NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Candesartan is an angiotensin II receptor blocker used widely in the therapy of hypertension and heart failure. Candesartan is associated with a low rate of transient serum aminotransferase elevations and has been linked to rare instances of acute liver injury.
Background
Candesartan (kan" de sar' tan) is an angiotensin II receptor blocker (ARB) that is widely used alone or in combination with other agents as therapy of hypertension and heart failure. Candesartan inhibits the renin-angiotensin system by blocking the angiotensin II type 1 receptor (AT1), which prevents the vasoconstriction and volume expansion induced by circulating angiotensin II, accounting for its antihypertensive activity. Candesartan was approved for use in the United States in 1998 and is available in 4, 8, 16 and 32 mg tablets generically and under the trade name Atacand. Current indications include treatment of hypertension (usually in combination with other agents) and to prevent cardiovascular events and death in patients with chronic heart failure. The typical dose of candesartan in adults is 16 to 32 mg once daily, and it is used long term. Candesartan is also available in fixed combinations with hydrochlorothiazide (Atacand HCT and others). Side effects of candesartan are uncommon, but may include headache, dizziness, fatigue, cough, gastrointestinal upset and fetal toxicity. Many ARBs, but not specifically candesartan, have been linked to cases of a severe sprue-like enteropathy that presents with severe diarrhea and weight loss and villous flattening and atrophy on intestinal biopsy arising after months or years of ARB use. The enteropathy resembles celiac disease but does not repond to a gluten-free diet, but resolves promptly with stopping the angiotensin receptor blocker.
Hepatotoxicity
Candesartan has been associated with a low rate of serum aminotransferase elevations (<1%) that in controlled trials was no higher than with placebo therapy. These elevations were transient and rarely required dose modification. Rare instances of clinically apparent acute liver injury have been reported in association with candesartan therapy. The onset is usually within 1 to 8 weeks of starting therapy and the serum enzyme pattern can be either hepatocellular or cholestatic with an acute hepatitis- or cholestatic hepatitis-like clinical syndrome. In some instances, cholestasis can be prolonged and relapsing, but candesartan therapy has not been associated with vanishing bile duct syndrome or chronic liver injury. Immunoallergic manifestations (rash, fever, eosinophilia) are not common, nor is autoantibody formation.
Likelihood score: C (Probable cause of rare instances of clinically apparent liver injury).
Mechanism of Injury
The cause of the minor serum aminotransferase elevations and the acute liver injury associated with candesartan is not known, but resembles idiosyncratic liver injury due to a hypersensitivity reaction. Candesartan has minor liver metabolism through the cytochrome P450 system (CYP 2C9) and has minimal drug-drug interactions.
Outcome and Management
The instances of acute liver injury reported with candesartan use have been self limited and have not resulted in acute liver failure or chronic liver injury. While corticosteroids have been used in cases of severe cholestasis due to ARBs, their efficacy has not been shown and their use is best avoided. Patients with candesartan induced acute liver injury should probably avoid use of other ARBs, although cross sensitivity to liver injury among the members of this class of agents has not been shown.
References on the safety and potential hepatotoxicity of candesartan are given in the Overview section on the angiotensin II receptor antagonists.
Drug Class: Antihypertensive Agents, Angiotensin II Receptor Antagonists
Other Drugs in the Subclass, Angiotensin II Receptor Antagonists: Azilsartan, Eprosartan, Irbesartan, Losartan, Olmesartan, Telmisartan, Valsartan
CASE REPORT
Case 1. Severe hepatitis attributed to candesartan.
[Modified from: Basile G, Villari D, Gangemi S, Ferrara T, Accetta MG, Nicita-Mauro V. Candesartan cilexetil-induced severe hepatotoxicity. J Clin Gastroenterol 2003; 36: 273-5. PubMed Citation]
A 61 year old woman with hypertension started therapy with candesartan cilexetil (16 mg daily) and developed fever, anorexia, nausea, abdominal pain and jaundice approximately 4 weeks later. She had no history of liver disease, alcohol abuse, risk factors for viral hepatitis or previous serious drug reactions. On examination, she had jaundice and low grade fever (37.8 oC). Laboratory tests showed marked elevations in serum bilirubin (27.2 mg/dL) and serum aminotransferase levels (ALT 918 U/L, AST 1367 U/L) with minimal increase in alkaline phosphatase (142 U/L), LDH (700 U/L: normal <460 U/L) and GGT (49 U/L) (Table). The prothrombin index was reduced at 52% (normal 70% to 120%). Tests for hepatitis A, B and C were negative and antinuclear antibody titers were minimally increased (1:40). Ultrasound and CT of the abdomen showed mild hepatomegaly and minimal ascites without evidence of biliary obstruction. A liver biopsy showed acute hepatocellular necrosis and inflammation but also cholestasis, ductopenia and biliary epithelial injury. There was mild fibrosis. Because of rising levels of serum bilirubin (peak 46.8 mg/dL), she was treated with a seven week course of methylprednisolone (40 mg/day for 3 weeks, 20 mg/day for 2 weeks, and 8 mg/day for two weeks). There was a gradual improvement in the patient’s condition and she was discharged after 8 weeks in the hospital. One month later, all liver tests were repeated and were normal.
Key Points
| Medication: | Candesartan (16 mg daily) |
|---|---|
| Pattern: | Hepatocellular (R=13) |
| Severity: | 4+ (jaundice, prothrombin time prolongation and ascites) |
| Latency: | 4 weeks |
| Recovery: | 8-12 weeks |
| Other medications: | None mentioned |
Laboratory Values
Comment
The patient developed an acute hepatitis-like clinical syndrome one month after starting candesartan for hypertension. No other cause of acute liver injury was identified, and a liver biopsy showed changes that were compatible with drug induced liver disease (mixed hepatocellular and biliary injury). Corticosteroids were given because of the severity of the injury and recovery, while delayed, was ultimately complete within 8 to 12 weeks of onset. Whether the corticosteroids prompted or sped recovery is uncertain, but importantly, the methylprednisone dose was quickly lowered and stopped. Clinically apparent acute liver injury from angiotensin receptor antagonists is exceedingly rare, but the timing of onset and recovery and liver biopsy findings in this case were convincing. In view of the severity of the injury and the availability of other medications to treat hypertension, rechallenge with candesartan is not warranted.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Candesartan – Atacand®
DRUG CLASS
Angiotensin II Receptor Antagonists
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Candesartan | 139481-59-7 | C24-H20-N6-O3 |
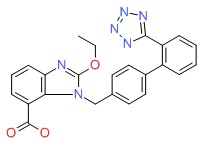 |
- PubChem SubstanceRelated PubChem Substances
- Review Angiotensin II Receptor Antagonists.[LiverTox: Clinical and Researc...]Review Angiotensin II Receptor Antagonists.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Candesartan cilexetil: an angiotensin II receptor blocker.[Ann Pharmacother. 1999]Review Candesartan cilexetil: an angiotensin II receptor blocker.Stoukides CA, McVoy HJ, Kaul AF. Ann Pharmacother. 1999 Dec; 33(12):1287-98.
- Candesartan, rather than losartan, improves motor dysfunction in thioacetamide-induced chronic liver failure in rats.[Braz J Med Biol Res. 2017]Candesartan, rather than losartan, improves motor dysfunction in thioacetamide-induced chronic liver failure in rats.Murad HA, Gazzaz ZJ, Ali SS, Ibraheem MS. Braz J Med Biol Res. 2017 Sep 21; 50(11):e6665. Epub 2017 Sep 21.
- Combination treatment with a calcium channel blocker and an angiotensin blocker in a rat systolic heart failure model with hypertension.[Hypertens Res. 2002]Combination treatment with a calcium channel blocker and an angiotensin blocker in a rat systolic heart failure model with hypertension.Namba M, Kim S, Zhan Y, Nakao T, Iwao H. Hypertens Res. 2002 May; 25(3):461-6.
- Review Losartan.[LiverTox: Clinical and Researc...]Review Losartan.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Candesartan - LiverToxCandesartan - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...