NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Dactinomycin is an intravenously administered, antineoplastic antibiotic that is used in the treatment of solid tumors in children and choriocarcinoma in adult women. In high doses, dactinomycin can cause severe liver injury including sinusoidal obstruction syndrome.
Background
Dactinomycin (dak” tin oh mye’ sin) is one of the actinomycins, anticancer antibiotics that were discovered by Selman Waksman and colleagues in the 1940s using fermentation exacts from bacteria (Streptomyces). The actinomycins are chromopeptides which bind to double-helical DNA and interrupt RNA transcription, causing cell arrest and inhibition of cell division. Actinomycin D, later named dactinomycin, was isolated from Streptococcus parvullus and was identified as a promising antineoplastic agent. Subsequently, dactinomycin was shown to have antitumor effect against a broad array of solid tumors. Dactinomycin was formally approved for use in the United States in 1964 and continues to be a valuable agent in the therapy of solid tumors of childhood (Wilms tumor, rhabdomyosarcoma) and in choriocarcinoma in adult women. Dactinomycin is available as a solution or lyophilized powder for injection in vials of varying concentrations under the commercial name Cosmegen and must be given by the intravenous route, avoiding tissue extravasation. The dose is based upon indication and body weight; a typical regimen is 10 to 15 mcg/kg daily for 5 days, with repeat courses every 2 to 4 weeks based upon tolerance and antitumor effects. Dactinomycin can also be given as a component of regional perfusion regimens for solid malignancies. Side effects of dactinomycin include bone marrow suppression, anorexia, nausea, diarrhea, glossitis, proctitis, oral ulcers, alopecia, erythema and skin rash.
Hepatotoxicity
Chemotherapy with dactinomycin in combination with other agents is associated with serum enzyme elevations in a high, but variable proportion of patients depending upon the dose, other agents used as well as the frequency of monitoring and criteria used to define elevations. The ALT elevations are usually asymptomatic and transient and may resolve without dose modification. In many instances, it is difficult to attribute the liver test abnormalities to dactinomycin, because of the exposure to other potentially hepatotoxic agents.
Dactinomycin can also cause a distinctive form of clinically apparent liver injury referred to as hepatopathy-thrombocytopenia syndrome (HTS) that can be severe and even fatal. This syndrome appears to be due to sinusoidal obstruction, but there may also be an element of direct hepatic and bone marrow injury. In large studies, between 1% and 5% of children with cancer treated with regimens including dactinomycin developed acute hepatic injury and thrombocytopenia suggestive of HTS. The syndrome is more common in younger children and with higher doses of dactinomycin. The time to onset is typically within 3 to 6 weeks after the initial dose, often arising 5 to 10 days after the 2nd or 3rd course of cyclic chemotherapy with dactinomycin. The onset of symptoms is sudden, and children characteristically present with right upper quadrant pain or tenderness, hepatomegaly, liver test abnormalities and signs of excessive bleeding such as epistaxis or bruising. Serum aminotransferase levels are markedly elevated (10 to 100 times ULN) early in the course, but fall rapidly and can be normal within 7 to 14 days. The platelet count is generally less than 25,000/μL and also resolves rapidly. Serum alkaline phosphatase is typically normal and bilirubin levels are minimally elevated, except if the course is progressive and fatal. Serum ammonia and INR may also be raised, and ascites often develops during the acute syndrome. The overall pattern of injury resembles acute hepatic necrosis, and liver histology shows centrolobular necrosis and evidence of sinusoidal obstruction. Recovery is rapid and usually complete.
Likelihood score: C (Probable cause of clinically apparent liver injury).
Mechanism of Injury
Dactinomycin is a direct toxin and likely causes acute damage to hepatic sinusoidal endothelial cells, resulting in sinusoidal obstruction and acute toxic injury to hepatocytes.
Outcome and Management
The acute hepatic injury caused by dactinomycin is usually self-limiting in course and reversible. Management should focus on supportive care. The mortality rate ranges from 5% to 20%, but most children recover rapidly. Interestingly, the liver injury usually does not recur with retreatment at least with reduced doses of dactinomycin, and long term hepatic consequences are rare.
Drug Class: Antineoplastic Agents
Other Drugs in the Subclass, Antibiotics, Cytotoxic: Bleomycin, Daunorubicin, Doxorubicin, Epirubicin, Idarubicin, Mitomycin, Mitoxantrone, Plicamycin
CASE REPORT
Case 1. Acute hepatotoxicity due to dactinomycin therapy.
[Modified from Case 1 in: Farruggia P, Macaluso A, Tropia S, Di Marco F, Russo D, Grigoli A, Trizzino A, D'Angelo P. Hepatopathy-thrombocytopenia syndrome (HTS) after actinomycin-D therapy: report of three cases and review of the literature. Pediatr Hematol Oncol 2011; 28: 237-43. PubMed Citation]
An 18 month old girl with Wilms tumor underwent diagnostic and therapeutic resection and was started on dactinomycin [1.5 mg/m2] and vincristine [1.5 mg/m2]. Nine days after the first course and just after a second dose of vincristine, she developed fever, pallor, marked bruising of the skin, hepatomegaly and ascites. Blood tests showed a hemoglobin of 6.1 g/dL, platelet count 9000/μL, bilirubin 1.1 mg/dL [direct 0.6], ALT 579 U/L, AST 1832 U/L, LDH 5082 U/L and partial thromboplastin time 36 seconds. Serum ammonia levels were normal. Chemotherapy was held and she was monitored (Table). She worsened for several days, but then began to improve and was discharged 15 days later with normal liver tests. Chemotherapy was resumed and she achieved a complete remission and was without evidence of recurrence 12 years later.
Key Points
Laboratory Values
Comment
This distinctive syndrome is commonly referred to as “hepatopathy-thrombocytopenia Syndrome” (HTS) and occurs in 1% to 5% of children who receive cyclic chemotherapy with dactinomycin for treatment of solid tumors such as Wilms tumor and rhabdomyosarcoma. Risk factors appear to be younger age (less than 3 years) and higher doses of dactinomycin. The clinical presentation is striking, with sudden onset of painful hepatomegaly and marked thrombocytopenia with epistaxis, bruising or bleeding. Despite the dire features of the presenting illness, recovery is usually rapid and complete. Strikingly, patients may later tolerate dactinomycin therapy, sometimes in unmodified doses. The cause of HTS is unknown but it resembles acute sinusoidal obstruction syndrome, although the rapidly of recovery is somewhat atypical for this form of hepatic injury. A similar syndrome has been reported in adults treated with dacarbazine (DTIC). An atypical feature of this case was the appearance after the first course of chemotherapy; presentation within a few days of the second or third course being more typical.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Dactinomycin – Generic, Cosmegen®
DRUG CLASS
Antineoplastic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Dactinomycin | 50-76-0 | C62-H86-N12-O16 |
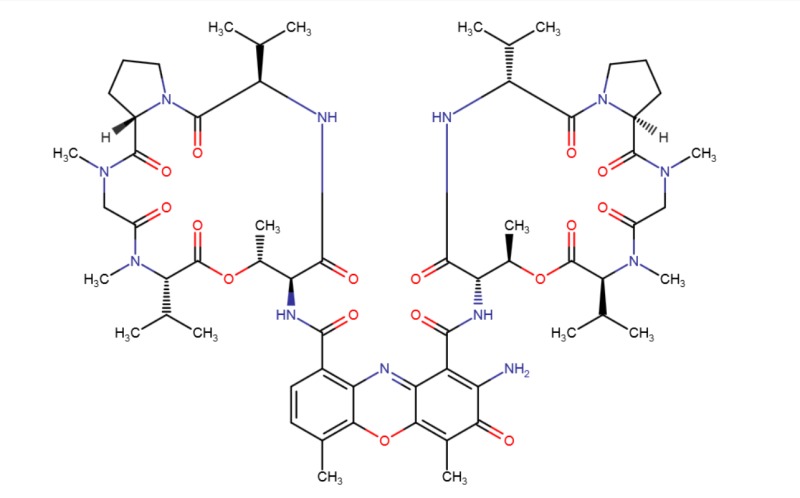 |
ANNOTATED BIBLIOGRAPHY
References updated: 14 November 2017
- Zimmerman HJ. Antibiotics. Hepatotoxic effects of oncotherapeutic and immunosuppressive agents. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 694-8.(Expert review of hepatotoxicity of cancer chemotherapeutic agents published in 1999 mentions that dactinomycin appears to have little hepatotoxic potential, except when given in high doses or with irradiation which can result in sinusoidal obstruction syndrome).
- DeLeve LD. Cancer chemotherapy. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 541-68.(Review of hepatotoxicity of cancer chemotherapeutic agents mentions that dactinomycin can cause sinusoidal obstruction syndrome, particularly in children with large, right sided Wilms tumor and partial outflow obstruction, which may contribute to the syndrome).
- Chabner BA, Bertino J, Cleary J, Ortiz T, Lane A, Supko JG, Ryan DP. Antibiotics. Cytotoxic agents. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1712-5.(Textbook of pharmacology and therapeutics).
- Harris F, Cullity G, Lister J. Hepatitis following actinomycin D and irradiation. Proc R Soc Med. 1974; 67: 756-7. [PMC free article: PMC1645831] [PubMed: 4371666](3 year old boy with Wilms tumor treated with dactinomycin and radiotherapy developed sinusoidal obstruction syndrome with edema and ascites 2 month after starting chemotherapy [bilirubin 1.7, ALT 700 U/L, platelets 18,000/μL], ultimately resolving).
- McVeagh P, Ekert H. Hepatotoxicity of chemotherapy following nephrectomy and radiation therapy for right-sided Wilms tumor. J Pediatr 1975; 87: 627-8. [PubMed: 169340](Two 4 year old girls with Wilms tumor developed hepatomegaly, mild AST elevations [45 and 180 U/L] and thrombocytopenia 1-2 months after radiation therapy and starting cycles of dactinomycin and vincristine, resolving completely and later tolerating further dactinomycin therapy).
- Jayabose S, Shende A, Lanzkowsky P. Hepatotoxicity of chemotherapy following nephrectomy and radiation therapy for right-sided Wilms tumor. J Pediatr 1976; 88: 898. [PubMed: 178848](Letter in response to McVeagh [1975] with a similar case; 5 year old girl with Wilms tumor developed hepatomegaly 60 days after starting radiation therapy, dactinomycin and vincristine [bilirubin 2.3 mg/dL, ALT 100 U/L], biopsy showing centrilobular congestion and necrosis and liver scan showing a hepatic lesion, all of which ultimately resolved).
- Mihevc-Srakar N, Petrić-Grabnar G. [Actinomycin D: toxic effects with special reference to hepatic injury]. Bilt Hematol Transfuz 1979; 7: 85-90. Croatian. [PubMed: 552251](Description of two children treated with dactinomycin who developed hepatotoxicity similar to that described by McVeagh [1975]).
- Sznol M, Ohnuma T, Holland JF. Hepatic toxicity of drugs used for hematologic neoplasia. Semin Liver Dis 1987: 237-56. [PubMed: 3317861](Review of the hepatotoxicity of cancer chemotherapeutic agents; dactinomycin is not discussed).
- D'Angio GJ. Hepatotoxicity with actinomycin D. Lancet 1987; 2 (8550): 104. [PubMed: 2885556](5 of 40 children with Wilms tumor receiving pulsed, intensive regimens of dactinomycin developed "sharp rises in liver function test values", hepatomegaly and ascites; one died and the others recovered fully).
- Green DM, Finklestein JZ, Norkool P, D'Angio GJ. Severe hepatic toxicity after treatment with single-dose dactinomycin and vincristine. A report of the National Wilms' Tumor Study. Cancer 1988; 62: 270-3. [PubMed: 2838151](Further description of the 5 children with Wilms tumor who developed liver injury [ascites, hepatomegaly, AST 890 to 19,723 U/L] after 1 to 3 cycles of an intensive dose regimen of dactinomycin).
- Choonara IA, Kendall-Smith S, Bailey CC. Accidental actinomycin D overdosage in man, a case report. Cancer Chemother Pharmacol 1988; 21: 173-4. [PubMed: 3349565](17 year old boy with rhabdomyosarcoma received an overdose of dactinomycin [~3.3 instead of 2.5 mg/m2] and developed skin rash, peripheral edema, bone marrow suppression, diarrhea, hyponatremia, seizures and mild ALT elevations [rising from 66 to 150 U/L] but ultimately recovered completely).
- Pritchard J, Raine J, Wallendszus K. Hepatotoxicity of actinomycin-D. Lancet 1989; 1 (8630): 168. [PubMed: 2563091](Letter in response to D'Angio [1987]; among 279 children with Wilms tumor treated with dactinomycin in the UK, 4 [1.4%] developed severe hepatotoxicity, but 17 [6%] of children overall had severe thrombocytopenia without neutropenia, and some may have had a milder form of the same syndrome).
- D'Angio GJ; De Camargo B. Hepatotoxicity and actinomycin D. Lancet 1990; 335 (8700): 1290. [PubMed: 1971368](Two letters; D'Angio from the United States mentions that dactinomycin hepatotoxicity is seen even with the standard doses of dactinomycin used to treat Wilms tumor; De Camargo from Brazil mentions that 4 of 33 children with Wilms tumor treated with the pulsed intensive regimen developed hepatotoxicity, but no case was severe, yet one severe case occurred among the 32 children given the standard dosing regimen).
- Raine J, Bowman A, Wallendszus K, Pritchard J. Hepatopathy-thrombocytopenia syndrome - a complication of dactinomycin therapy for Wilms' tumor: a report from the United Kingdom Childrens Cancer Study Group. J Clin Oncol 1991; 9: 268-73. [PubMed: 1846405](Among 501 children with Wilms tumor treated in the UK, 6 developed a syndrome of severe hepatotoxicity with thrombocytopenia [bilirubin 1.3-6.1 mg/dL, ALT 335-5,731 U/L, Alk P 46-412 U/L, platelets 7,000-20,000/μL], all had received dactinomycin; the injury arising within 10 weeks of starting therapy, usually after the 3rd course, resolving in 7-14 days; several children later tolerated lower doses of dactinomycin).
- de Camargo B, Franco EL. A randomized clinical trial of single-dose versus fractionated-dose dactinomycin in the treatment of Wilms' tumor. Results after extended follow-up. Brazilian Wilms' Tumor Study Group. Cancer 1994; 73: 3081-6. [PubMed: 8200006](Abstract; 176 Brazilian children with Wilms tumor were randomized to receive dactinomycin in a standard 5 day fractionated course or in a 1 day, pulsed intensive course; response rates were similar and severe hepatotoxicity occurred in only one child who received the fractionated course).
- Arndt C, Hawkins D, Anderson JR, Breitfeld P, Womer R, Meyer W. Age is a risk factor for chemotherapy-induced hepatopathy with vincristine, dactinomycin, and cyclophosphamide. J Clin Oncol 2004; 22: 1894-901. [PubMed: 15143082](Among 339 children with rhabdomyo-sarcoma treated with dactinomycin, vincristine and cyclophosphamide, 18 [5%] developed hepatotoxicity [bilirubin 1.4-40 mg/dL, ALT 346-14,046 U/L], usually within 12 weeks of starting, 17 received dactinomycin, 11 with jaundice, 15 with ascites, 4 died; frequency was 15% in children less than 3 years and 4% in older children).
- Mao Y, Wan X, Lv W, Xie X. Relapsed or refractory gestational trophoblastic neoplasia treated with the etoposide and cisplatin/etoposide, methotrexate, and actinomycin D (EP-EMA) regimen. Int J Gynaecol Obstet 2007; 98: 44-7. [PubMed: 17481633](Among 18 patients with gestational trophoblastic cancer, hepatotoxicity arose after 17 of 74 cycles [23%] of chemotherapy using etoposide, cisplatin, methotrexate and dactinomycin, but most instances were mild and the timing, clinical features and source of the injury were not provided).
- Takeyama J, Ando R, Sato T, Nio M, Shimanuki Y, Sato A, Imaizumi M. Focal nodular hyperplasia-like lesion of the liver in a child previously treated for nephroblastoma. Pathol Int 2008; 58: 606-8. [PubMed: 18801077](6 year old boy was found to have focal nodular hyperplasia 4-5 years after chemotherapy for Wilms tumor with dactinomycin and vincristine, and an episode of sinusoidal obstruction syndrome).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J; Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008; 135: 1924-34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, several cases were attributed to antineoplastic agents [such as mercaptopurine, cyclophosphamide, docetaxel, temozolomide, bortezomib and imatinib], but none to dactinomycin).
- Reuben A, Koch DG, Lee WM; Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology 2010; 52: 2065-76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, including 2 attributed to antineoplastic agents, 1 to melphalan and 1 to gemtuzumab, but none to dactinomycin).
- Langholz B, Skolnik JM, Barrett JS, Renbarger J, Seibel NL, Zajicek A, Arndt CA. Dactinomycin and vincristine toxicity in the treatment of childhood cancer: a retrospective study from the Children's Oncology Group. Pediatr Blood Cancer 2011; 57: 252-7. [PMC free article: PMC3467305] [PubMed: 21671362](The rate of all severe toxicities of dactinomycin from 6 clinical trials in 4567 patients was 6% and these adverse events typically occurred early and decreased with cumulative dose).
- Lee AC, Goh PY. Dactinomycin-induced hepatic sinusoidal obstruction syndrome responding to treatment with N-acetylcysteine. J Cancer. 2011; 2: 527-31. [PMC free article: PMC3204401] [PubMed: 22043237](16 year old girl with Wilms tumor developed thrombocytopenia followed by SOS after 5 doses of vincristine and two of dactinomycin [bilirubin 1.1 mg/dL, ALT 746 U/L, ascites], improving rapidly with N-acetylcysteine therapy).
- Farruggia P, Macaluso A, Tropia S, Di Marco F, Russo D, Grigoli A, Trizzino A, D'Angelo P. Hepatopathy-thrombocytopenia syndrome (HTS) after actinomycin-D therapy: report of three cases and review of the literature. Pediatr Hematol Oncol 2011; 28: 237-43. [PubMed: 21271778](Three children, ages 15-23 months, with Wilms tumor or rhabdomyosarcoma who received dactinomycin developed severe hepatotoxicity with thrombocytopenia [peak bilirubin 1.0, 3.4, and 2.6 mg/dL, ALT 1000, 851, and 2161 U/L, LDH 6445, 3912 and 10,102 U/L, platelets 9000, 3000 and 11,000/μL], one died while 2 recovered and later tolerated continuation of chemotherapy: Case 1).
- Martín-Lázaro JF, Palanca D, Garcia-Iñiguez JP, Madurga P, Carboné A. Hepatopathy-thrombocytopenia syndrome after actinomycin-D therapy: treatment with defibrotide. Pediatr Hematol Oncol 2013; 30: 25-7. [PubMed: 23216129](13 year old female with Wilm tumor developed abdominal pain and fever during a second course of dactinomycin and vincristine [bilirubin 1.7 mg/dL, ALT 1580 U/L, platelet count not given] with worsening coagulopathy and weight gain; was treated with defibrotide [25 mg/kg daily for 14 days] for SOS and recovered rapidly).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 49 were attributed to antineoplastic agents, but none to dactinomycin).
- Baskin Y, Amirfallah A, Calibasi G, Olgun N. Hepatopathy-thrombocytopenia syndrome during actinomycin D treatment may be related to MDR1 (ABCB1) gene polymorphisms. Am J Ther 2016; 23: e594-6. [PubMed: 24413370](3.5 year old female with Wilm Tumor developed severe thrombocytopenia during a 4th monthly cycle of dactinomycin and vincristine [bilirubin 0.9 mg/mL, ALT 53 U/L, AST 93 U/L, LDH 332 U/L, platelets 11,000 cells/µL] and was found to have multiple variants of MDR1, but recovered rapidly and later tolerated further cycles of dactinomycin).
- Shi Q, Yang X, Greenhaw JJ, Salminen AT, Russotti GM, Salminen WF. Drug-Induced liver injury in children: clinical observations, animal models, and regulatory status. Int J Toxicol 2017; 36: 365-79. [PubMed: 28820004](Review of large series of drug induced liver injury in children lists dactinomycin as causing veno-occlusive disease more commonly in children than adults).
- Dactinomycin-induced Hepatic Sinusoidal Obstruction Syndrome Responding to Treatment with N-acetylcysteine.[J Cancer. 2011]Dactinomycin-induced Hepatic Sinusoidal Obstruction Syndrome Responding to Treatment with N-acetylcysteine.Lee AC, Goh PY. J Cancer. 2011; 2:527-31. Epub 2011 Oct 25.
- Methotrexate-induced resistance to dactinomycin in choriocarcinoma.[Cancer. 1988]Methotrexate-induced resistance to dactinomycin in choriocarcinoma.Goto S, Okayama Y, Fan C, Ueda S, Saito M, Furuhashi Y, Ishizuka T, Tomoda Y. Cancer. 1988 Sep 1; 62(5):873-7.
- Treatment of malignant trophoblastic tumors. An analysis of 209 cases.[Chin Med J (Engl). 1991]Treatment of malignant trophoblastic tumors. An analysis of 209 cases.Wang SL, Zhang CS, Peng HQ, Wu KH. Chin Med J (Engl). 1991 Feb; 104(2):156-60.
- Review [Recent advances in the treatment of choriocarcinoma].[Gan To Kagaku Ryoho. 1988]Review [Recent advances in the treatment of choriocarcinoma].Tomoda Y, Ishizuka T, Gotoh S, Furuhashi Y, Inoue T. Gan To Kagaku Ryoho. 1988 Jun; 15(6):1833-9.
- Review [Development of chemotherapy of chorionic tumors].[Nihon Rinsho. 1969]Review [Development of chemotherapy of chorionic tumors].Ishizuka N, Kaseki S. Nihon Rinsho. 1969 Jun; 27(6):1610-7.
- Dactinomycin - LiverToxDactinomycin - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...