NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Cocaine is a benzoid acid ester that that was originally used as a local anesthetic, but is no longer used because of its potent addictive qualities. When given in high doses systemically, cocaine has mood elevating effects that have led to its widescale abuse. High doses of cocaine can be associated with toxic reactions including hyperthermia, rhabdomyolysis, shock and acute liver injury which can be severe and even fatal.
Background
Cocaine (koe kane') is a potent local anesthetic that appears to act by inhibition of voltage-gated sodium channels, increasing the threshold for electric excitability of nerve axons and thus decreasing neuroconduction. In the central nervous system, cocaine appears to block both norepinephrine and serotonin reuptake. High doses produce euphoria followed by withdrawal symptoms, leading to a repeated desire to restart it and great abuse potential. Chronic use is associated with irritability, paranoia, violence and drug seeking behavior. Cocaine is one of the most addictive medications known. For this reason, cocaine is listed as a Schedule I drug, indicating that it has high abuse potential and no current medical usefulness. Cocaine abuse is relatively common; an estimated 600,000 Americans regularly abuse cocaine.
Hepatotoxicity
Cocaine has many serious medical consequences including cardiac arrhythmias, coronary artery spasm and myocardial infarction, cerebrovascular accidents, subarachnoid hemorrhage, seizures, hallucinations, intestinal ischemia, renal infarction, rhabdomyolysis and acute liver injury. Cocaine is a not infrequent cause of sudden “unexplained” death in young adults. Hepatotoxicity usually arises hours to a few days after an acute overdose, generally following or accompanying other major organ involvement. The clinical phenotype of cocaine hepatototoxicity is usually acute hepatic necrosis. Initially, serum aminotransferase and LDH levels are markedly elevated with minimal increase in alkaline phosphatase. The prothrombin time becomes abnormal rapidly and may also reflect disseminated intravascular coagulation (DIC). The serum bilirubin begins to rise after 2 to 3 days. Immunoallergic features and autoantibodies are usually absent. Liver histology usually shows centrolobular (zone 3) necrosis and fatty change, features that resemble ischemic hepatitis or liver injury due to hyperthermia, factors that may partially mediate the hepatotoxic effects of cocaine. In self-limited cases, recovery is rapid and serum aminotransferase levels usually return to normal within 1 to 2 weeks.
Likelihood score: A[HD] (well known cause of acute liver injury, but only when taken as an overdose).
Mechanism of Injury
Cocaine is believed to cause liver injury by conversion to a toxic metabolite as a result of P450 metabolism. In experimental animal models, modulation of P450 activity by inducers, inhibitors or alcohol changes the relative toxicity and pattern of injury from cocaine. In humans, it is less clear whether the hepatic injury is mediated by a toxic metabolite of cocaine as opposed to the direct effects of hyperthermia, anoxia or hepatic ischemia.
Outcome and Management
The liver injury due to the cocaine is usually self-limited and resolves rapidity. However, fatal instances have been reported often due to the other major systemic effects of cocaine overdose (myocardial infarction, stroke, multiorgan failure). There is no specific therapy or antidote for acute cocaine toxicity. Infusions of N-acetylcysteine are often given because of the similarity of the injury to acetaminophen hepatotoxicity.
Drug Class: CNS Stimulants, Agents of Abuse
Other CNS Stimulants: Amphetamines, Armodafinil, Atomoxetine, Methylphenidate, Modafinil
CASE REPORT
Case 1. Acute hepatic necrosis and rhabdomyolysis after cocaine use.
[Modified from: Kanel GC, Cassidy W, Shuster L, Reynolds TB. Cocaine-induced liver cell injury: comparison of morphological features in man and in experimental models. Hepatology 1990; 11: 646-51. PubMed Citation]
A 24 year old man with bizarre behavior after cocaine use was admitted for observation in a jail ward with tachycardia (100/min), fever (100 oF) and tachypnea (30/min). Examination showed small pupils, but was otherwise normal. He had a history of snorting and “free-basing” cocaine and a previous history of injection drug use. Laboratory results showed elevations in CPK, ALT and AST. He was given intravenous hydration, but developed progressive renal failure and was started on dialysis. His liver tests progressively worsened (Table). After three days he became confused, hypoglycemic, and had signs of progressive hepatic failure. The following day he developed respiratory failure followed by hypotension and cardiac arrest not responding to resuscitative measures. On autopsy, the liver showed midzonal and central (zones 2 and 3) coagulative necrosis, with prominent fatty change in surviving periportal hepatocytes and minimal inflammatory change with no cholestasis, fibrosis or bile duct injury.
Key Points
| Medication: | Cocaine (unknown amount) |
|---|---|
| Pattern: | Hepatocellular (R=40) |
| Severity: | 5+ (fatal) |
| Latency: | 1 day |
| Recovery: | None |
| Other medications: | None |
Laboratory Values
| Time After Stopping | ALT (U/L) | CPK (U/L) | Alk P (U/L) | Protime* | Bilirubin (mg/dL) | Other |
|---|---|---|---|---|---|---|
| Arrest for bizarre and combative behavior after cocaine use | ||||||
| 0 | 135 | 617 | ||||
| 1 day | 1760 | 14,240 | 146 | 12% | 1.9 | |
| 2 days | >10,000 | 46,480 | 15% | 3.5 | Renal failure | |
| 4 days | 2,280 | 28,860 | 194 | 9% | 8.7 | Hypoglycemia |
| Death from cardio-respiratory arrest | ||||||
| Normal | <42 | <170 | <90 | >85% | <1.2 | |
* Prothrombin activity as a precent of normal.
Comment
Cocaine is one of the most addictive and dangerous drugs of abuse. This case demonstrates the range of its medical complications, including initial bizarre and combative behavior followed by rhabdomyolysis, hepatic and renal failure, respiratory arrest and cardiovascular collapse. The pattern of liver injury was acute hepatic necrosis with rapid rise and fall of serum aminotransferase levels, little change in alkaline phosphatase and delayed rise in serum bilirubin. Typically, the prothrombin time becomes abnormal early and signs of hepatic encephalopathy can arise at the time that serum bilirubin levels are minimally elevated. Rhabdomyolysis and renal failure are also frequent and the cause of death is usually multiorgan failure rather than acute liver failure per se. Liver histology resembles that of acute ischemic hepatitis and acetaminophen poisoning.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Cocaine – No Commercial Products
DRUG CLASS
Central Nervous System Stimulants
Product labeling at DailyMed, National Library of Medicine, NIH
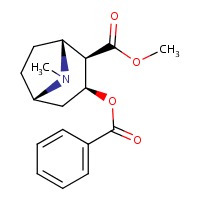
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Cocaine | 50-36-2 | C17-H21-N-O4 |
 |
ANNOTATED BIBLIOGRAPHY
References updated: 26 October 2017
- Zimmerman HJ. Cocaine. Miscellaneous drugs and diagnostic chemicals. In, Zimmerman, HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 712-4.(Expert review of hepatotoxicity published in 1999 mentions that cocaine is known to cause hepatic injury, although this is often eclipsed by cardiac, neurological or muscular damage; it is a dose dependent hepatotoxin in experimental animals).
- Larrey D, Ripault MP. Illegal and recreational compounds. Hepatotoxicity of psychotropic drugs and drugs of abuse. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 456-7.(Review of hepatotoxicity of drugs of abuse mentions that cocaine can cause a severe hepatitis, usually arising within 2 days and associated with marked aminotransferase elevations and other organ failure).
- O’Brien CP. Drug addiction. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 649-59.(Textbook of pharmacology and therapeutics).
- Ehrlich P. [Studies on the effects of cocaine]. Dtsh Med Wochenschr 1890; 16: 716. Not indexed in PubMed.(Early report on effects of cocaine, largely as an anesthetic).
- Marks V, Chapple PA. Hepatic dysfunction in heroin and cocaine users. Br J Addict Alcohol Other Drugs 1967; 62: 189-95. [PubMed: 5231851](Among 89 heroin and cocaine users, 6 were jaundiced and 69% had ALT elevations and marked elevations occurred with relapse in cocaine and heroin use).
- Rubel LR, Ishak KG. The liver in fatal exertional heatstroke. Liver 1983; 3: 249-60. [PubMed: 6672506](Liver histology of 50 cases of fatal heatstroke arising during military training in 17-36 year olds; initially fatty change, vacuolization and congestion, followed by zone 3 coagulative necrosis, cholestasis and microvacuolar fatty change).
- Kloss MW, Rosen GM, Rauckman EJ. Cocaine-mediated hepatotoxicity. A critical review. Biochem Pharmacol 1984; 33: 169-73. [PubMed: 6367747](Discussion of the mechanism of hepatic injury by cocaine in animal model systems).
- Armen R, Kanel GC, Reynolds T. Phencyclidine-induced malignant hyperthermia causing submassive liver necrosis. Am J Med 1984; 7: 167-72. [PubMed: 6741977](3 patients developed agitation, combative behavior and hyperthermia [107-108 oF] shortly after phencyclidine abuse with rise in CPK, ALT and bilirubin [peak levels 15.7-22.5 mg/dL] by day 2; one patient died and 2 recovered with rapid fall of enzymes to normal, liver histology on autopsy showing centrolobular necrosis suggestive of hyperthermia injury).
- Cregler LL, Mark H. Medical complications of cocaine abuse. N Engl J Med 1986; 315: 1495-500. [PubMed: 3537786](Review of the severe medical complications of cocaine abuse including coronary artery spasm, myocardial infarction, rupture of aorta, subarachnoid bleed, stroke, seizures, intestinal and renal infarction; hepatotoxicity not discussed).
- Bates CK. Medical risks of cocaine use. West J Med 1988; 148: 440-4. [PMC free article: PMC1026136] [PubMed: 3291396](Clinical description of cocaine reactions; early, mild effects are behavioral changes and teeth grinding with tachycardia, hypertension and hyperthermia; more severe reactions are then followed by excited delirium, stupor, ventricular arrhythmias and sudden death usually from myocardial infarction or respiratory arrest).
- Perino LE, Warren GH, Levine JS. Cocaine-induced hepatotoxicity in humans. Gastroenterology 1987; 93: 176-80. [PubMed: 3582904](32 year old man developed bizarre behavior and respiratory arrest after snorting cocaine, with AST rising from 620 to 10,700 U/L and bilirubin 0.3 to 4.5 mg/dL and with progressive bradycardia and cardiac arrest within 2 days of admission; autopsy showed mild fatty change and periportal and midzonal necrosis).
- Porter JM, Sussman MS, Rosen GM. Cocaine-induced hepatotoxicity. Hepatology 1988; 8: 1713. [PubMed: 3192186](Commentary on Perino et al [1987]).
- Roth D, Alarcón FJ, Fernandez JA, Preston RA, Bourgoignie JJ. Acute rhabdomyolysis associated with cocaine intoxication. N Engl J Med 1988; 319: 673-7. [PubMed: 3412385](39 patients with acute rhabdomyolysis after cocaine use; 35 were agitated or combative, 4 comatose; CPK levels >10 times ULN in all, muscle tenderness in 20, hyperthermia in 13, acute renal failure in 13, 8 requiring dialysis, disseminated intravascular coagulation in 7, severe liver dysfunction in 13 [ALT mean 5558 U/L, AST 4415 U/L, direct bilirubin 8.7 mg/dL]; 2 died of cardiac arrhythmias and 4 of multiorgan failure).
- Campbell BG. Cocaine abuse with hyperthermia, seizures and fatal complications. Med J Aust 1988; 149: 387-9. [PubMed: 3173196](23 year old woman developed agitation and seizures shortly after cocaine use with fever to 42 oC and subsequent disseminated intravascular coagulation, rhabdomyolysis, acute renal failure, and jaundice [bilirubin initially normal rising to 2.6 mg/dL, AST 99 to 3415 U/L, CK 152 to 10,000 U/L], dying 45 hours after admission).
- Jandreski MA, Bermes EW, Leischner R, Kahn SE. Rhabdomyolysis in a case of free-base cocaine ("crack") overdose. Clin Chem 1989; 35: 1547-9. [PubMed: 2758612](27 year old man developed bizarre behavior followed by combativeness after smoking crack cocaine, with CPK 30 times ULN, ALT and AST >40 times ULN the following day and rise in creatinine, but spontaneous recovery and resolution within one week).
- Bauwens JE, Boggs JM, Hartwell PS. Fatal hyperthermia associated with cocaine use. West J Med 1989; 150; 210-2. [PMC free article: PMC1026353] [PubMed: 2728444](2 men, aged 30 and 38 years old, developed seizures and agitation after cocaine use with temperature of 41.1 and 43 oC with rapid appearance of rhabdomyolysis, renal failure, disseminated intravascular coagulation, liver failure within 1 day and death at 7 days).
- Kanel GC, Cassidy W, Shuster L, Reynolds TB. Cocaine-induced liver cell injury: comparison of morphological features in man and in experimental models. Hepatology 1990; 11: 646-51. [PubMed: 2328957](24 year old man developed bizarre behavior after cocaine use with rhabdomyolysis and subsequent jaundice [bilirubin rising from 1.9 to 8.7 mg/dL, ALT 135 to >10,000 U/L, CPK 617 to 46,480], renal failure, seizures, multiorgan failure and death; autopsy showed zone 2 and 3 hepatic necrosis, periportal fat and minimal inflammation: Case 1).
- Wanless IR, Dore S, Gopinath N, Tan J, Cameron R, Heathcote EJ, Blendis LM, et al. Histopathology of cocaine hepatotoxicity. Report of four patients. Gastroenterology 1990; 98: 497-501. [PubMed: 2153087](Liver histology in 3 women and 1 man with cocaine hepatotoxicity including one fatality; ages 24-28 years, 2 presenting acutely with bizarre behavior followed by rhabdomyolysis and renal and liver failure [bilirubin 3.7 and 4.9 mg/dL, ALT 7300 and 10,200 U/L, Alk P 71 and 123 U/L], one dying on day 6 and one recovering by day 12; two patients had a more subacute presentation several days after exposure [bilirubin normal, ALT 1940 and 435, CPK 6720 and 27,000 U/L], resolving in 7-10 days; histology showed variable amounts of zone 3 coagulative necrosis sometimes extending to zone 2 with fat in remaining hepatocytes, minimal inflammation).
- Gubbins GP, Schiffman RM, Alapati RS, Batra SK. Cocaine-induced hepatonephrotoxicity: a case report. Henry Ford Hosp Med J 1990; 38: 55-6. [PubMed: 2228713](35 year old woman developed dark urine 2 days after smoking crack cocaine [bilirubin 3.0 mg/dL, ALT 9295 U/L, Alk P 131 U/L, CPK 258 U/L, creatinine 5.3 mg/dL], resolving over next two weeks).
- Tabasco-Minguillan J, Novick DM, Kreek MJ. Liver function tests in non-parenteral cocaine users. Drug Alcohol Depend 1990; 26: 169-74. [PubMed: 2242718](56 users of cocaine, but not injection drugs, only 3 had elevated ALT levels [peak 111 U/L] and two of them had hepatitis B suggesting that cocaine use, by itself, does not cause chronic hepatitis or persistent ALT elevations).
- Silva MO, Roth D, Reddy KR, Fernandez JA, Albores-Saavedra J, Schiff ER. Hepatic dysfunction accompanying acute cocaine intoxication. J Hepatol 1991; 12: 312-5. [PubMed: 1940259](Retrospective analysis of 39 patients with cocaine intoxication and rhabdomyolysis; 23 had ALT elevations, 16 were severe; liver injury occurred in all 13 patients with renal failure and in 7 of 8 who died; autopsy showed centrolobular necrosis, compatible with shock or hyperthermia).
- Mallat A, Dhumeaux D. Cocaine and the liver. J Hepatol 1991; 12: 275-8. [PubMed: 1940255](Editorial accompanying article by Silva [1991]).
- Saltzman JR, Johnston DE. Sickle cell crisis and cocaine hepatotoxicity. Am J Gastroenterol. 1992; 87: 1661-4. [PubMed: 1442696](33 year old man with sickle cell anemia and multiple crises, presented with rise in bilirubin [6.2 at baseline to 37.5 mg/dL], ALT [24 to 726 U/L] and Alk P [152 to 370 U/L] after cocaine use; also taking amoxicillin/clavulanate).
- Peyrière H, Mauboussin JM. Cocaine-induced acute cytologic hepatitis in HIV-infected patients with nonactive viral hepatitis. Ann Intern Med 2000; 132: 1010-1. [PubMed: 10858171](3 patients with HIV/HBV or HCV coinfection who had rises in ALT levels [baseline of 7-30 rising to 340-1669 U/L], without jaundice or rise in Alk P a few days after intranasal cocaine use ).
- Campos Franco J, Martínez Rey C, Pérez Becerra E, González Quintela A. [Cocaine related fulminant liver failure]. An Med Interna 2002; 19: 365-7. [PubMed: 12224146](23 year old woman presented with confusion 10 hours after cocaine use [bilirubin 1.2 mg/dL, ALT 1031 U/L, Alk P 103 U/L], worsening for 6 days and then resolving rapidly over next 10 days; biopsy showed centrolobular coagulative necrosis with minimal inflammation).
- Hurtova M, Duclos-Vallée JC, Saliba F, Emile JF, Bemelmans M, Castaing D, Samuel D. Liver transplantation for fulminant hepatic failure due to cocaine intoxication in an alcoholic hepatitis C virus-infected patient. Transplantation 2002; 73: 157-8. [PubMed: 11792999](33 year old man with chronic hepatitis C presented with acute liver failure shortly after iv cocaine use [ALT 30 times ULN, CPK 27,000 U/L, prothrombin index 9%], undergoing liver transplantation; explant showing centrolobular coagulative necrosis and marked steatosis).
- Kramer L, Bauer E, Schenk P, Steininger R, Vigl M, Mallek R. Successful treatment of refractory cerebral oedema in ecstasy/cocaine-induced fulminant hepatic failure using a new high-efficacy liver detoxification device (FPSA-Prometheus). Wien Klin Wochenschr 2003; 115: 599-603. [PubMed: 14531175](27 year old man developed coma within hours of injecting heroin and cocaine and taking 300 mg of MDMA with evidence of multiorgan failure and rhabdomyolysis [bilirubin 1.1 rising to 9.5 mg/dL, ALT 5870 U/L, LDH 11,030 U/L, INR 1.6 rising to 3.2] and was treated with a fractionated plasma separation and adsorption device, with ultimate resolution within 3 weeks).
- Balaguer F, Fernández J, Lozano M, Miquel R, Mas A. Cocaine-induced acute hepatitis and thrombotic microangiopathy. JAMA 2005; 293: 797-8. [PubMed: 15713768](22 year old woman developed jaundice a few days after cocaine use [bilirubin 12.0 rising to 71.4 mg/dL, ALT 1305 U/L, Alk P 308 U/L], with respiratory and renal failure and hemolytic anemia but eventual resolution).
- Abd El-Rahman AM, Ammar H. Cocaine-induced acute hepatitis and thrombotic microangiopathy. JAMA 2005; 293: 2715; author reply 2715-6. [PubMed: 15941798](Letter in response to Balaguer [2005] discussing use of fresh frozen plasma exchange rather than albumin).
- Jiménez Pérez M, Marín García D, Santaella Leiva I, Olmedo García R. [Cocaine-induced hepatotoxicity]. Med Clin (Barc) 2008; 130: 279. Spanish. [PubMed: 18355433](42 year old man became semicomatose 10 hours after inhaling cocaine [bilirubin 1.9 mg/dL, ALT 2673 U/L, GGT 244 U/L, creatinine 5 mg/dL], with rhabdomyolysis and renal failure requiring dialysis, but ultimate recovery and near normal liver enzymes 8 days after admission).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J; Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008; 135: 1924-34. PubMed Citation . [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, 3 cases were attributed to atomoxetine and one to methylphenidate, but none to cocaine or ecstasy).
- Reuben A, Koch DG, Lee WM; Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology 2010; 52: 2065-76. PubMed Citation . [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, including one attributed to cocaine and one to ecstasy).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, Presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 2013; 144: 1419-25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, but none were attributed to cocaine or amphetamine use).
- Giuliani E, Albertini G, Vaccari C, Manenti A, Barbieri A. Multi-organ failure following severe cocaine-tetramisole intoxication in a body-packer. Anaesth Intensive Care. 2012; 40: 562-4. [PubMed: 22577932](51 year old woman, who had swallowed sealed packets of cocaine to smuggle them into Italy, had sudden onset of seizures followed by coma and cardiac arrest; after resuscitation, ALT levels rose starting on day 2 to a peak of 6000 U/L on day 4 and rapid recovery and discharge on day 7).
- Zimmerman JL. Cocaine intoxication. Crit Care Clin 2012; 28: 517-26. [PubMed: 22998988](Review of the major complications of cocaine overdose including cardiac, neurologic, respiratory and renal; no discussion of hepatotoxicity).
- Trabulo D, Marques S, Pedroso E. Cocaine capsules in the colon: the internal concealment of illicit drugs. J Gastrointestin Liver Dis 2015; 24: 9. [PubMed: 25822426](26 year old man was arrested and jailed for drug smuggling and developed fever and abdominal pain 2 days later, X-rays showing "nodules" in colon which were successfully removed by enemas; no follow up provided).
- Guollo F, Narciso-Schiavon JL, Barotto AM, Zannin M, Schiavon LL. Significance of alanine aminotransferase levels in patients admitted for cocaine intoxication. J Clin Gastroenterol 2015; 49: 250-5. [PubMed: 24518798](Retrospective analysis of 93 patients wtih cocaine intoxication, 5 of whom had marked ALT elevations [>20 times ULN], all were critically ill and had rhabdomyolysis, two had renal failure and one died).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, no cases were attributed to cocaine or other illicit drugs).
- Review Cocaine-associated rhabdomyolysis and excited delirium: different stages of the same syndrome.[Am J Forensic Med Pathol. 1999]Review Cocaine-associated rhabdomyolysis and excited delirium: different stages of the same syndrome.Ruttenber AJ, McAnally HB, Wetli CV. Am J Forensic Med Pathol. 1999 Jun; 20(2):120-7.
- Cocaine intoxication: hyperpyrexia, rhabdomyolysis and acute renal failure.[J Toxicol Clin Toxicol. 1987]Cocaine intoxication: hyperpyrexia, rhabdomyolysis and acute renal failure.Merigian KS, Roberts JR. J Toxicol Clin Toxicol. 1987; 25(1-2):135-48.
- Review Nephrotoxic effects of common and emerging drugs of abuse.[Clin J Am Soc Nephrol. 2014]Review Nephrotoxic effects of common and emerging drugs of abuse.Pendergraft WF 3rd, Herlitz LC, Thornley-Brown D, Rosner M, Niles JL. Clin J Am Soc Nephrol. 2014 Nov 7; 9(11):1996-2005. Epub 2014 Jul 17.
- Rhabdomyolysis and acute renal failure associated with cocaine abuse.[J Toxicol Clin Toxicol. 1990]Rhabdomyolysis and acute renal failure associated with cocaine abuse.Singhal PC, Rubin RB, Peters A, Santiago A, Neugarten J. J Toxicol Clin Toxicol. 1990; 28(3):321-30.
- Rhabdomyolysis and hyperthermia after cocaine abuse: a variant of the neuroleptic malignant syndrome?[Acta Neurol Scand. 1995]Rhabdomyolysis and hyperthermia after cocaine abuse: a variant of the neuroleptic malignant syndrome?Daras M, Kakkouras L, Tuchman AJ, Koppel BS. Acta Neurol Scand. 1995 Aug; 92(2):161-5.
- Cocaine - LiverToxCocaine - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...