NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Erythromycin is an oral macrolide antibiotic that has been in common use since the 1950s. Erythromycin has been linked to rare instances of acute liver injury that are usually self-limited, but can result in severe injury and death.
Background
Erythromycin (e rith" roe mye' sin) is a semisynthetic macrolide antibiotic used widely for many decades to treat mild-to-moderate bacterial infections caused by sensitive agents. Erythromycin is bacteriostatic against many gram positive bacteria including many strains of streptococci, staphylococci, clostridia, corynebacteria, listeria, haemophilus sp., moxicella, and Neisseria meningitidis. Modifications of erythromycin have been developed with a wider range of activity and less likelihood for resistance (azithromycin, clarithromycin, telithromycin). The macrolide antibiotics are believed to act by inhibiting protein synthesis of bacteria by binding to the 50S ribosomal element. Resistance occurs by several mechanisms. Erythromycin was approved for use in the United States in 1967, and currently more than 1.5 million prescriptions are filled yearly. Specific indications include mild-to-moderate upper or lower respiratory tract infections, urethritis, pelvic inflammatory disease, urogenital chlamydia infections, Legionnaires’ disease, and intestinal amebiasis. Erythromycin is commonly used as a second-line agent when penicillin, tetracyclines or metronidazole are contraindicated. Erythromycin is available in multiple formulations (estolate, ethylsuccinate, lactobionate, stearate) in many generic and brand name forms in capsules or tablets of 250 or 500 mg including enteric coated and delayed release forms. The usual adult dose is 1 to 4 grams daily in divided doses for 7 to 21 days, depending upon the type, nature and severity of the infection. Gastrointestinal side effects (abdominal pain, nausea, and diarrhea) are common, but are rarely severe.
Hepatotoxicity
Erythromycin therapy is associated with a low rate (1% to 2%) of serum enzyme elevations during therapy. The enzyme elevations are typically asymptomatic and transient, and may occur no more frequently than with placebo or other comparator anitbiotic treatments.
Clinically apparent liver injury from erythromycin is rare, but because of the frequency of its use, erythromycin has been one of the most common causes of drug induced liver injury at least in previous years. Initially, liver injury was thought to be more common with, or perhaps limited to, erythromycin estolate. However, instances of jaundice and liver damage have been reported with virtually all formulations of erythromycin, and cross sensitivity to injury is common, although not universal. The hepatotoxicity of erythromycin resembles that described in other macrolide antibiotics and is typically a mild and self-limiting cholestatic hepatitis. The latency period between starting erythromycin and onset of liver injury is short, typically 1 to 3 weeks and is shorter (<1 week) with reexposure. Symptoms may include right upper quadrant pain and jaundice, clinical features that might suggest cholecystitis. Eosinophilia and fever are common, but not universal; rash is reported less commonly. The pattern of enzyme elevations is often mixed or variable, but the disease is usually cholestatic and symptoms of pruritus may be prominent. The liver injury is usually mild and self-limited with recovery in 4 to 8 weeks. However, instances of prolonged jaundice and cholestasis with paucity of bile ducts due to erythromycin have been reported. Furthermore, cases of abupt onset of liver injury after a short latency (<1 week) and a hepatocellular pattern of liver enzyme elevations have been reported, particularly with repeat exposure, and some of these cases have led to acute liver failure and death or need for liver transplantation. Rapid recurrence occurs with rechallenge even within 24 hours of a single dose.
A separate syndrome associated with erythromycin use is acute right upper quadrant pain without jaundice that arises within a day or two of starting therapy. Serum enzymes may be mildly elevated, usually in a hepatocellular pattern and with rapid recovery once erythromycin is stopped.
Likelihood score: A (well known cause of clinically apparent liver injury).
Mechanism of Injury
The cause of the idiosyncratic hepatitis following erythromycin therapy is not known. Allergic manifestations (rash, fever and eosinophilia) are typical, so that hypersensitivity is assumed to be the cause. Other features suggesting hypersensitivity are that rechallenge typically leads to recurrence with a shortened latency period, and patients may have a history of previous exposure to erythromycins without adverse effects.
Outcome and Management
Most cases of erythromycin induced liver disease are mild and self-limiting; however, very rare instances of severe acute hepatic injury leading to acute liver failure and need for transplantation or death have been described. Furthermore, isolated examples of prolonged cholestasis with vanishing bile duct syndrome have been reported. Patients with erythromycin induced hepatic injury should be cautioned to avoid further exposure and it is prudent to avoid use of other macrolides in patients with clinically apparent liver injury due to erythromycin.
Drug Class: Antiinfective Agents, Macrolide Antibiotics
CASE REPORTS
Case 1. Abdominal pain and jaundice after erythromycin therapy.
(Modified from: Reed C, Ritchie F. Toxic jaundice due to propionyl erythromycin ester lauryl sulfate (“Ilosone”). Med J Aust 1962; 49: 810-2. PubMed Citation
A 33 year old man with a superficial cellulitis on his hand was treated with erythromycin estolate in January 1961 and again in March. Within 10 days of starting the second course, he developed right upper quadrant abdominal pain followed by dark urine and jaundice. With stopping the drug, he improved rapidly, the pain and jaundice clearing within days (Table) and ALT levels falling to normal over the next two months. In October of the same year, he restarted erythromycin for a recurrence of the cellulitis and developed severe abdominal pain within the next day, followed shortly afterwards by jaundice and dark urine. Therapy was stopped after 2 days when he was found to be jaundiced. Again, recovery was rapid. During both episodes, there was no rash, fever, arthralgias or eosinophilia. Testing for autoantibodies was not mentioned in the report, which predated tests for hepatitis A, B and C.
Key Points
| Medication: | Erythromycin estolate (250 mg four times daily) |
|---|---|
| Pattern: | Hepatocellular (elevations in aminotransferases only) |
| Severity: | 2+ (jaundiced, but not hospitalized) |
| Latency: | 10 days (first episode), 1 day (rechallenge) |
| Recovery: | Complete within 8 weeks |
| Other medications: | None |
Laboratory Values
| Time After Starting | Time After Stopping | ALT (U/L) | Alk P* (KA U/L) | Bilirubin (mg/dL) | Other |
|---|---|---|---|---|---|
| Abdominal pain and dark urine 10 days after starting erythromycin | |||||
| 12 days | 0 | 3000 | 9.5 | 4.7 | |
| 1 week | 2 days | 1400 | 9.0 | 0.7 | |
| 3 weeks | 9 days | 350 | 7.0 | 0.6 | |
| 4 weeks | 16 days | 260 | 5.0 | 0.4 | |
| 6 weeks | 4 weeks | 140 | |||
| 7 weeks | 5 weeks | 155 | |||
| 8 weeks | 6 weeks | 105 | |||
| 10 weeks | 8 weeks | 95 | |||
| Abdominal pain and dark urine within 1 day of restarting erythromycin | |||||
| 2 days | 0 | 3200 | 10.5 | 7.5 | |
| 7 days | 5 days | 1400 | 1.0 | ||
| 13 days | 11 days | 400 | 1.2 | ||
| 15 days | 13 days | 170 | 0.5 | ||
| Normal Values | <35 | <13 | <1.2 | ||
* KA U=King Armstrong Units.
Comment
A very convincing example of erythromycin hepatotoxicity, with symptoms arising 10 days after a second exposure to the medication and then within 24 hours of the inadvertent rechallenge 6 months later. Abdominal pain is a common presenting symptom in macrolide associated acute hepatic injury. The two episodes were mirror images in pattern and height of enzyme and bilirubin elevations. The course suggests an immunoallergic mechanism of injury, even though rash, fever and eosinophilia were absent. The symptoms and high ALT levels are typical of hepatocellular injury; but, erythromycin is classically believed to lead to cholestatic hepatitis; this example demonstrating that serum enzymes in hyperacute cases are more typically hepatocellular in pattern.
Case 2. Asymptomatic liver injury after one day of erythromycin.
(Modified from: Alcalay J, Halevy S, Theodor E, Sandbank M. Asymptomatic liver injury due to erythromycin stearate. Drug Intell Clin Pharm 1986; 20: 601-2. PubMed Citation)
A 73 year old woman was started on erythromycin stearate just before being admitted for evaluation of facial pyoderma, but was then found to have abnormal liver tests with elevations in both alkaline phosphatase and ALT (Table). Serum enzyme levels continued to climb and erythromycin was stopped, whereupon levels fell into the normal range. During the whole period, she was asymptomatic and specifically denied fatigue, nausea, abdominal pain or dark urine. Serum bilirubin levels remained normal.
Key Points
| Medication: | Erythromycin stearate (500 mg four times daily) |
|---|---|
| Pattern: | Cholestatic (R=1.8) |
| Severity: | 1+ (no jaundice) |
| Latency: | 2 days |
| Recovery: | Complete within 2 weeks |
| Other medications: | None mentioned |
Laboratory Values
| Time After Starting | Time After Stopping | ALT* (U/L) | Alk P* (U/L) | Bilirubin* (mg/dL) | Other |
|---|---|---|---|---|---|
| Oral erythromycin stearate started for facial pyoderma | |||||
| 2 days | 125 | 178 | Normal | Asymptomatic | |
| 4 days | 0 | 210 | 240 | Erythromycin stopped | |
| 6 days | 2 days | 140 | 230 | ||
| 9 days | 5 days | 115 | 175 | ||
| 11 days | 7 days | 70 | 140 | ||
| 14 days | 10 days | 60 | 120 | ||
| 15 days | 11 days | 35 | 110 | ||
| Normal Values | <40 | <95 | <1.2 | ||
* Some values estimated from Figure 1. Bilirubin converted from µmol (1.0 mg% = 17.1 µmol).
Comment
This case was unusual in several regards. First, the latency period was short, particularly for a patient who had not received erythromycin in the past. Second, the enzyme pattern was cholestatic, but there was no jaundice or symptoms. Erythromycin typically causes a syndrome of sudden onset of right upper quadrant pain, fever and jaundice. Jaundice from erythromycin is usually mild, but can occasionally be severe and prolonged. This is one of the few cases of acute erythromycin induced liver disease published in the last 25 years. This form of drug induced liver injury appears to be less common with the non-estolate forms of erythromycin, and there is a general lack of interest in publishing cases of hepatotoxicity due to drugs well known to be associated with liver injury.
Case 3. Acute hepatitis from erythromycin.
[Modified from a case in the database of the Drug-Induced Liver Injury Network.]
A 73 year old woman developed right flank pain and fever 2 to 3 days after starting erythromycin ethylsuccinate (400 mg four times daily) for symptoms of cystitis. She stopped erythromycin promptly, but developed increasing fatigue, jaundice and pruritus over the next few days and presented to her physician 4 days later. She did not drink alcohol and had no history of liver disease or risk factors for viral hepatitis. Her other medications included atorvastatin and aspirin which she had taken for many years. She had been treated with erythromycin six months previously, but without adverse effects. On admission, her serum bilirubin was 8.6 mg/dL, ALT 1884 U/L, AST 1574 U/L, alkaline phosphatase 492 U/L, serum albumin 3.2 g/dL and INR 0.85 (Table). Tests for hepatitis A, B and C were negative. Antinuclear antibody was negative, while smooth muscle antibodies were weakly positive (1:80). Abdominal ultrasound, computerized tomography and magnetic resonance cholangiopancreatography demonstrated a single large gallstone, but no evidence of biliary obstruction. She was monitored on no specific therapy and liver test abnormalities slowly improved. Symptoms resolved within two weeks, serum bilirubin fell to normal within one month and all liver tests were normal when she was seen in follow up 3 months later. Atorvastatin, which had been stopped with the onset of jaundice, was restarted without recurrence of liver injury.
Key Points
| Medication: | Erythromycin ethylsuccinate (400 mg four times daily) for two days |
| Pattern: | Hepatocellular (R=13.5) |
|---|---|
| Severity: | 3+ (jaundice and hospitalization) |
| Latency: | 2 days to symptoms, 4 days to jaundice |
| Recovery: | Complete within 3 months |
| Other medications: | Atorvastatin, aspirin (given chronically) |
Laboratory Values
| Time After Starting | Time After Stopping | ALT (U/L) | Alk P (U/L) | Bilirubin (mg/dL) | Other |
|---|---|---|---|---|---|
| Oral erythromycin ethylsuccinate taken for 2 days for urinary tract infection | |||||
| 6 days | 4 days | 1884 | 492 | 8.6 | Admission |
| 10 days | 8 days | 2058 | 626 | 7.3 | CT scan |
| 2 weeks | 12 days | 2011 | 596 | 5.4 | |
| 3 weeks | 3 weeks | 1308 | 408 | 3.1 | MRCP |
| 4 weeks | 4 weeks | 670 | 269 | 1.9 | |
| 5 weeks | 5 weeks | 263 | 191 | 1.2 | |
| 6 weeks | 6 weeks | 80 | 144 | 0.9 | |
| 3 months | 3 months | 32 | 78 | 0.4 | Atorvastatin restarted |
| 10 months | 10 months | 22 | 63 | 0.7 | |
| Normal Values | <45 | <125 | <1.2 | ||
Comment
The appearance of liver injury and jaundice within a week of starting erythromycin is typical of the acute onset of injury with rechallenge. This patient had taken erythromycin in the past without difficulty, but the previous exposure may have resulted in a sensitization that became clinically manifest with reexposure. The serum enzyme elevations were hepatocellular with marked increases in serum ALT and AST (40-50 times normal). However, the alkaline phosphatase was also elevated (3- to 5-fold) and she complained of pruritus during the acute episode, suggesting a cholestatic element to the injury. Erythromycin hepatotoxicity appears to be more common in older individuals. The acute, abrupt hepatocellular injury with macrolide antibiotics can be severe and lead to acute liver failure. The prompt discontinuation of the medication may have been fortunate.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Erythromycin — Generic, ERYC®
DRUG CLASS
Antiinfective Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Erythromycin | 114-07-8 | C37-H67-N-O13 |
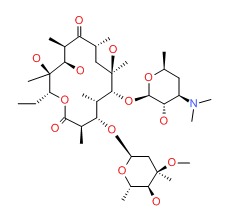 |
ANNOTATED BIBLIOGRAPHY
References updated: 10 August 2017
- Zimmerman HJ. Erythromycins. In, Zimmerman HJ. Hepatotoxicity: The adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 1999, pp. 594-5.(Expert review of erythromycin and liver injury published in 1999; erythromycin has been linked to many instances of cholestatic hepatitis typically presenting after 1-3 weeks of therapy [initial exposure] but sometimes within a week of starting treatment [repeat exposure] with abdominal pain [75%], jaundice [75%], fever [50%], eosinophilia [60%], and pruritus [25%], most cases being self-limiting and benign).
- Moseley RH. Macrolide antibiotics. Hepatotoxicity of antimicrobials and antifungal agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced Liver Disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 466-7.(Expert review of macrolide antibiotic-induced liver injury mentions that liver injury from erythromycin is typically cholestatic and usually self-limited, occurring in 3-4 persons per 100,000 users; now rarely reported).
- MacDougall C, Chambers HF. Macrolides and ketolides. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1529-34.(Textbook of pharmacology and therapeutics).
- Johnson DF Jr, Hall WH. Allergic hepatitis caused by propionyl erythromycin ester of lauryl sulfate. N Engl J Med 1961; 265: 1200-2. [PubMed: 14452017](Onset of fever and right upper quadrant pain after 12 days of erythromycin estolate [bilirubin 1.8 mg/dL, AST 117 U/L]; re-exposure caused immediate recurrence with pain [bilirubin 3.0 mg/dL, AST 320 U/L, Alk P 5 times ULN] but full subsequent recovery).
- Kohlstaedt KG. Propionyl erythromycin ester lauryl sulfate and jaundice. JAMA 1961; 178: 89-90.(Letter describing 7 cases reported to Eli Lilly of jaundice, AST elevations [100-300 U/L], eosinophilia, and elevated Alk P levels after erythromycin use; 4 had positive rechallenge with pain and jaundice; after 3 years of availability, a total of 33 cases of liver injury were reported after an estimated 15 million courses: ~2 per million).
- Dittler EL. Upper abdominal pain and intrahepatic cholestasis as manifestations of sensitivity to Ilosone. Am J Gastroenterol 1962; 38: 691-2. [PubMed: 14028076](50 year old woman had three episodes of right upper quadrant pain, fever, Alk P and ALT elevations after single erythromycin estolate ingestion: no jaundice, but few tablets taken).
- Gilbert FI Jr. Cholestatic hepatitis caused by esters of erythromycin and oleandomycin. JAMA 1962; 182: 1048-50. [PubMed: 13947810](46 year old man developed severe right upper quadrant pain and fever 12 hours after taking 2 doses of erythromycin estolate [bilirubin 2.4 mg/dL, AST 350 U/L, Alk P 4.7 BU], but subsequently had no reaction to one challenge dose of erythromycin stearate).
- Havens WP Jr. Cholestatic jaundice in patients treated with erythromycin estolate. JAMA 1962; 180: 30-2. [PubMed: 13905478](Report of 4 patients [ages 19-59 years, 3 men and 1 woman] with erythromycin hepatitis, latency to onset of 1-3 weeks presenting with jaundice, itching, fever and abdominal pain, 3 with eosinophilia; mixed, cholestatic and hepatocellular patterns of enzyme elevations, 3 treated with prednisone, 1 had severe and prolonged course beyond 6 months).
- Masel MA. Erythromycin hepato-sensitivity: a preliminary report of two cases. Med J Aust 1962; 49: 560-2. [PubMed: 14470759](Two cases: 12 and 17 year old boys developed acute liver injury 11 and 17 days after starting erythromycin therapy with fever, rash, abdominal pain, jaundice [bilirubin 6.5 and 5.4 mg/dL] and eosinophilia with rapid recovery).
- Reed C, Ritchie F. Toxic jaundice due to propionyl erythromycin ester lauryl sulfate (“Ilosone”). Med J Aust 1962; 49: 810-2. [PubMed: 14037477](33 year old man developed abdominal pain 10 days after starting erythromycin [2nd exposure] with subsequent jaundice [bilirubin 4.7 mg/dL, ALT 3000 U/L, Alk P normal], and an immediate recurrence after a single dose 6 months later; rapid recovery after both episodes: Case 1).
- Riley WA. Hepatitis following administration of Ilosome. Case report. N C Med J 1962; 23: 362. [PubMed: 14038696](23 year old man developed fatigue after 5 days of oral erythromycin, with subsequent jaundice [bilirubin 9.6 mg/dL], resolving within a month of stopping; no serum enzyme results; had a positive rechallenge).
- Robinson MM. Demonstration by "challenge" of hepatic dysfunction associated with propionyl erythromycin ester lauryl sulfate. Antibiot Chemother 1962; 12: 147-51. [PubMed: 14492925](Follow up study, triacetyloleandomycin led to raised ALT in 11 of 59 patients treated for more than 14 days; rechallenge in 3 led to increases in ALT to 340, 81 and 274 U/L with eosinophilia [6-11%] but no jaundice).
- Robinson MM. Hepatic dysfunction associated with triacetyloleandomycin and propionyl erythromycin ester lauryl sulfate. Am J Med Sci 1962; 243: 502-10. [PubMed: 14492926](Prospective study of 80 patients receiving erythromycin estolate, 10 developed raised ALT [67-300 U/L] within 14-21 days, 2 had jaundice [2.2 and 3.5 mg/dL], all resolved with stopping but 3/3 had ALT rise [180-2060 U/L] and eosinophilia within 24 hours of rechallenge).
- Robinson MM. Hepatic dysfunction associated with triacetyloleandomycin demonstrated by challenge. Am J Med Sci 1962; 244: 221-4. [PubMed: 14492927](Follow up study, triacetyloleandomycin led to raised ALT in 11 of 59 patients treated for more than 14 days; rechallenge in 3 led to increases in ALT to 340, 81 and 274 U/L with eosinophilia [6-11%] but no jaundice).
- Brown AR. Two cases of untoward reaction after "Ilosone". Br Med J 1963; 2: 913-5. [PMC free article: PMC1873009] [PubMed: 14067683](2 case reports from Australia: 25 year old man developed fever, severe right upper quadrant pain and jaundice that persisted for 3 months after 2nd day of a second 3-day course of erythromycin estolate; 51 year old woman developed acute right upper quadrant pain after single dose of erythromycin [bilirubin normal, AST 95 U/L, Alk P 22 KA U/L], resolving within 3 weeks).
- Farmer CD, Hoffman HN 2nd, Shorter RG, Thurber DL, Bartholomew LG. Intrahepatic cholestasis associated with the ingestion of erythromycin estolate (Ilosone). Gastroenterology 1963; 45: 158-60. [PubMed: 14054883](6 cases of erythromycin hepatotoxicity from Mayo Clinic with onset after 6-21 days, usually presenting with abdominal pain and fever but mild jaundice, rapid recovery; 2 patients had previous exposures, 1 had positive rechallenge).
- Ticktin HE, Robinson MM. Effects of some antimicrobial agents on the liver. Ann NY Acad Sci 1963; 104: 1080-92. (Not in PubMed).
- Fischer HW, Hoak JC. Mimicry of acute cholecystitis by erythromycin estolate reactions. Report of 2 cases. Am J Med Sci 1964; 247: 283-5. [PubMed: 14130320](Two men (ages 42 and 53 years] developed acute right upper quadrant pain after 4 and 2 days of oral erythromycin with minimal ALT increase and no jaundice or gallstones, 1 had rapid recurrence with rechallenge).
- Fukayak TG. [Case of hypersensitive hepatitis due to propionyl erythromycin lauryl sulfate] Naika 1964; 14: 741-4. Japanese. [PubMed: 14202924]
- Nilsson S. [Liver disorders due to treatment with propionyl-erythromycin-lauryl sulfate (Ilosone)] Nord Med 1964; 72: 1417-9. Swedish. [PubMed: 14227583]
- Herskovic T, Solis J, Villasana Z, Jinich H. Acute abdomen associated with the ingestion of erythromycin estolate. Am J Gastoenterol 1965; 43: 138-142.
- McKenzie I, Doyle A. Two cases of jaundice following "Ilosone". Med J Aust 1966; 1: 349-51. [PubMed: 5906690](Two cases: 40 and 21 year old men developed jaundice after 4 and 8 days of therapy with erythromycin estolate [bilirubin 6 and 12 mg/L, AST 80 and 87 U/L, Alk P 47 and 15 U/L], with slow recovery [1 and 6 months]).
- Petricević I, Kosutić Z, Schönwald S, Rulnjević J. [Hepatitis caused by erythromycin] Lijec Vjesn 1968; 90: 1051-9. Croatian. [PubMed: 5195777]
- Braun P. Hepatotoxicity of erythromycin. J Infect Dis 1969; 119: 300-6. [PubMed: 4888905](Thorough review of literature on hepatotoxicity of macrolides up to 1969: by then, there were 45 published cases of liver injury from erythromycin estolate [none with stearate] presenting within 1-3 weeks with jaundice [67%], abdominal pain, nausea and fever [~50%] as well as eosinophilia [62%], elevations in ALT [100%: average 338 U/L] and Alk P [51%]; 13 rechallenged, invariably followed by rapid recurrence, often severe])
- Kosenow W, Stollenwerk F. [Jaundice following erythromycin-estolate therapy] Dtsch Med Wochenschr 1971; 96: 1836 passim. German. [PubMed: 5121113]
- Oliver LE, Iser JH, Stening GF, Smallwood RA. Abdominal pain and erythromycin estolate. Lancet 1972; 2: 980. [PubMed: 4116869](Letter describing 5 cases of severe right upper quadrant pain within 4-36 hours of taking erythromycin estolate, 2 with jaundice).
- The erythromycins. A further report from the Australian Drug Evaluation Committee. Med J Aust 1973; 2: 192-3. [PubMed: 4741351](As of May 1973, 113 cases of jaundice due to erythromycin estolate had been reported to Australian registry; all ages affected, mostly within 14 days, but some >21 days of starting, usually lasting < 28 days, no deaths).
- [Erythromycin estolate and liver toxicity] Ugeskr Laeger 1974; 136: 2093-4. Danish. [PubMed: 4409491]
- Buchanec J, Krajnák V. [Liver damage during erythromycin therapy in 3 children] Cesk Pediatr 1974; 29: 76-8. Slovak. [PubMed: 4452168]
- Tolman KG, Sannella JJ, Freston JW. Chemical structure of erythromycin and hepatotoxicity. Ann Intern Med 1974; 81: 58-60. [PubMed: 4834945](Patient with erythromycin estolate hepatotoxicity was rechallenged with various erythromycins: rapid recurrence after estolate [temp 39.9° C, bilirubin 2.3 mg/dL, ALT 608 U/L], within 5 days and after propionate [temp 38.4° C, bilirubin 1.7 mg/dL, ALT 326 U/L] but no recurrence after stearate, ethylsuccinate or erythromycin-base rechallenges).
- Lunzer MR, Huang SN, Ward KM, Sherlock S. Jaundice due to erythromycin estolate. Gastroenterology 1975; 68(5 Pt 1): 1284-91. [PubMed: 1126604](43 year old man developed right upper quadrant pain 24 hours after starting a second course of erythromycin estolate followed by jaundice; rechallenged and redeveloped pain [AST rising from 12 to 302 U/L, Alk P 11 to 22 KA U, bilirubin 0.5 to 1.3 mg/dL]: biopsy before and after rechallenge showed inflammation and endoplasmic reticulum changes by electron microscopy without necrosis).
- Pessayre D, Marie C, Benhamou JP. [Hepatitis due to erythromycin propionate (author's transl)] Arch Fr Mal App Dig 1976; 65: 405-8. French. [PubMed: 1008656](Cholestatic jaundice with right upper quadrant pain and eosinophilia, resolving with stopping erythromycin propionate and recurring with rechallenge).
- Cacace LG, Schweigert BF, Gildon AM. Erythromycin estolate induced hepatotoxicity: report of a case and review of the literature. Drug Intell Clin Pharm 1977; 11: 22-25. Not in PubMed.
- Cooksley WG, Powell LW. Erythromycin jaundice: diagnosis by an in vitro challenge test. Aust N Z J Med 1977; 7: 291-3. [PubMed: 269690](53 year old woman developed fever within 24 hours and jaundice within 4 days of taking 2 capsules of erythromycin estolate [bilirubin 17.1 mg/dL, AST 69 U/L, Alk P 114 U/L] and recovery in ~3 weeks; lymphocyte transformation tests was positive 2 years later to estolate but not stearate or erythromycin base).
- McCormack WM, George H, Donner A, Kodgis LF, Alpert S, Lowe EW, Kass EH. Hepatotoxicity of erythromycin estolate during pregnancy. Antimicrob Agents Chemother 1977; 12: 630-5. [PMC free article: PMC429989] [PubMed: 21610](Prospective study comparing safety and efficacy of erythromycin estolate, clindamycin and placebo for 6 weeks in 539 pregnant women with genital mycoplasma infections; AST elevations occurred in 10% with erythromycin [44-130 U/L], vs 2.4% with clindamycin [42-44 U/L] and 1.8% with placebo [42-88 U/L]; lower rates subsequently with stearate [3.0%]).
- Lloyd-Still JD, Sherman JO, Boggs J, Demers LM. Erythromycin estolate hepatotoxicity. Am J Dis Child 1978; 132: 320. [PubMed: 629252](7 year old boy developed fever and severe right upper quadrant pain within 24 hours of re-exposure to erythromycin estolate [bilirubin 4.8 mg/dL, AST 150 U/L, Alk P 90 U/L, bile acids >100 fold increased]).
- Rodríguez Cuartero A, Rodríguez Cuartero F, Alonso Fernández J, Castillo Higueras PL. [Acute hepatitis caused by erythromycin] Rev Esp Enferm Apar Dig 1978; 54: 533-6. Spanish. [PubMed: 746229](29 year old pregnant woman had onset of abdominal pain and nausea within days of starting erythromycin, followed by miscarriage at 10 days and jaundice at two weeks [bilirubin 7.2 mg/dL, ALT 214 U/L, Alk P not done]; resolving within 1 month).
- Gafter U, Mandel EM, Weiss S, Djaldetti M. Erythromycin estolate-induced hepatitis. Ultrastructural study of liver. N Y State J Med 1979; 79: 87-9. [PubMed: 282477](28 year old woman developed abdominal pain, fever and jaundice after 2 weeks of erythromycin estolate [12% eosinophils, bilirubin 3.7 mg/dL, ALT 175 U/L, Alk P 2 times ULN], recurring within 1 day of rechallenge with one pill [bilirubin 2.8 mg/dL], biopsy showing mild changes of cholestasis by electron microscopy with dilated canaliculi).
- Krowchuk D, Seashore JH. Complete biliary obstruction due to erythromycin estolate administration in an infant. Pediatrics 1979; 64: 956-8. [PubMed: 514726](6 week old infant developed jaundice and acholic stools starting 6 days after course of erythromycin estolate which resolved after passing of "green plug" in stool).
- Pessayre D, Benhamou JP. Hepatotoxicity of erythromycin derivatives. Br Med J 1979; 1: 1357. [PMC free article: PMC1599613] [PubMed: 445081](Letter in response to review that suggested that only the estolate form of erythromycin causes liver injury: argues that this is not correct).
- Viteri AL, Greene JF Jr, Dyck WP. Erythromycin ethylsuccinate-induced cholestasis. Gastroenterology 1979; 76 (5 Pt 1): 1007-8. [PubMed: 437404](Initial report of liver toxicity of ethylsuccinate, 52 year old woman developed abdominal pain 1 day after starting erythomycin ethylsuccinate, followed by fever and jaundice [AST 54 U/L, Alk P 178 U/L, bilirubin 4.8 mg/dL, GGT 197 U/L] resolving 5 weeks later; history was later obtained of similar episode with previous exposure to erythromycin).
- Zafrani ES, Ishak KG, Rudzki C. Cholestatic and hepatocellular injury associated with erythromycin esters: report of nine cases. Dig Dis Sci 1979; 24: 385-96. [PubMed: 456225](Review of histology of 9 cases of erythromycin liver injury from Armed Forces Institute of Pathology files; mostly cholestatic or mixed enzyme pattern, all self-limited, [bilirubin 2.1-12 mg/dL, ALT 128-560 U/L, Alk P 2-12 times ULN]; liver histology showed cholestasis and hepatocellular injury).
- Sullivan D, Csuka ME, Blanchard B. Erythromycin ethylsuccinate hepatotoxicity. JAMA 1980; 243: 1074. [PubMed: 6965509](45 year old woman developed cholecystitis-like clinical picture with fever and eosinophilia 9 days after starting erythromycin ethylsuccinate [ALT rising to 613 U/L, Alk P 190 U/L but no jaundice], resolving rapidly after stopping).
- Bachman BA, Boyd WP Jr, Brady PG. Erythromycin ethylsuccinate-induced cholestasis. Am J Gastroenterol 1982; 77: 397-400. [PubMed: 6979924](49 year old woman with recurrent episodes of right upper quadrant pain and cholestatic jaundice caused by intermittent use of erythromycin ethylsuccinate, reproduced within 1 day of deliberate rechallenge [bilirubin 2.2 mg/dL, ALT 243 U/L, Alk P 438 U/L]).
- Cocchi P, Silenzi M, Salvi G, Calabri G, Tamburini M, Alvisi P. [Hepatotoxic syndrome caused by erythromycin ethyl succinate] Minerva Pediatr 1982; 34: 68-9. Italian. [PubMed: 6978458]
- Funck-Brentano C, Danan G, Pessayre D, Benhamou JP. [Hepatitis due to erythromycin ethylsuccinate] Gastroenterol Clin Biol 1982; 6: 1044-5. French. [PubMed: 6984402](48 year old man developed fatigue after 9 and jaundice after 11 days of oral erythromycin ethylsuccinate [bilirubin 12.9 mg/dL, ALT 360 U/L, Alk P 2.5 times ULN] and prolonged jaundice [2 months] with slow recovery [drug not stopped promptly]).
- Keeffe EB, Reis TC, Berland JE. Hepatotoxicity to both erythromycin estolate and erythromycin ethylsuccinate. Dig Dis Sci 1982; 27: 701-4. [PubMed: 6980110](Two cases of erythromycin estolate liver injury with rapid recurrence on exposure to ethylsuccinate 13-15 years later; cholecystitis-like syndrome with abdominal pain and fever [peak AST 63 and 500 U/L, Alk P 99 and 159 U/L).
- Ponsot P, Théodore C, Larrey D, Breil P, Hugentobler JP, Paolaggi JA. [Acute hepatitis caused by erythromycin propionate] Gastroenterol Clin Biol 1982; 6: 594. French. [PubMed: 7117770](Third reported case of hepatitis from erythromycin propionate; 58 year old man developed abdominal pain and fever within 8 hours of taking drug [bilirubin 2.7 mg/dL, ALT 55 U/L, Alk P 5.4 times ULN], resolving within 1 week of stopping).
- Funck-Brentano C, Pessayre D, Benhamou JP. [Hepatitis caused by various derivatives of erythromycin] Gastroenterol Clin Biol 1983; 7: 362-9. French. [PubMed: 6347792]
- Hosker JP, Jewell DP. Transient, selective factor X deficiency and acute liver failure following chest infection treated with erythromycin BP. Postgrad Med J 1983; 59: 514-5. [PMC free article: PMC2417580] [PubMed: 6622343](57 year old man developed "acute liver failure" and coagulopathy arising after 6 days of therapy with oral erythromycin base [bilirubin 2.0 mg/dL, AST 61 U/L, Alk P 866 U/L, protime 19.6 seconds], with eventual recovery).
- Inman WH, Rawson NS. Erythromycin estolate and jaundice. Br Med J (Clin Res Ed) 1983; 286: 1954-5. [PMC free article: PMC1548281] [PubMed: 6407653](Survey of ~5000 physicians using erythromycin in UK during 2 months of 1982, 3 reports of jaundice attributable to drug, all due to erythromycin stearate).
- Paliard P, Stremsdoerfer N, Moindrot H. [Acute hepatitis caused by erythromycin esters (propionate and ethylsuccinate)] Gastroenterol Clin Biol 1983; 7: 100-1. French. [PubMed: 6601598](54 year old man developed cholecystitis-like syndrome after 15 days of erythromycin propionate; 2 years later patient received erythromycin ethylsuccinate and developed fever and jaundice 7 days later [bilirubin 3.8 mg/dL, ALT 194 U/L, Alk P 148 U/L], resolving within 3 weeks; then had positive response to deliberate rechallenge with propionate with fever and ALT rising to 323 U/L in 24 hours).
- Phillips KG. Hepatotoxicity of erythromycin ethylsuccinate in a child. Can Med Assoc J 1983; 129: 411-2. [PMC free article: PMC1875174] [PubMed: 6603894](9 year old boy developed right upper quadrant pain after 7 days of erythromycin ethylsuccinate therapy [bilirubin 3.1 mg/dL, AST 258 U/L, Alk P 424 U/L], resolving within 15 days of stopping).
- Diehl AM, Latham P, Boitnott JK, Mann J, Maddrey WC. Cholestatic hepatitis from erythromycin ethylsuccinate. Am J Med 1984; 76: 931-4 . [PubMed: 6609640](46 and 54 year old women developed acute cholestatic hepatitis from erythromycin ethylsuccinate with latency of 2 and 6 days [with previous exposures] and ALT 98-405 U/L, Alk P 206-234 U/L [normal <33], and recovery within 2-6 weeks).
- Ortuño JA, Olaso V, Berenguer J. [Cholestasis hepatitis caused by erythromycin propionate] Med Clin (Barc) 1984; 82: 912. Spanish. [PubMed: 6748800](38 year old woman developed fever followed by jaundice and pruritus 15 days after starting erythromycin propionate [bilirubin 11.9 mg/dL, ALT 128 U/L, Alk P 246 U/L]; biopsy showed intrahepatic cholestasis, resolved within 5 weeks of stopping).
- Patel J, Schneider R. Hepatotoxic reaction to erythromycin ethylsuccinate. South Med J 1984; 77: 1343-4. [PubMed: 6333077](70 year old woman developed fatigue after 2 weeks of erythromycin ethylsuccinate therapy [bilirubin 1.3 mg/dL, ALT 254 U/L, Alk P 314 U/L] with rapid recovery upon stopping).
- García Monzón C, Noguerado A, Hidalgo S, Escudero V. [Cholestatic hepatitis caused by erythromycin estolate] Rev Clin Esp 1985; 177: 420-1. Spanish. [PubMed: 3836470]
- Pessayre D, Larrey D, Funck-Brentano C, Benhamou JP. Drug interactions and hepatitis produced by some macrolide antibiotics. J Antimicrob Chemother 1985; 16 Suppl A: 181-94. [PubMed: 3877043](Review of hepatic effects of macrolides: 55 published cases of hepatitis from estolate, 10 from ethylsuccinate, and 3 from propionate; usually with a mixed enzyme pattern, fever in 59%, eosinophilia in 45%, “outcome is always favorable”).
- Simon C, Roul G, Chabrier G, Schlienger JL, Imler M. [Hepatic involvement induced by erythromycin propionate] Rev Med Interne 1985; 6: 84-5. French. [PubMed: 4001646]
- Alcalay J, Halevy S, Theodor E, Sandbank M. Asymptomatic liver injury due to erythromycin stearate. Drug Intell Clin Pharm 1986; 20: 601-2. [PubMed: 3743417](73 year old woman found to have enzyme elevations [bilirubin normal, ALT 126 U/L, Alk P 178 U/L] 36 hours after starting erythromycin stearate, resolving with stopping drug within 2 weeks; no symptoms or jaundice: Case 2).
- Swayne LC, Kolc J. Erythromycin hepatotoxicity. A rare cause of a false-positive technetium-99m DISIDA study. Clin Nucl Med 1986; 11: 10-2. [PubMed: 3943237](39 year old woman developed abdominal pain and fever after 3 days of erythromycin estolate therapy [bilirubin 1.9 mg/dL, ALT 417 U/L, Alk P 250 U/L] and abnormal hepatobiliary radiotracer scan, but normal on follow up).
- Perrier M, Portier G, de Calan L, et al. [Erythromycin-induced hepatitis] Cah Anesthesiol 1987; 35: 237. French. [PubMed: 3621021]
- Geubel AP, Nakad A, Rahier J, Dive C. Prolonged cholestasis and disappearance of interlobular bile ducts following chlorpropamide and erythromycin ethylsuccinate. Case of drug interaction? Liver 1988; 8: 350-3. [PubMed: 3265170](52 year old man developed vanishing bile duct syndrome leading to cirrhosis and death 2 years later, which arose after an acute cholestatic hepatitis with fever, rash and eosinophilia [bilirubin 8.0 mg/dL, ALT 159 U/L, Alk P 1156 U/L] after 3 weeks of erythromycin ethylsuccinate therapy, but also 4 months after starting chlorpropamide).
- Luherne JY, Pariente EA, Maitre F. [Crossed hepatotoxicity of erythromycin propionate and troleandomycin?] Gastroenterol Clin Biol 1988; 12: 869-70. French. [PubMed: 3265396]
- Rigauts HD, Selleslag DL, Van Eyken PL, Van Damme BJ, Fevery JM, Marchal GJ. Erythromycin-induced hepatitis: simulator of malignancy. Radiology 1988; 169: 661-2. [PubMed: 3055031](67 year old woman developed jaundice and pruritus 2 weeks after starting erythromycin estolate [bilirubin 2.3 mg/dL, ALT 219 U/L, Alk P 180 U/L] with liver-spleen scan showing changes suggestive of multiple metastases, biopsy showing cholestatic hepatitis and repeat scan 10 weeks later was normal).
- Dubois A, Nakache N, Raffanel C, Balmes JL. [Acute cholestatic hepatitis after ingestion of roxithromycin] Gastroenterol Clin Biol 1989; 13: 317-8. French. [PubMed: 2731688](58 year old woman developed jaundice 4 days after starting a 5-day course of roxithromycin [introduced in France in 1987] with bilirubin 4.9 mg/dL, Alk P 442 U/L, ALT 46 U/L, and full recovery within 2 months of stopping).
- García Buey L, García-Samaniego Rey J, González Estecha A, Pajares García JM. [Hepatotoxicity of erythromycin] Rev Clin Esp 1989; 184: 158. Spanish. [PubMed: 2785700]
- Alemayehu G, Näslund I. [Erythromycin caused liver injury and gallbladder inflammation] Lakartidningen 1990; 87: 2866. Swedish. [PubMed: 2215004]
- Bojarska-Dahlig H. Hepatotoxicity of macrolide antibiotics. J Antimicrob Chemother 1990; 25: 475-7. [PubMed: 2338425](Discussion of relative rates of liver injury in rats based upon molecular weight and erythromycin equivalents).
- Delcourt A, Lambert M, Brenard R, Geubel A. Reversible liver injury possibly due to roxithromycin therapy. Acta Clin Belg 1990; 45: 206-7. [PubMed: 2166418](Second case of roxithromycin-induced liver injury, in a 43 year old man with onset of jaundice after 1 week of therapy [bilirubin 3.5 mg/dL, ALT 147 U/L, Alk P 477 U/L, GGT 950 U/L], resolving within 3 weeks of stopping).
- de Escalante B, Sampedro JA, Zabala S, Gracia P. [Cholestatic hepatitis caused by erythromycin propionate] An Med Interna 1990; 7: 656. Spanish. [PubMed: 2135589]
- Gholson CF, Warren GH. Fulminant hepatic failure associated with intravenous erythromycin lactobionate. Arch Intern Med 1990; 150: 215-6. [PubMed: 2297290](72 year old man developed liver injury after 7 days of iv erythromycin therapy [bilirubin 3.0 mg/dL rising to 14.1 mg/dL, AST 450 rising to 1420 U/L, Alk P 108 U/L] with rapid progression to liver failure and death within a week).
- Serrano Heranz R, Ziad F. [Hepatotoxicity caused by erythromycin ethylsuccinate] An Med Interna 1990; 7: 215. Spanish. [PubMed: 2103790]
- Caballeria Rovira E, Arago López JV, Masso Ubeda RM, Sanchis Closa A. [Hepatotoxicity due to erythromycin ethylsuccinate] Rev Esp Enferm Dig 1991; 80: 356. Spanish. [PubMed: 1768482]
- Lehtonen L, Lankinen KS, Wikberg R, Rita H, Salmi HA, Valtonen V. Hepatic safety of erythromycin acistrate in 1549 patients with respiratory tract or skin infections. J Antimicrob Chemother 1991; 27: 233-42. [PubMed: 1676027](Post-marketing evaluation of enzyme elevations during 7-14 day courses of erythromycin acistrate, a prodrug: ALT elevations occurred in ~8% before and ~15% after the courses, usually mild and transient; only 3 [0.2%] attributed to drug).
- Degott C, Feldmann G, Larrey D, Durand-Schneider AM, Grange D, Machayekhi JP, Moreau A, et al. Drug-induced prolonged cholestasis in adults: a histological semiquantitative study demonstrating progressive ductopenia. Hepatology 1992; 15: 244-51. [PubMed: 1735527](Clinical and histological description of drug-induced prolonged cholestasis and ductopenia, the severe form of which can lead to vanishing bile duct syndrome, cirrhosis and hepatic failure: 8 cases with 3 due to ajmaline and one each to cyamemazine, troleandomycin, erythromycin, amitriptyline, and cyproheptadine).
- Saiz Santos S, Montero López L. [Hepatotoxicity from erythromycin estolate] Aten Primaria 1992; 10: 1050. Spanish. [PubMed: 1467424]
- Carson JL, Strom BL, Duff A, et al. Acute liver disease associated with erythromycins, sulfonamides, and tetracyclines. Ann Intern Med 1993; 119(7 Pt 1): 576-83. [PubMed: 8363168](In Medicaid records between 1980-87, 107 patients were hospitalized for acute hepatitis of unknown cause, 5 [4.7%] of whom had received erythromycins compared to 0.9% of controls. No case received estolate).
- Derby LE, Jick H, Henry DA, Dean AD. Erythromycin-associated cholestatic hepatitis. Med J Aust 1993; 158: 600-2. [PubMed: 8479375](Retrospective cohort study of 366,064 people who received erythromycin in UK database, found 13 cases of cholestatic hepatitis of uncertain cause within 45 days of prescription: risk=3.6/100,000 similar for ethylsuccinate and base preparations [estolate and stearate rarely used]: risk increased with age and was independent of sex).
- Esteban A, Molina MJ, Soto C, Hernández G. [Acute cholestatic hepatitis due to roxithromycin] Rev Clin Esp 1993; 192: 352-3. Spanish. [PubMed: 8497745]
- Gross R, Mion F, Paliard P. [Cholestasis induced by roxithromycin in a patient with a past history of pregnancy intrahepatic cholestasis] Gastroenterol Clin Biol 1993; 17: 146-7. French. [PubMed: 8500706]
- Howe E, Howe E, Benn RA. Hepatotoxicity due to erythromycin ethylsuccinate. Med J Aust 1993; 158: 142-4. [PubMed: 8419773](3 adults with fever and right upper quadrant pain, 2 with jaundice, within few days of starting erythromycin ethylsuccinate, [with history of previous exposures] similar syndrome to that of estolate).
- Pedersen FM, Bathum L, Fenger C. Acute hepatitis and roxithromycin. Lancet 1993; 341: 251-2. [PubMed: 8093543](23 year old woman developed jaundice and fever after 4 days of roxithromycin therapy [bilirubin 7 mg/dL, ALT 4630 U/L, protime 17%], resolving within 3 weeks; possible contribution of acetaminophen use).
- Danan G, Bénichou C. Roxithromycin-induced or herpes hepatitis? Lancet 1993; 341: 896-7. [PubMed: 8096597](Letter from manufacturer in response to Pederson et al questioning the role of roxithromycin).
- Pérez Gutthann S, García Rodríguez LA. The increased risk of hospitalizations for acute liver injury in a population with exposure to multiple drugs. Epidemiology 1993; 4: 496-501. [PubMed: 8268277](Case control study from Canadian Health Plan records, 1982-6, risk of hospitalization for liver injury was 1/100,000 for NSAIDs and 14/100,000 for erythromycin estolate [no case related to other types of erythromycin] and risk increased if multiple known hepatotoxins were used).
- Periti P, Mazzei T, Mini E, Novelli A. Adverse effects of macrolide antibacterials. Drug Saf 1993; 9: 346-64. [PubMed: 8280403](Extensive review of literature on adverse events reported with macrolide antibiotics).
- Ducloux D, Welker Y, Modai J. [Pseudo-cholangitis, a form of erythromycin-induced hepatitis] Presse Med 1995; 24: 1663. French. [PubMed: 8545387]
- Gilbert FI Jr. Cholestatic hepatitis caused by esters of erythromycin and oleandomycin. 1962. Hawaii Med J 1995; 54: 603-5. [PubMed: 7642362]
- Hautekeete ML. Hepatotoxicity of antibiotics. Acta Gastroenterol Belg 1995; 58: 290-6. [PubMed: 7491842](Review of hepatotoxicity associated with antibiotics; the erythromycins are mentioned as well known to cause cholestatic hepatitis).
- Tomei F, Iavicoli S, Iavicoli A, Papaleo B, Baccolo TP. Liver damage in pharmaceutical industry workers. Arch Environ Health 1995; 50: 293-7. [PubMed: 7677429](Study of 40 Italians working in a pharmaceutical plant producing erythromycin found 37% to have elevated ALT levels compared to 6% in controls working elsewhere; no frank hepatitis or markedly elevated values).
- von Rosensteil NA, Adam D. Macrolide antibacterials. Drug interactions of clinical significance. Drug Saf 1995; 13: 105-22. [PubMed: 7576262]
- George DK, Crawford DH. Antibacterial-induced hepatotoxicity. Incidence, prevention and management. Drug Saf 1996; 15: 79-85. [PubMed: 8862966](Review of hepatotoxicity of antibiotics including macrolides from Australia).
- Pillans PI. Drug associated hepatic reactions in New Zealand: 21 years experience. N Z Med J 1996; 109: 315-9. [PubMed: 8816722](Erythromycin ranked 1st as a cause of liver adverse drug reactions in New Zealand from 1974 to 1995, accounting for ~12% of cases).
- Viluksela M, Vainio PJ, Tuominen RK. Cytotoxicity of macrolide antibiotics in a cultured human liver cell line. J Antimicrob Chemother 1996; 38: 465-73. [PubMed: 8889721](In vitro study of cytotoxicity of macrolides).
- Vial T, Biour M, Descotes J, Trepo C. Antibiotic-associated hepatitis: update from 1990. Ann Pharmacother 1997; 31: 204-20. [PubMed: 9034423](Extensive review including discussion of macrolides [erythromycin, clarithromycin and azithromycin]; ALT elevations occur in 0.4-1.2% of patients treated with macrolides but similar rates found in placebo controls; rare instances of cholestatic hepatitis attributed to all three).
- Wong PW, Dillard TA, Kroenke K. Multiple organ toxicity from addition of erythromycin to long-term lovastatin therapy. South Med J 1998; 91: 202-5. [PubMed: 9496876](73 year old man on long term lovastatin therapy developed rhabdomyolysis [CPK 4235 U/L, AST 476 U/L, ALT 236 U/L, bilirubin 1.1 mg/dL, GGT 30 U/L] after receiving 2 weeks of erythromycin [which may have altered the metabolism of the statin causing elevated levels and muscle injury]; renal failure occurred but patient ultimately recovered).
- Horn S, Aglas F, Horina JH. Cholestasis and liver cell damage due to hypersensitivity to erythromycin stearate--recurrence following therapy with erythromycin succinate. Wien Klin Wochenschr 1999; 111: 76-7. [PubMed: 10081126](Woman developed cholestatic hepatitis after both erythromycin stearate and succinate).
- Principi N, Esposito S. Comparative tolerability of erythromycin and newer macrolide antibacterials in paediatric patients. Drug Saf 1999; 20: 25-41. [PubMed: 9935275]
- Lazarczyk DA, Duffy MC. Erythromycin-induced primary biliary cirrhosis. Dig Dis Sci 2000; 45: 1115-8. [PubMed: 10877225](48 year old woman developed jaundice and pruritus 3 weeks after an 8-day course of erythromycin [bilirubin 4.1 mg/dL, ALT 249 U/L, Alk P 336 U/L] with rapid resolution but finding of mitochrondial antibody [AMA] and persistence of mildly abnormal liver enzymes [bilirubin 0.2 mg/dL, ALT 58 U/L, Alk P 120 U/L] led to a liver biopsy 6 months later that showed primary biliary cirrhosis).
- Chitturi S, Farrell GC. Drug-induced cholestasis. Semin Gastrointest Dis 2001; 12: 113-24. [PubMed: 11352118](Review of cholestatic forms of drug-induced liver disease with case report of 70 year old man who developed prolonged jaundice and pruritus starting 8 weeks after a 1-week course of erythromycin base [bilirubin 18 mg/dL, ALT 62 U/L, Alk P 277 U/L]; liver biopsy showing fibrosis and duct paucity at 18 months and ultimate clinical recovery despite persistence of mild Alk P elevations for 10 years thereafter).
- Easton-Carter KL, Hardikar W, Smith AL. Possible roxithromycin-induced fulminant hepatic failure in a child. Pharmacotherapy 2001; 21: 867-70. [PubMed: 11444584](5 year old child developed fever and rash 1 day after 5- day course of roxithromycin followed by jaundice [bilirubin 17 mg/dL, ALT 1912 U/L, Alk P 480 U/L] progressing to hepatic failure requiring liver transplantation).
- Pari L, Uma A. Protective effect of Sesbania grandiflora against erythromycin estolate-induced hepatotoxicity. Therapie 2003; 58: 439-43. [PubMed: 14682193](Study of prevention of erythromycin hepatic injury in rats with herbals).
- Akcay A, Kanbay M, Sezer S, Ozdemir FN. Acute renal failure and hepatotoxicity associated with roxithromycin. Ann Pharmacother 2004; 38: 721-2. [PubMed: 14766998](73 year old woman developed fever and arthralgias after 2 days of roxithromycin therapy followed by renal insufficiency [creatinine 3.9 mg/dL, bilirubin not given, ALT 225 U/L, GGT 227 U/L, 25% eosinophilia], resolving within 1 week without dialysis).
- Pari L, Murugan P. Protective role of tetrahydrocurcumin against erythromycin estolate-induced hepatotoxicity. Pharmacol Res 2004; 49: 481-6. [PubMed: 14998559](Study of prevention of hepatic injury in rats with anti-oxidants).
- Björnsson E, Jerlstad P, Bergqvist A, Olsson R. Fulminant drug-induced hepatic failure leading to death or liver transplantation in Sweden. Scand J Gastroenterol 2005; 40: 1095-101. [PubMed: 16165719](Review of fatal adverse drug event reports of liver injury in Sweden between 1966 and 2002, found 103 cases, one attributed to erythromycin).
- Karthik SV, Casson D. Erythromycin-associated cholestatic hepatitis and liver dysfunction in children: the British experience. J Clin Gastroenterol 2005; 39: 743-4. [PubMed: 16082288](10 year old girl developed abdominal pain within a day of starting erythromycin ethylsuccinate therapy followed by jaundice [bilirubin 14.1 mg/dL, ALT 278 U/L, GGT 4 times ULN], resolving within 8 weeks of stopping).
- Chang CY, Schiano TD. Drug hepatotoxicity. Aliment Pharmacol Ther 2007; 25: 1135-51. [PubMed: 17451560](Review article summarizing large cohort studies in which erythromycin or the macrolides were often among the most common causes of liver injury).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J; Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008; 135: 1924-34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug-induced liver disease in the U.S. collected from 2004 to 2008, 5 cases were attributed to telithromycin and 3 to azithromycin as single agents but none to erythromycin or clarithromycin).
- Leitner JM, Graninger W, Thalhammer F. Hepatotoxicity of antibacterials: pathomechanisms and clinical data. Infection 2010; 38; 3-11. [PubMed: 20107858](Review; the macrolide antibiotics may cause cholestatic hepatitis at an estimated rate of 3.6 for erythromycin, 3.8 for clarithromycin, and 5.5 cases per 100,000 prescriptions for telithromycin, compared to 10 for sulfonamides and 2000 per 100,000 for isoniazid).
- Ferrajolo C, Capuano A, Verhamme KM, Schuemie M, Rossi F, Stricker BH, Sturkenboom MC. Drug-induced hepatic injury in children: a case/non-case study of suspected adverse drug reactions in VigiBase. Br J Clin Pharmacol 2010; 70: 721-8. [PMC free article: PMC2997312] [PubMed: 21039766](World wide pharmacovigilance database containing 9036 hepatic adverse drug reactions in children includes 63 cases attributed to azithromycin, 60 to erythromycin and 35 to clarithromycin).
- Reuben A, Koch DG, Lee WM; Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology 2010; 52: 2065-76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, of which 31 were due to antibiotics, but none were attributed to erythromycin).
- Lee CH, Wang JD, Chen PC; Health Data Analysis in Taiwan (hDATa) Research Group. Case-crossover design: an alternative strategy for detecting drug-induced liver injury. J Clin Epidemiol 2012; 65: 560-7. [PubMed: 22445086](Analysis of the Taiwan National Health Insurance database from 1997 to 2004 found an adjusted odds ratio of 2.1 to 2.5 for hospitalization, with unexplained liver injury within 30 days of a prescription for erythromycin).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 2013; 114: 1419-25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, none of which were attributed to erythromycin or other macrolide antibiotics).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol 2014; 13: 231-9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, one of which was attributed to clarithromycin [acute liver failure], but none were attributed to erythromycin).
- Ferrajolo C, Coloma PM, Verhamme KM, Schuemie MJ, de Bie S, Gini R, Herings R, et al.; EU-ADR consortium. Signal detection of potentially drug-induced acute liver injury in children using a multi-country healthcare database network. Drug Saf 2014; 37: 99-108. [PubMed: 24446276](Analyses of large spontaneous reporting databases from 3 European countries between 1995 and 2010 identified 125 drugs with at least one exposed case of unexplained acute liver injury in children, 20 of which had a statistically significant association, including clarithromycin [5 cases] and erythromycin [4 cases], but not azithromycin).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 323 [36%] were attributed to antibiotics including 29 due to marolides, of which 18 were linked to azithromycin, 2 clarithromycin, 2 erythromycin and 7 telithromycin: Case 3).
- Ferrajolo C, Verhamme KM, Trifirò G, 't Jong GW, Picelli G, Giaquinto C, Mazzaglia G, et al. Antibiotic-induced liver injury in paediatric outpatients: a case-control study in primary care databases. Drug Saf 2017; 40: 305-15. [PMC free article: PMC5362651] [PubMed: 28025733](In a health care database of 429,772 children in Italy and the Netherlands followed between 2008 and 2010, 938 cases of liver injury of uncertain cause were identified, the rate being higher in those with current use of antibiotics [12% vs 3.6%] for an adjusted odds rate ratio [aOR] of 3.2; specific antibiotics most commonly implicated were fluoroquinolones [19.0], cephalosporins [4.5], macrolides [3.5] and penicillins [2.6]; no specific mention of erythromycin).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Assessment of Long-Term Macrolide Exposure on the Oropharyngeal Microbiome and Macrolide Resistance in Healthy Adults and Consequences for Onward Transmission of Resistance.[Antimicrob Agents Chemother. 2...]Assessment of Long-Term Macrolide Exposure on the Oropharyngeal Microbiome and Macrolide Resistance in Healthy Adults and Consequences for Onward Transmission of Resistance.Burr LD, Taylor SL, Richard A, Schreiber V, Lingman S, Martin M, Papanicolas LE, Choo JM, Rogers GB. Antimicrob Agents Chemother. 2022 Apr 19; 66(4):e0224621. Epub 2022 Mar 16.
- Outcomes Following Macrolide Use in Kidney Transplant Recipients.[Can J Kidney Health Dis. 2019]Outcomes Following Macrolide Use in Kidney Transplant Recipients.Jeong R, Quinn RR, Lentine KL, Lloyd A, Ravani P, Hemmelgarn B, Braam B, Garg AX, Wen K, Wong-Chan A, et al. Can J Kidney Health Dis. 2019; 6:2054358119830706. Epub 2019 Feb 21.
- Impact of Long-Term Erythromycin Therapy on the Oropharyngeal Microbiome and Resistance Gene Reservoir in Non-Cystic Fibrosis Bronchiectasis.[mSphere. 2018]Impact of Long-Term Erythromycin Therapy on the Oropharyngeal Microbiome and Resistance Gene Reservoir in Non-Cystic Fibrosis Bronchiectasis.Choo JM, Abell GCJ, Thomson R, Morgan L, Waterer G, Gordon DL, Taylor SL, Leong LEX, Wesselingh SL, Burr LD, et al. mSphere. 2018 Apr 25; 3(2). Epub 2018 Apr 18.
- Review Dental therapeutic indications for the newer long-acting macrolide antibiotics.[J Am Dent Assoc. 1999]Review Dental therapeutic indications for the newer long-acting macrolide antibiotics.Moore PA. J Am Dent Assoc. 1999 Sep; 130(9):1341-3.
- Review The use of erythromycin as a gastrointestinal prokinetic agent in adult critical care: benefits versus risks.[J Antimicrob Chemother. 2007]Review The use of erythromycin as a gastrointestinal prokinetic agent in adult critical care: benefits versus risks.Hawkyard CV, Koerner RJ. J Antimicrob Chemother. 2007 Mar; 59(3):347-58. Epub 2007 Feb 8.
- Erythromycin - LiverToxErythromycin - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...