NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Artemisinin is an ancient Chinese herbal therapy for malarial fevers which has been recently found to have potent activity against many forms of malarial organisms, including chloroquine-resistant Plasmodium falciparum. Several artemisinin derivatives have been developed for clinical use in prevention and treatment of malaria, some of which have been linked to rare instances of acute liver injury.
Background
The artemisinins (ar tem' is in in), including artesumate, arteeter, artemether, artemisinin, and dihydroartemisinin, are derivatives of the Chinese herb known as "qing hao" or sweet wormwood plant (Artemisia annua). The artemisinins have antimalarial activity in vitro and in vivo and are believed to act by release of free radicals into the parasite vacuoles. Artemisinin derivatives are currently the most active antimalarial drugs available and have been introduced around the world as an integral part of therapy of active malaria, always in combination with other antimalarials to prevent resistance such as amodiaquine, lumefantrine and mefloquine. Several oral and parenteral formulations of artemisinin derivatives are available worldwide. In the United States, the combination of artemether (20 mg) and lumefantrine (120 mg) was approved for therapy of P. falciparum malaria in 2009 under the brand name Coartem. The recommended dose for adults is 4 tablets twice daily for 3 days (6 doses). Artesunate (Adamsunate) is also available on a named-patient basis from the Centers for Disease Control and Prevention (CDC) Malaria Hotline (770-488-7788, M-F, 8 am to 4:30 pm, Eastern time). General recommendations on use of artemisinin and other antimalarial agents are available at the CDC website: http://www.cdc.gov/malaria/. Common side effects of artesunate include nausea, vomiting, anorexia, and dizziness. Potentially severe adverse events include prolongation of the QTc interval and cardiac arrhythmias.
Hepatotoxicity
Artemisinin derivatives have been associated with a low rate of serum aminotransferase elevations (1% to 4%) that are generally asymptomatic, mild-to-moderate and self-limited, often resolving even with continuing therapy. In most studies, the rate of serum ALT elevations during artemisinin therapy was similar to that of patients on comparator agents. Importantly, there have been increasing numbers of reports of idiosyncratic acute liver injury in patients taking artemisinin derivatives. Complicating the interpretation of these reports, however, is that most severe cases of liver injury occurred in patients who were also receiving other antimalarial agents, some of which are known to be hepatotoxic (amodiaquine, sulfamethoxazole, sulfadiazine/pyrimethamine). The onset of injury was usually within a few days to weeks of starting artemisinin, and the pattern of serum enzyme elevations was typically hepatocellular. Features of hypersensitivity such as rash, fever and eosinophilia were uncommon and autoantibodies have not been described. Symptoms can resemble those of acute viral hepatitis and the hepatitis can be severe, and several fatal instances or cases requiring emergency liver transplantation have been reported. Nevertheless, clinically apparent liver injury due to artemisinin derivatives is very rare and was not reported in several large clinical trials of malaria treatment. Most published reports of hepatotoxicity of artemisinin were linked to use of herbal supplements containing artemisinin and with extended treatment.
Liklihood score: D (possible rare cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism by which artemisinin derivatives cause liver injury is unknown. Clinical factors and testing for serum antibodies suggest an idiosyncratic immunological reaction to a hepatic metabolite may be responsible. Artemisinin derivatives are extensively metabolized by the liver (primarily via CYP 3A4) and are prone drug-drug interactions if given with strong CYP 3A4 inducers such as rifampin, phenytoin or St. John's wort or inhibitors such as intraconazole or ritonavir.
Outcome and Management
There does not seem to be cross reactivity to hepatic injury of the artemisinin derivatives with other antimalarial agents, but it is likely that sensitivity will be shared among the various artemisinin.
Drug Class: Antimalarial Agents
CASE REPORT
Case 1. Acute liver injury due to artemisinin exposure.
[Modified from: Centers for Disease Control and Prevention (CDC). Hepatitis temporally associated with an herbal supplement containing artemisinin – Washington, 2008. MMWR Morb Mortal Wkly Rep 2009; 58: 854-6. PubMed Citation]
A 52 year old man with irritable bowel syndrome was treated with an herbal powder that contained artemisinin and developed fatigue and dark urine 10 days later. He had no history of liver disease, alcohol abuse, recent travel or risk factors for viral hepatitis. His only other medication was an occasional acetaminophen tablet. Analysis of the powder indicated that he had been taking the equivalent of 600 mg of artemisinin daily. Physical examination revealed jaundice and mild abdominal tenderness without fever or rash. Laboratory testing suggested a mild hepatitis (Table). His serum enzymes had been normal on routine testing five months earlier. Tests for hepatitis A, B and C were negative. Acetaminophen was not detected. He was monitored on no therapy and improved rapidly. Symptoms had resolved and all tests were negative two weeks later.
Key Points
| Medication: | Herbal powder containing artemisinin |
|---|---|
| Pattern: | Hepatocellular (R=9.6) |
| Severity: | 3+ (jaundice, hospitalization) |
| Latency: | 2 weeks |
| Recovery: | 2 weeks |
| Other medications: | Occasional acetaminophen |
Laboratory Values
Comment
Cases of artemisinin hepatotoxicity have been characterized by rapid onset within a few days to 3 weeks of starting therapy and a hepatocellular pattern of serum enzyme elevations, but without signs of hypersensitivity such as rash, fever or eosinophilia. The cause of the injury is unknown, but it has many features of hypersensitivity such as short latency and occurrence upon reexposure. Fatal instances have been reported. The current case was distinctive in that the patient was taking artemesinin not for malaria, but as a part of an herbal medication for gastrointestinal complaints. Artemisinin was taken in very high doses and for a longer period than is typical for acute malaria (active therapy of which is typically for 3 days).
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Artemisinin Derivatives (artemether, lumefantrine) – Coartem®
DRUG CLASS
Antimalarial Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Artemisinin | 63968-64-9 | C15-H22-O5 |
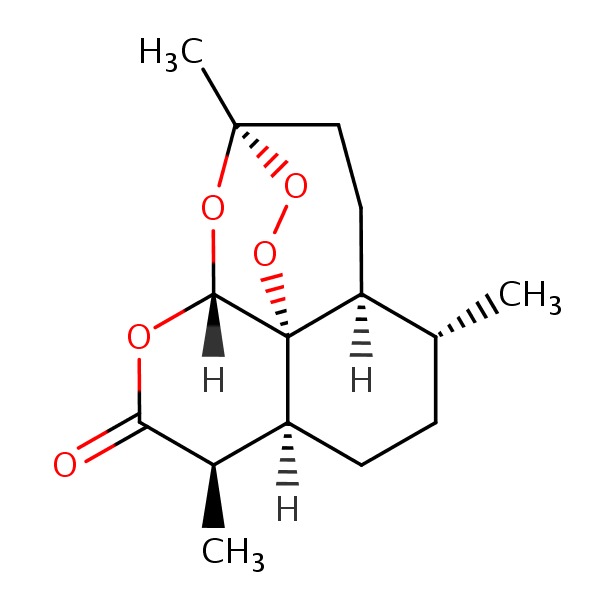 |
ANNOTATED BIBLIOGRAPHY
References updated: 08 February 2017
- Zimmerman HJ. Antiprotozoal agents. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 623-5.(Expert review of hepatotoxicity published in 1999; before the availability of artemisinin derivatives).
- Vinetz JM, Clain J, Bounkeua V, Eastman RT, Fidock D. Chemotherapy of malaria.l In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman.s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1383-418.(Textbook of pharmacology and therapeutics).
- Ribeiro IR, Olliaro P. Safety of artemisinin and its derivatives. A review of published and unpublished clinical trials. Med Trop (Mars) 1998; 58 (Suppl 3): 50-3. [PubMed: 10212898](Systematic review of 108 studies of artemisinin derivatives enrolling 9241 patients found low rate of adverse events, elevated ALT levels occurred in 36 patients [0.9%], but no severe adverse events were attributed to drug).
- Orrell C, Taylor WR, Olliaro P. Acute asymptomatic hepatitis in a healthy normal volunteer exposed to 2 oral doses of amodiaquine and artesunate. Trans R Soc Trop Med Hyg 2001; 95: 517-8. [PubMed: 11706664](In a single dose crossover study in 15 volunteers, one developed rise in ALT from normal to peak of 483 U/L 6 weeks after dosing with amodiaquine and artesunate without symptoms or bilirubin rise, resolving in 4-8 weeks).
- Taylor WR, White NJ. Antimalarial drug toxicity: a review. Drug Saf 2004; 27: 25-61. [PubMed: 14720085](Review of the toxicities and side effects of antimalarials; artemisinin derivatives are associated with ALT elevations in 0.9% of patients and have been linked to rare cases of severe hepatitis).
- Sowunmi A, Fehintola FA, Adedeji AA, Gbotosho GO, Tambo E, Fateye BA, Happi TC, Oduola AM. Open randomized study of artesunate-amodiaquine vs. chloroquine-pyrimethamine-sulfadoxine for the treatment of uncomplicated Plasmodium falciparum malaria in Nigerian children. Trop Med Int Health 2005; 10: 1161-70. [PubMed: 16262741](Controlled trial of 3 day regimens of artesunate-amodiaquine vs chloroquine-pyrimaethamine-sulfadoxine in 153 children with malaria; “biochemical … parameters remained normal before and after treatment in all subjects”).
- Zongo I, Dorsey G, Rouamba N, Tinto H, Dokomajilar C, Guiguemde RT, Rosenthal PJ, Ouedraogo JB. Artemether-lumefantrine versus amodiaquine plus sulfadoxine-pyrimethamine for uncomplicated falciparum malaria in Burkina Faso: a randomised non-inferiority trial. Lancet 2007; 369(9560): 491-8. [PubMed: 17292769](Controlled trial of artemether-lumefantrine vs sulfadoxine-pyrimethamine and amodiaquine in 521 patients with malaria; adverse event rates were similar and no mention of ALT levels or hepatotoxicity).
- Osorio L, Gonzalez I, Olliaro P, Taylor WR. Artemisinin-based combination therapy for uncomplicated Plasmodium falciparum malaria in Colombia. Malar J 2007; 6: 25. [PMC free article: PMC1820788] [PubMed: 17328806](Controlled trial of 3 day courses of amodiaquine alone vs its combination with artemisinin in 85 patients with P. falciparum malaria; two regimens had equivalent efficacy and safety; ALT elevations in 4%, but without clinical symptoms).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J; Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008; 135: 1924-34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, one case was attributed to artemisinin which was being taken for prevention of malaria, but the causality was scored as only possible).
- Efferth T, Romero MR, Wolf DG, Stamminger T, Marin JJ, Marschall M. The antiviral activities of artemisinin and artesunate. Clin Infect Dis 2008; 47: 804-11. [PubMed: 18699744](Review of in vitro data on antiviral activity of the artemisinins derived from sweet wormwood).
- Gasasira AF, Kamya MR, Achan J, Mebrahtu T, Kalyango JN, Ruel T, Charlebois E, et al. High risk of neutropenia in HIV-infected children following treatment with artesunate plus amodiaquine for uncomplicated malaria in Uganda. Clin Infect Dis 2008; 46: 985-91. [PubMed: 18444813](Analysis of safety of artesunate and amodiaquine in children with malaria; ALT elevations occurred in less than 1%).
- Maiteki-Sebuguzi C, Jagannathan P, Yau VM, Clark TD, Njama-Meya D, Nzarubara B, Talisuna AO, et al. Safety and tolerability of combination antimalarial therapies for uncomplicated falciparum malaria in Ugandan children. Malar 2008; 7: 106. [PMC free article: PMC2441629] [PubMed: 18547415](Controlled trial of 3 combination regimens in 382 children with malaria in Uganda; ALT elevations occurred in 0.5% on amodiaquine/artesunate, 0.3% on amodiaquine/sulfadoxine/pyrimethamine, 0.6% on artemether-lumefantrine).
- Adjei GO, Kurtzhals JA, Rodrigues OP, Alifrangis M, Hoegberg LC, Kitcher ED, Badoe EV, et al. Amodiaquine-artesunate vs artemether-lumefantrine for uncomplicated malaria in Ghanaian children: a randomized efficacy and safety trial with one year follow-up. Malar 2008; 7: 127. [PMC free article: PMC2478668] [PubMed: 18620577](Controlled trial of artesunate-amodiaquine vs artemether-lumefantrice in 227 children with malaria in Ghana; similar efficacy; ALT levels improved during therapy and no reports of hepatitis or ALT increases).
- Sirima SB, Tiono AB, Gansané A, Diarra A, Ouédraogo A, Konaté AT, Kiechel JR, et al. The efficacy and safety of a new fixed-dose combination of amodiaquine and artesunate in young African children with acute uncomplicated Plasmodium falciparum. Malar J 2009; 8: 48. [PMC free article: PMC2662869] [PubMed: 19291301](Controlled trial of fixed vs “loose” dose combinations of amodiaquine and artesunate in 750 children with P. falciparum malaria; similar efficacy [92%] and safety, 7 [~1%] had ALT elevations, one >1000 U/L, but bilirubin normal and no symptoms).
- Guévart E, Aguémon A. [Two cases of fulminant hepatitis during a curative treatment with an artesunate-amodiaquine combination]. Med Mal Infect 2009; 39: 57-60. French. [PubMed: 19013042](Two cases of fulminant hepatitis in women; 32 year old African given artesunate and amodiaquine for fever developed fatigue and anemia 3 days later, with ALT 483 U/L and progressive hepatic failure; 44 year old African physician treated for fever with artesunate and amodiaquine developed fatigue after 3 and jaundice after 5 days, with ALT 15,000 U/L and progressive hepatic failure).
- Centers for Disease Control and Prevention(CDC). Hepatitis temporally associated with an herbal supplement containing artemisinin – Washington, 2008. MMWR Morb Mortal Wkly Rep 2009; 58: 854-6. [PubMed: 19680221](Artemisinin is available in several over-the-counter herbal products; 52 year old man developed jaundice after 10 days of taking herbal product which contained ~600 mg artemisinin [bilirubin 3.1 mg/dL, ALT 898 U/L, Alk P 258 U/L], returning to normal within 2 weeks: Case 1).
- Ndiaye JL, Randrianarivelojosia M, Sagara I, Brasseur P, Ndiaye I, Faye B, Randrianasolo L, et al. Randomized, multicentre assessment of the efficacy and safety of ASAQ--a fixed-dose artesunate-amodiaquine combination therapy in the treatment of uncomplicated Plasmodium falciparum malaria. Malar J 2009; 8: 125. [PMC free article: PMC2698916] [PubMed: 19505304](Controlled trial of artesunate-amodiaquine vs artemether-lumefantine for 3 days in 940 patients with malaria; response rates and side effects were similar in the two groups; rates of ALT elevations decreased during therapy and follow up, from 9% to 6%).
- Kayentao K, Maiga H, Newman RD, McMorrow ML, Hoppe A, Yattara O, Traore H, Kone Y, et al. Artemisinin-based combinations versus amodiaquine plus sulphadoxine-pyrimethamine for the treatment of uncomplicated malaria in Faladje, Mali. Malar J 2009; 8: 5. [PMC free article: PMC2631542] [PubMed: 19128455](Controlled trial of 3 day courses of 3 different antimalarial regimens in 397 children with malaria; no difference in side effects, but regimens with sulfadoxine-pyrimethamine had superior response rates).
- Sinclair D, Zani B, Donegan S, Olliaro P, Garner P. Artemisinin-based combination therapy for treating uncomplicated malaria. Cochrane Database Syst Rev 2009; (3): CD007483. PubMed 19588433. [PMC free article: PMC6532584] [PubMed: 19588433](Review of 50 trials of artemisinin based regimens as therapy of malaria does not mention or discuss hepatotoxicity or ALT elevations).
- Devarbhavi H, Dierkhising R, Kremers WK, Sandeep MS, Karanth D, Adarsh CK. Single-center experience with drug-induced liver injury from India: causes, outcome, prognosis, and predictors of mortality. Am J Gastroenterol 2010; 105: 2396-404. [PubMed: 20648003](313 cases of drug induced liver injury were seen over a 12 year period at a large hospital in Bangalore, India; none were attributed to antimalarials).
- Ayede IA, Falade AG, Sowunmi A, Jansen FH. An open randomized clinical trial in comparing two artesunate-based combination treatments on Plasmodium falciparum malaria in Nigerian children: artesunate/sulphamethoxypyrazine/pyrimethamine (fixed dose over 24 hours) versus artesunate/amodiaquine (fixed dose over 48 hours). Malar J 2010; 9: 378. [PMC free article: PMC3024282] [PubMed: 21194422](Among 250 children with malaria treated with artesunate either with sulfamethoxypyrazine and pyrimethamine over 24 hours or with amodiaquine over 48 hours, there were no hepatic serious adverse events and mean ALT and AST levels did not change).
- Brasseur P, Vaillant MT, Olliaro PL. Anti-malarial drug safety information obtained through routine monitoring in a rural district of South-Western Senegal. Malar J 2012; 11: 402. [PMC free article: PMC3548733] [PubMed: 23216982](Analysis of safety information obtained through routine monitoring of of ~3,000 cases of acute malaria treated with various regimens [usually with artemisinin] in a rural district in Senegal, found no significant changes in laboratory tests, except for a decrease in ALT and AST from pretreatment values and no deaths or severe adverse event attributable to liver injury).
- Zwang J, Dorsey G, Djimdé A, Karema C, Mårtensson A, Ndiaye JL, Sirima SB, et al. Clinical tolerability of artesunate-amodiaquine versus comparator treatments for uncomplicated falciparum malaria: an individual-patient analysis of eight randomized controlled trials in sub-Saharan Africa. Malar J 2012; 11: 260. [PMC free article: PMC3468407] [PubMed: 22856598](Among 3113 patients treated with artesunate and amodiaquine for falciparum malaria in 8 controlled trials, common treatment emergent side effects were cough [33%], anorexia [17%], vomiting [15%], diarrhea [17%], pruritus [18%] and weakness [16%]; 4 patients [1%] developed jaundice, but no details provided).
- Thanh NX, Trung TN, Phong NC, Quang HH, Dai B, Shanks GD, Chavchich M, et al. The efficacy and tolerability of artemisinin-piperaquine (Artequick®) versus artesunate-amodiaquine (Coarsucam™) for the treatment of uncomplicated plasmodium falciparum malaria in south-central Vietnam. Malar J 2012; 11: 217. [PMC free article: PMC3411481] [PubMed: 22741618](Controlled trial comparing artemisinin combined with either piperaquine [n=63] for 2 days or with amodiaquine [65] for 3 days for falciparum malaria in Vietnam reported similar efficacy and tolerance; no severe adverse events reported and no mention of liver injury, jaundice or ALT elevations).
- Schramm B, Valeh P, Baudin E, Mazinda CS, Smith R, Pinoges L, Sundaygar T, et al. Tolerability and safety of artesunate-amodiaquine and artemether-lumefantrine fixed dose combinations for the treatment of uncomplicated Plasmodium falciparum malaria: two open-label, randomized trials in Nimba County, Liberia. Malar J 2013; 12: 250. [PMC free article: PMC3728046] [PubMed: 23866736](Analysis of safety from two prospective controlled trials conducted in Liberia comparing 3 day courses of artesunate-amodiaquine to artemether-lumefantrine in treating uncomplicated Plasmodium falciparum malaria; ALT elevations occurred in 2.0-5.2% of patients and "the only clinical hepatotoxicity was mild jaundice in one patients").
- Yeka A, Lameyre V, Afizi K, Fredrick M, Lukwago R, Kamya MR, Talisuna AO. Efficacy and safety of fixed-dose artesunate-amodiaquine vs. artemether-lumefantrine for repeated treatment of uncomplicated malaria in Ugandan children. PLoS One 2014; 9 (12): e113311. [PMC free article: PMC4249977] [PubMed: 25436614](Among 413 Ugandan children with repeated [n=6027] episodes of malaria treated each time with one of two artemisinin combination regimens, cure and adverse event rates were similar and liver tests abnormalities occurred in 6.5% overall and were treatment related in 0.5%, but all resolved spontaneously and there were no instances of clinically apparent liver injury).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, no cases were attributed to an antimalarial drug, but one occurred in a patient taking an herbal supplement that reportedly contained artemisinin).
- Twomey PS, Smith BL, McDermott C, Novitt-Moreno A, McCarthy W, Kachur SP, Arguin PM. Intravenous artesunate for the treatment of severe and complicated malaria in the United States: clinical use under an investigational new drug protocol. Ann Intern Med 2015; 163: 498-506. [PMC free article: PMC4627466] [PubMed: 26301474](Among 102 US patients with severe malaria treated with intravenous artesunate, the mortality rate was 7% but all deaths were considered due to malaria; ALT or AST elevations occurred in 51%, but most were mild-to-moderate in severity and self-limited in course; there were no instances of clinically apparent liver injury attributed to antimalarial therapy).
- Kumar S. Cholestatic liver injury secondary to artemisinin. Hepatology 2015; 62: 973-4. [PubMed: 25980398](43 year old woman developed jaundice 6 weeks after starting an herbal supplement containing artemisinin [bilirubin 15.4 mg/dL, ALT 675 U/L, Alk P 208 U/L, INR 1.1], resolving slowly upon withdrawal, jaundice lasting 4 months).
- Adjei A, Narh-Bana S, Amu A, Kukula V, Nagai RA, Owusu-Agyei S, Oduro A, et al. Treatment outcomes in a safety observational study of dihydroartemisinin/piperaquine (Eurartesim(®)) in the treatment of uncomplicated malaria at public health facilities in four African countries. Malar J 2016; 15: 43. [PMC free article: PMC4729128] [PubMed: 26818128](Among 1002 patients with malaria treated in 4 African countries with dihydroartemisinin with piperaquine who were tested for ALT and AST, mean levels decreased during therapy and there was no "significant liver or renal impairment", but ALT levels were still elevated at day 7 in 11.5% and serum bilirubin in 7.6% of patients).
- Silva-Pinto A, Ruas R, Almeida F, Duro R, Silva A, Abreu C, Sarmento A. Artemether-lumefantrine and liver enzyme abnormalities in non-severe Plasmodium falciparum malaria in returned travellers: a retrospective comparative study with quinine-doxycycline in a Portuguese centre. Malar J 2017; 16: 43. [PMC free article: PMC5264472] [PubMed: 28122572](Among 57 travellers treated for non-severe malaria, 10 [18%] developed liver enzyme elevations, more commonly with artemether-lumefantrine [42%] than quinine-doxycycline [5%], but none developed clinically apparent liver injury).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Artemisinin, an endoperoxide antimalarial, disrupts the hemoglobin catabolism and heme detoxification systems in malarial parasite.[J Biol Chem. 1999]Artemisinin, an endoperoxide antimalarial, disrupts the hemoglobin catabolism and heme detoxification systems in malarial parasite.Pandey AV, Tekwani BL, Singh RL, Chauhan VS. J Biol Chem. 1999 Jul 2; 274(27):19383-8.
- In vitro selection of Plasmodium falciparum Pfcrt and Pfmdr1 variants by artemisinin.[Malar J. 2016]In vitro selection of Plasmodium falciparum Pfcrt and Pfmdr1 variants by artemisinin.Njokah MJ, Kang'ethe JN, Kinyua J, Kariuki D, Kimani FT. Malar J. 2016 Jul 22; 15(1):381. Epub 2016 Jul 22.
- Susceptibility of Plasmodium falciparum to artemisinins and Plasmodium vivax to chloroquine in Phuoc Chien Commune, Ninh Thuan Province, south-central Vietnam.[Malar J. 2019]Susceptibility of Plasmodium falciparum to artemisinins and Plasmodium vivax to chloroquine in Phuoc Chien Commune, Ninh Thuan Province, south-central Vietnam.Phong NC, Chavchich M, Quang HH, San NN, Birrell GW, Chuang I, Martin NJ, Manh ND, Edstein MD. Malar J. 2019 Jan 17; 18(1):10. Epub 2019 Jan 17.
- Review Natural products as starting points for future anti-malarial therapies: going back to our roots?[Malar J. 2011]Review Natural products as starting points for future anti-malarial therapies: going back to our roots?Wells TN. Malar J. 2011 Mar 15; 10 Suppl 1(Suppl 1):S3. Epub 2011 Mar 15.
- Review [Combined antimalarial therapy using artemisinin].[Parassitologia. 2004]Review [Combined antimalarial therapy using artemisinin].Majori G. Parassitologia. 2004 Jun; 46(1-2):85-7.
- Artemisinin - LiverToxArtemisinin - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...