false positive reaction was due to etodolac).
- Sampaziotis F, Brais RJ, Griffiths WJ. A case of acute liver failure due to etodolac. Br J Clin Pharmacol 2013; 75: 1156-7. [PMC free article: PMC3612737] [PubMed: 22943552](73 year old woman developed jaundice 6 months after starting etodolac [bilirubin 30.7 mg/dL, ALT 1400 U/L, Alk P 274 U/L, protime 16.7 seconds], developing hepatic encephalopathy, but then recoverying spontaneously within 3 months of stopping).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 2013; 144: 1419-25 . [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, including 6 attributed to diclofenac [ranking 2nd], but none due to etodolac).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol 2014; 13: 231-9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, the most common class of implicated agents being NSAIDS [n=62, 32%], but specific agents were nimesulide [n=53], piroxicam [5], diclofenac [2], gold salts [1], and naproxen [1]; etodolac was not listed]).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 28 were attributed to NSAIDs, including 2 to etodolac [Schmeltzer 2016]).
- Schmeltzer PA, Kosinski AS, Kleiner DE, Hoofnagle JH, Stolz A, Fontana RJ, Russo MW; Drug-Induced Liver Injury Network (DILIN). Liver injury from nonsteroidal anti-inflammatory drugs in the United States. Liver Int 2016; 36: 603-9. [PMC free article: PMC5035108] [PubMed: 26601797](Among 1221 cases of drug induced liver injury enrolled in a prospective, US database between 2004 and 2014, 30 cases [2.5%] were attributed to NSAIDs, including 2 due to etodolac [Case 1], both of which presented with jaundice 5 and 7 months after starting [bilirubin 3.8 and 4.0 mg/dL, ALT 322 and 661 U/L, Alk P 128 and 341 U/L, INR 1.0 and 1.0], both recovering rapidly upon stopping without residual injury).
- Taneja S, Kumar P, Rathi S, Duseja A, Singh V, Dhiman RK, Chawla YK. Acute liver failure due to etodolac, a selective cycloxygenase- 2 (COX -2) inhibitor non-steroidal anti-inflammatory drug established by RUCAM-based causality assessment. Ann Hepatol 2017; 16: 818-21. PubMed Citation. [PubMed: 28809737](Two women, ages 27 and 80 years, developed nausea and vomiting within 48 hours of starting a fixed combination of etodolac [400 mg] and acetminophen [500 mg] twice daily followed rapidly by jaundice and confusion [bilirubin 4.3 and 4.4 mg/dL, ALT 6060 and 6896 U/L, Alk P 229 and 78 U/L , INR 6.7 and 4.0] with hyperammonemia and lactic acidosis, one patient dying within 2 days and the other recovering rapidly, a pattern indicative of acute hepatic necrosis).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Effect of a nonsteroidal antiinflammatory drug on synovial fluid in osteoarthritis.[J Rheumatol. 1996]Effect of a nonsteroidal antiinflammatory drug on synovial fluid in osteoarthritis.Schumacher HR Jr, Meng Z, Sieck M, Zonay L, Clayburne G, Baker JF, Park J, Baker DG. J Rheumatol. 1996 Oct; 23(10):1774-7.
- Review Nabumetone.[LiverTox: Clinical and Researc...]Review Nabumetone.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Meloxicam.[LiverTox: Clinical and Researc...]Review Meloxicam.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Tissue selective inhibition of prostaglandin biosynthesis by etodolac.[J Rheumatol Suppl. 1997]Review Tissue selective inhibition of prostaglandin biosynthesis by etodolac.Dvornik DM. J Rheumatol Suppl. 1997 Feb; 47:40-7.
- Review Tolmetin.[LiverTox: Clinical and Researc...]Review Tolmetin.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Etodolac - LiverToxEtodolac - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...