NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Acetazolamide and methazolamide are carbonic anhydrase inhibitors used as diuretics and in the therapy of glaucoma. Both acetazolamide and methazolamide have been linked to rare cases of clinically apparent drug induced liver disease.
Background
Acetazolamide (a seet" a zol' a mide) and methazolamide (meth" a zol' a mide) are inhibitors of carbonic anhydrase, an enzyme that converts carbon dioxide and water to carbonic acid. Inhibition of this enzyme in the kidney causes an alkalization of the urine and diuresis. In the eye, inhibition of carbonic anhydrase causes a decrease in intraocular pressure making these agents valuable in the treatment of glaucoma. The effects of acetazolamide on acid-base status (causing a mild metabolic acidosis) are also of potential value in managing other conditions including epilepsy, sleep apnea, and acute mountain sickness. Acetazolamide was approved for use in the United States in 1986 for treatment of glaucoma and as a diuretic to prevent or ameliorate acute mountain sickness. Acetazolamide is available in 125 and 250 mg tablets in generic forms and under the brand name of Diamox. Acetazolamide is also available in extended release forms (capsules of 500 mg) and as powder for injection. The recommended dose and regimen of acetazolamide varies by indication, but for chronic use in adults the typical dose is 250 to 1,000 mg daily in divided doses.
Methazolamide was approved for use in the United States in 1959 for the treatment of glaucoma. Methazolamide is available as tablets of 25 and 50 mg in generic forms and under the trade name Neptazane. Typical doses of methazolamide in adults with glaucoma are 50 to 100 mg two to three times daily.
The common side effects of acetazolamide and methazolamide are change in taste, numbness and tingling in fingers and toes, blurred vision, tinnitus, dizziness, decrease in hearing, polyuria, nausea, diarrhea, fatigue, and headache. Methazolamide and acetazolamide have similar chemical structures and are related to the sulfonamides and can cause allergic reactions including anaphylaxis, rash, erythema multiforme, and Stevens Johnson syndrome.
Hepatotoxicity
Idiosyncratic, clinically apparent liver injury from acetazolamide and methazolamide is rare, but several instances have been reported as isolated case reports. Acetazolamide is a sulfonamide and cross reactivity to sulfonamide reactions have been reported. The liver injury typically arises after a few days to weeks of therapy and the pattern of serum enzyme elevations is usually hepatocellular or mixed. Immunoallergic features (rash, fever, eosinophilia) are common, but autoantibody formation is not. Both acetazolamide and methazolamide have been linked to Stevens Johnson syndrome and a genetic association has been made with HLA-B*59:01. Hepatic involvement and jaundice can occur in cases of Stevens Johnson syndrome but is generally overshadowed by the severe cutaneous reaction.
Likelihood score: D (possible but rare cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism of acetazolamide hepatic injury is believed to be due to hypersensitivity with shared pathogenesis with the sulfonamides.
Outcome and Management
Severity ranges from mild, asymptomatic elevations in serum enzymes, to clinically apparent acute hepatitis to severe injury with acute liver failure or prolonged jaundice. Corticosteroids are often used in patients with other features of hypersensitivity, but their role in altering the ultimate outcome of the injury is unproven. Rechallenge should be avoided and patients should be warned to avoid sulfa-containing drugs in the future.
Drug Class: Diuretics
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Acetazolamide – Generic, Diamox®
Methazolamide – Generic, Neptazane®
DRUG CLASS
Diuretics
COMPLETE LABELING (Acetazolamide)
COMPLETE LABELING (Methazolamide)
Product labeling at DailyMed, National Library of Medicine, NIH
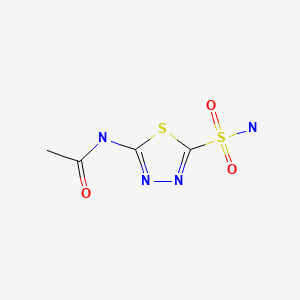
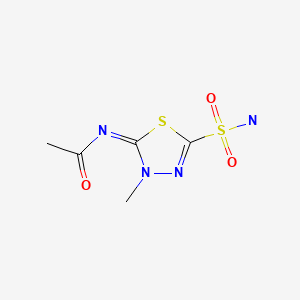
CHEMICAL FORMULAS AND STRUCTURES
ANNOTATED BIBLIOGRAPHY
References updated: 13 October 2021
- Zimmerman HJ. Diuretic drugs. Drugs used in cardiovascular disease. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 662-4.(Expert review of hepatotoxicity of diuretics published in 1999 mentions that clinically apparent liver injury due to diuretics is rare; acetazolamide and methazolamide have been linked to several instances of cholestatic or mixed hepatitis, perhaps due to hypersensitivity).
- De Marzio DH, Navarro VJ. Hepatotoxicity of cardiovascular and antidiabetic drugs. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 519-40.(Review of hepatotoxicity of cardiovascular agents, mentions that diuretics can rarely cause cholestatic hepatitis).
- Jackson EK. Drugs affecting renal excretory function. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 445-70.(Textbook of pharmacology and therapeutics).
- Kristinsson A. Fatal reaction to acetazolamide. Br J Ophthalmol. 1967;51:348–9. [PMC free article: PMC506396] [PubMed: 6022777](34 year old man with glaucoma developed fatigue, nausea and generalized rash followed by delirium 26 days after starting acetazolamide [bilirubin 10.9 mg/dL, ALT 180 U/L, Alk P 3 times ULN], with progressive hepatic failure and death within 24 hours).
- Gangitano JL, Foster SH, Contro RM. Nonfatal methazolamide-induced aplastic anemia. Am J Ophthalmol. 1978;86:138–9. [PubMed: 677225](83 year old man developed aplastic anemia 3 months after starting methazolamide for glaucoma; no mention of liver test abnormalities).
- Werblin TP, Pollack IP, Liss RA. Aplastic anemia and agranulocytosis in patients using methazolamide for glaucoma. JAMA. 1979;241:2817–8. [PubMed: 448845](Two cases of aplastic anemia, 1 of which occurred after starting methazolamide; no mention of liver injury).
- Krivoy N, Ben-Arich Y, Carter A, Alroy G. Methazolamide induced hepatitis and pure RBC aplasia. Arch Intern Med. 1981;141:1229–30. [PubMed: 7196210](69 year old man with glaucoma developed rash 3 weeks after starting methazolamide with fever, diarrhea, pruritus and jaundice [bilirubin 24 mg/dL, AST 72 U/L, Alk P 865 U/L], developing anemia during recovery, resolving fully after prednisone therapy).
- Sud RN, Grewal SS. Stevens Johnson syndrome due to Diamox. Indian J Ophthalmol. 1981;29:101–3. [PubMed: 7327685](Short report of Stevens Johnson syndrome in 8 Indian patients with glaucoma treated with acetazolamide; all recovered, no mention of hepatic injury or jaundice).
- Flach AJ, Smith RE, Fraunfelder FT. Stevens-Johnson syndrome associated with methazolamide treatment reported in two Japanese American women. Ophthalmology. 1995;102:1677–80. [PubMed: 9098261](Two cases of Stevens Johnson syndrome in Japanese women, ages 65 and 27 years, with onset of rash and fever within 10 days of starting methazolamide for glaucoma with long term skin and corneal sequelae; no mention of ALT elevations or liver injury).
- Shirato S, Kagaya F, Suzuki Y, Joukou S. Stevens-Johnson syndrome induced by methazolamide treatment. Arch Ophthalmol. 1997;115:550–3. [PubMed: 9109770](Four cases of Stevens Johnson syndrome in 3 Japanese women and 1 man, ages 30 to 47 years, with onset of fever and rash 2-8 weeks after starting methazolamide for glaucoma; all recovered; no mention of hepatic injury).
- Russo MW, Galanko JA, Shrestha R, Fried MW, Watkins P. Liver transplantation for acute liver failure from drug-induced liver injury in the United States. Liver Transpl. 2004;10:1018–23. [PubMed: 15390328](Among ~50,000 liver transplants reported to UNOS between 1990 and 2002, 137 [0.5%] were done for idiosyncratic drug induced acute liver failure, none were attributed to a diuretic).
- Andrade RJ, Lucena MI, Fernández MC, Pelaez G, Pachkoria K, García-Ruiz E, García-Muñoz B, et al. Drug-induced liver injury: an analysis of 461 incidences submitted to the Spanish Registry over a 10-year period. Gastroenterology. 2005;129:512–21. [PubMed: 16083708](Reports of drug induced liver injury to a Spanish network found 570 cases; diuretics not mentioned as cause).
- Björnsson E, Olsson R. Suspected drug-induced liver fatalities reported to the WHO database. Dig Liver Dis. 2006;38:33–8. [PubMed: 16054882](Survey of drug induced liver fatalities reported to WHO database between 1968-2003 revealed 4690 reports [89% from the US]; no diuretic found in the 20 most commonly implicated agents).
- Ogasawara K, Tomitsuka N, Kobayashi M, Komoribayashi N, Fukuda T, Saitoh H, Inoue T, et al. Stevens-Johnson syndrome associated with intravenous acetazolamide administration for evaluation of cerebrovascular reactivity. Case report. Neurol Med Chir (Tokyo). 2006;46:161–3. [PubMed: 16565588](62 year old Japanese man given single intravenous injection of acetazolamide developed Stevens Johnson syndrome 3 days later responding to prednisolone; no mention of ALT levels or jaundice).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, no case was attributed to a diuretic).
- Drugs for hypertension. Treat Guidel Med Lett. 2009;7:1–10. [PubMed: 19107095](Brief overview of currently available drugs for hypertension with guidelines on their use and information on prices and toxicities).
- Devarbhavi H, Dierkhising R, Kremers WK, Sandeep MS, Karanth D, Adarsh CK. Single-center experience with drug-induced liver injury from India: causes, outcome, prognosis, and predictors of mortality. Am J Gastroenterol. 2010;105:2396–404. [PubMed: 20648003](Among 313 cases of drug induced liver injury seen over a 12 year period at a large hospital in Bangalore, India, none were attributed to a diuretic).
- Ferrajolo C, Capuano A, Verhamme KM, Schuemie M, Rossi F, Stricker BH, Sturkenboom MC. Drug-induced hepatic injury in children: a case/non-case study of suspected adverse drug reactions in VigiBase. Br J Clin Pharmacol. 2010;70:721–8. [PMC free article: PMC2997312] [PubMed: 21039766](Among 624,673 adverse event reports in children between 2000 and 2006 in the WHO VigiBase, no diuretic was mentioned among the 30 most common causes of liver injury).
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, of which none were attributed to a diuretic).
- Kim SH, Kim M, Lee KW, Kim SH, Kang HR, Park HW, Jee YK. HLA-B*5901 is strongly associated with methazolamide-induced Stevens-Johnson syndrome/toxic epidermal necrolysis. Pharmacogenomics. 2010;11:879–84. [PubMed: 20504258](Among 5 Korean patients with methazolamide induced Stevens Johnson syndrome, all had HLA-B*5901 vs 4.1% of general population in Korea; also linked to Cw*0102 and A*2402).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, none of which were attributed to a diuretic).
- Başar Ö, Başar N, Tuna Y, Yüksel H, Çoban Ş. Acetazolamide induced severe hepatotoxicity. Wien Klin Wochenschr. 2013;125:223–4. [PubMed: 23519540](44 year old woman developed jaundice 2 weeks after starting acetazolamide [bilirubin 8.9 mg/dL, ALT 492 U/L, Alk P 348 U/L, INR 1.39], worsening for 4 days and then resolving within 21 days of stopping).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America: an analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Among 176 reports of drug induced liver injury from Latin America published between 1996 and 2012, none were attributed to a diuretic).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, none were attributed to a diuretic).
- Drugs for hypertension. Med Lett Drugs Ther. 2020;62(1598):73–80. [PubMed: 32555118](Concise summary of efficacy, safety and costs of drug therapy of hypertension including the diuretics, focusing upon relative usefulness; no mention of hepatic adverse events).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- The carbonic anhydrase inhibitors methazolamide and acetazolamide have different effects on the hypoxic ventilatory response in the anaesthetized cat.[J Physiol. 2006]The carbonic anhydrase inhibitors methazolamide and acetazolamide have different effects on the hypoxic ventilatory response in the anaesthetized cat.Teppema LJ, Bijl H, Mousavi Gourabi B, Dahan A. J Physiol. 2006 Jul 15; 574(Pt 2):565-72. Epub 2006 May 4.
- Liver carbonic anhydrase and urea synthesis. The effect of diuretics.[Biochem Pharmacol. 1986]Liver carbonic anhydrase and urea synthesis. The effect of diuretics.Häussinger D, Kaiser S, Stehle T, Gerok W. Biochem Pharmacol. 1986 Oct 1; 35(19):3317-22.
- Intraocular pressure effects of carbonic anhydrase inhibitors in primary open-angle glaucoma.[Am J Ophthalmol. 1989]Intraocular pressure effects of carbonic anhydrase inhibitors in primary open-angle glaucoma.Lichter PR, Musch DC, Medzihradsky F, Standardi CL. Am J Ophthalmol. 1989 Jan 15; 107(1):11-7.
- Review Drug interaction considerations in the therapeutic use of carbonic anhydrase inhibitors.[Expert Opin Drug Metab Toxicol...]Review Drug interaction considerations in the therapeutic use of carbonic anhydrase inhibitors.Supuran CT. Expert Opin Drug Metab Toxicol. 2016; 12(4):423-31. Epub 2016 Mar 3.
- Review Glaucoma and the applications of carbonic anhydrase inhibitors.[Subcell Biochem. 2014]Review Glaucoma and the applications of carbonic anhydrase inhibitors.Scozzafava A, Supuran CT. Subcell Biochem. 2014; 75:349-59.
- Carbonic Anhydrase Inhibitors - LiverToxCarbonic Anhydrase Inhibitors - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...