NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Arsenic is a nonessential trace element that is widely distributed in nature. Arsenic was used in medicinal agents in the 19th and early 20th centuries, but has been replaced by safer and more effective agents and has not been in use for over 50 years. Nevertheless, arsenic is found widely in nature and accidental or intentional acute or chronic exposures to moderate or high levels of arsenic can cause liver injury, sometimes presenting long after the exposure.
Background
Arsenic is a nonessential trace element and well known poison that is found widely in low concentrations in the environment. Typical arsenic concentrations are 2 to 5 parts per billion in soil and sea water. In the United States, the maximal allowable concentration of arsenic in well and drinking water is 50 parts per billion. Arsenic is used in pesticides and herbicides and is a byproduct of the mining of other metals, such as copper and lead. Arsenic can also contaminate herbal preparations and dietary supplements. As a consequence, occupational or accidental exposure to moderate or high doses of arsenic can occur, but are fortunately rare, at least in the United States and most of the developed world. Arsenic was formerly used medically as Fowler's solution (1% arsenic trioxide) to treat inflammatory conditions such as asthma, psoriasis and leukemia, and as various organic arsenicals such as arsphenamine (Salvarsan), mapharsen and tryparsamide to treat syphilis and protozoal infections. These agents are no longer used and have been replaced by more effective and safer agents. Arsenic is still a component of some traditional and herbal preparations and is still used to treat acute promyelocytic leukemia under the brand name Trisenox (arsenic trioxide) in intravenous doses of 10 mg daily for up to 60 days, followed by different dosing in consolidation and maintenance regimens.
Hepatotoxicity
Acute poisoning with arsenic is marked by severe abdominal pain, nausea and vomiting, diarrhea, muscle cramps, metallic taste and extreme thirst, followed by stupor, coma, cardiovascular collapse and death. Death can occur within 24 hours of exposure, but with sublethal doses, survival is possible and liver injury may arise 24 to 48 hours after the acute ingestion. Other symptoms include conjunctival and respiratory tract inflammation, epistaxis, rash, renal insufficiency and painful neuropathy. The characteristics of the liver injury have not been well defined, but are likely similar to those with acute iron poisoning, with a clinical phenotype of acute hepatic necrosis, marked elevations in serum aminotransferase levels, early onset of hepatic failure and rapid recovery in cases without early fatality.
Chronic, lower dose exposure to arsenic can be toxic and result in arsenosis, a syndrome marked by fatigue, nausea and vomiting, abdominal crampy pain, weakness, stupor, seizures and neuropathy. Skin manifestations are frequent and characteristic with chronic excessive exposure marked by hyper- and hypo-pigmentation, a "rain-drop" pattern of skin discoloration, skin dryness and exfoliation, keratosis of the palms and soles, and skin cancers. Arsenic is also deposited in the hair and nails, where it can be detected even after it is no longer measureable in urine. Liver injury can also occur with chronic arsenic exposure, typically with appearance of signs and symptoms of portal hypertension, without obvious cirrhosis (idiopathic or noncirrhotic portal hypertension). The clinical onset of noncirrhotic portal hypertension is often insidious with weight loss, fatigue and abdominal swelling and minor, nonspecific elevations in serum enzymes, followed by appearance of variceal hemorrhage or ascites. Features of portal hypertension (ascites, variceal hemorrhage) rather than hepatic failure (jaundice, encephalopathy or coagulopathy) predominate. Symptoms generally improve slowly upon withdrawal of arsenic exposure and long term survival is not uncommon, although porto-caval shunting may be needed to manage portal hypertension and variceal hemorrhage. Serum enzyme elevations and jaundice are uncommon, but may occur. Chronic exposure is usually due to environmental contamination, from elevated arsenic levels in water due to run-offs from mining or storage of arsenic containing compounds such as herbicides and pesticides. When arsenic was still being used as a medicinal agent, cases of chronic poisoning were linked to use of Fowler's solution for psoriasis and asthma and arsphenamine for syphilis generally after 5 to 25 years of use. Furthermore, some cases became clinically apparent several years after the arsenical was stopped and at a time that arsenic could no longer be detected in urine, tissue or hair samples. Chronic arsenic exposure has also been linked to cirrhosis, although the contribution of alcohol and other chronic liver diseases in reported cases could not be excluded. Chronic exposure has also been linked to liver cancer, including hepatic angiosarcoma and hepatocellular carcinoma. Other long term complications of arsenic exposure include skin discoloration, palmar and plantar keratosis, peripheral neuropathy, and skin and lung cancer which can arise several decades after exposure. Patients presenting with noncirrhotic portal hypertension due to arsenic frequently have other manifestations of its chronic toxicity such as skin discoloration, palmar keratosis and skin cancers.
Arsenic trioxide (Trisenox) given intravenously as therapy of acute promyelocytic leukemia has had limited use, but hepatotoxicity has been reported in 8% to 47% of patients, generally in the form of mild and transient serum enzyme elevations that resolve even with continuation of treatment. Nevertheless, more severe hepatic injury has been reported including cases of acute liver failure, although the clinical features of the injury and relatedness to the therapy were not well defined.
Likelihood score: A[HD] (well known cause of chronic liver injury when given in high dosess).
Mechanism of Injury
Arsenic uncouples oxidative phosphorylation and is a general cytoplasmic toxin binding to and inhibiting sulfhydryl groups on essential enzymes. With acute exposures, the skin, cardiac and neurologic toxicities are most prominent. With chronic exposure, skin and hepatic manifestations may dominant the clinical picture.
Outcome and Management
Arsenic poisoning is often treated with chelation, with uncertain efficacy. Both dimercaprol and succimer have been used, but their efficacy in ameliorating symptoms and signs and speeding clinical recovery has not been documented. The major invention should be directed at detection and elimination of the source of arsenic contamination and identification of others who might be exposed in the same manner.
Drug Class: Trace Elements and Metals
CASE REPORT
Case 1. Noncirrhotic portal hypertension attributed to arsenic exposure.
[Modified from: Upshaw CB Jr, Bryant MF, Claiborne TS Jr. Noncirrhotic portal hypertension after arsenic ingestion. South Med J 1979; 72: 1332-4. PubMed Citation; Upshaw CB Jr, Claiborne TS Jr. Medicinal arsenic poisoning: 27-year follow-up. South Med J 1995; 88: 892-3. PubMed Citation]
A 45 year old man developed recurrent variceal hemorrhage having taken an arsenic containing preparation for 2 years, several years in the past. He denied a history of liver disease, jaundice, alcohol abuse or risk factors for viral hepatitis. Several years in the past he had developed asthma and was treated with Fowler's solution (1% arsenic trioxide) for two years, between the ages of 40 and 42. The estimated total dose of arsenic was 1.6 grams. Thereafter, he felt well until he began developing episodes of hematemesis and melena approximately 3 years later. On examination, he appeared healthy but pale. A spleen tip was felt in the left upper quadrant, but there was no hepatomegaly, jaundice, ascites, peripheral edema, wasting or spider angiomata. Laboratory testing showed a hematocrit of 34%, white blood count 2,700/µL and platelet count 70,000/µL, but routine liver tests were normal. Gastrointestinal radiology showed esophageal varices and splenomegaly. A splenoportogram showed an elevated splenic pulp pressure [29 mm Hg, normal 3-17], but no evidence of splenic or portal vein thrombosis. He underwent splenectomy and anastomosis of the splenic vein to the left renal vein, which normalized the elevated portal pressure. He recovered from surgery uneventfully and had no further gastrointestinal bleeding or symptoms of liver disease, but had mildly abnormal liver test results (AST and Alk P < twice ULN) and an abnormal liver-spleen scan. He also developed several skin carcinomas, but died as a result of a farm accident 27 years after initial presentation and surgery.
Key Points
| Medication: | Arsenic trioxide (1% solution) for 2 years |
|---|---|
| Pattern: | None: normal serum enzymes |
| Severity: | 4+, variceal hemorrhage |
| Latency: | 4 years after a 2 year course of treatment |
| Recovery: | Symptomatically complete |
| Other medications: | None mentioned |
Comment
This case was distinctive in having excellent long term follow up summarized in a subsequent letter to the editor by the authors, 16 years after the first report. Noncirrhotic portal hypertension generally arises as a result of chronic injury, probably to portal venules and arterioles as a result of direct toxic endothelial cell injury caused by the high levels of orally absorbed arsenic in the portal system. The usual markers of liver injury are generally absent, serum enzymes being normal or near normal in the majority of patients before and at the time of initial presentation. In addition, the clinical presentation may be months or years after portal hypertension has developed. The most sensitive marker for the progressive increase in portal pressure is a decline in platelet count, even when in the normal range. Strikingly, arsenic may no longer be detectable in plasma, urine, tissue or hair when the liver injury finally becomes clinically manifest. In this case, as in most instances, withdrawal of the arsenic exposure, conservative management and portal decompression, if needed, is generally effective in resolving the clinical complications. The long term prognosis is often dependent upon the other long term complications of arsenic exposure, including skin, liver and lung carcinoma.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Arsenic – Trisenox®
DRUG CLASS
Trace Elements and Metals
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Arsenic Trioxide | 1327-53-3 | As2-O3 |
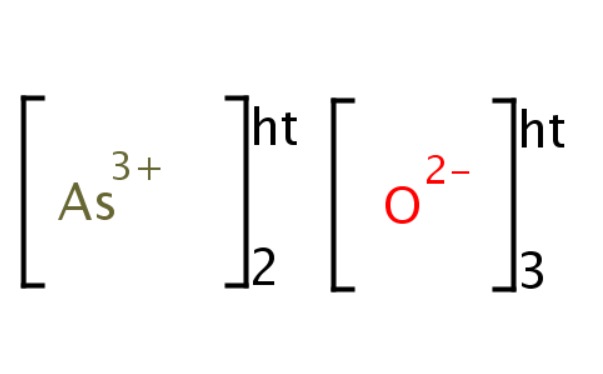 |
ANNOTATED BIBLIOGRAPHY
References updated: 25 July 2017
- Zimmerman HJ. Arsenic. Environmental hepatotoxicity. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, p 420.(Review of hepatotoxicity published in 1999 mentions that exposure to inorganic arsenic and organic arsenicals has been linked convincingly to cases of noncirrhotic portal hypertension and angiosarcoma, but somewhat less well to cirrhosis and hepatocellular carcinoma).
- Toman KG, Dalpiaz AS. Arsensic. Occupational and environmental hepatotoxicity. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, p 670.(Textbook on hepatotoxicity; mentions high incidence of cirrhosis in vineyard workers, coal miners and farmers exposed to arsenic and multiple reports of hepatoportal sclerosis, liver cancer and hepatic angiosarcoma, with water and environmental exposure to excessive concentrations of arsenic).
- Byrns MC, Penning TM. Treatment of metal exposure. Environmental toxicology: carcinogens and heavy metals. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1872-6.(Textbook of pharmacology and therapeutics).
- Hathcock JN, Rader JI. Arsenic. Food additives, contaminants, and natural toxins. In, Shils ME, Olson JA, Shihe M, Ross AC, eds. Modern Nutrition in Health and Disease. 9th ed. Baltimore: Williams & Wilkins, 1999, pp. 1866-7.(Textbook of nutrition).
- Bang FL. [Hydrops due to arsenic ingestion]. Soc Med Havn Collect 1884; 1: 307-9. Not in PubMed.(Initial report of anasarca associated with chronic use of arsenicals, quoted in O'Leary et al. 1928).
- Geyer L. Arch F Dermat u Syph 1898; 43: 221. Not in PubMed.(Quoted in Franklin [1950]; patient developed anasarca and ascites while on medicinal arsenic).
- Hamburger LP. Bull John Hopkins Hosp 1900; 11: 87. Not in PubMed.(Quoted in Franklin [1950]; patient developed anasarca and ascites while on medicinal arsenic).
- Hutchinson J. Arch Surg 1895; 6: 380. Not in PubMed.(Quoted in Franklin [1950]; patient developed skin discoloration, keratosis and ascites while on medicinal arsenic).
- Reynolds ES. An account of the epidemic outbreak of arsenical poisoning occurring in beer-drinkers in the north of England and the Midland counties in 1900. Lancet 1901; 157 (4038): 166-70. Not in PubMed. [PMC free article: PMC2036791] [PubMed: 20896969](A large number of cases of suspected alcoholic neuritis with skin eruptions and keratosis occurring in Manchester, England in 1900 were found to be due to arsenic poisoning from contamination of inexpensive beer [perhaps by sulfuric acid used in its manufacture], most patients presenting with neuropathy, but some with ascites and suspected cirrhosis).
- Sturroch AC, Brown J, Bowser JE, Infield S. Epidemic of peripheral neuritis traced to arsenical contamination of beer-making materials. Brit Med J 1900; 2: 1815-6. Not in PubMed. [PMC free article: PMC2464176] [PubMed: 20759350](An epidemic of painful peripheral neuropathy was traced to inexpensive beer drinking, possibly due to contamination in added sugar; 8 patients also presented with an "interstitial hepatitis" marked by abdominal pain, hepatomegaly and ascites sometimes with mild jaundice, resolving rapidly upon stopping beer intake).
- O'Leary PA, Snell AM, Bannick EG. Portal cirrhosis associated with chronic inorganic arsenical poisoning. JAMA 1928; 90: 1856-9. Not in PubMed.(Two cases and review of literature; 52 year old man developed abdominal distention 4 years after starting a solution of potassium arsenite for dermatitis herpetiformis, with normal serum bilirubin despite massive ascites and slow improvement with stopping; 41 year old man developed ascites and skin pigmentation a year after starting potassium arsenite with normal serum bilirubin [0.5 mg/dl] and slow improvement on stopping arsenic).
- Weir JF. Cirrhosis associated with chronic inorganic arsenical poisoning. Mayo Clin Pro 1930; 5: 173. Not in PubMed.(Two cases: 43 year old woman with pruritus, hyperpigmentation and jaundice [bilirubin 3.4 mg/dL] who developed ascites and variceal hemorrhage and had arsenic found in urine, but no mention of source; 27 year old woman with pruritus, hyperpigmentation and jaundice [bilirubin 7.8 mg/dL] suspected to be on Fowler's solution; but neither case had histologic confirmation of cirrhosis and may have represented other forms of liver disease).
- Franklin M, Bean WB, Hardin RC. Fowler's solution as an etiologic agent in cirrhosis. Am J Med Sci 1950; 219: 589-96. [PubMed: 15419170](Three cases of arsenical dermatitis and cirrhosis in 56-57 year old Iowan farmers who developed evidence of cirrhosis [ascites, variceal hemorrhage, mild jaundice], 2-9 years after starting Fowler's solution of 1% arsenic trioxide, with little evidence of improvement after stopping and no hepatic histology).
- Wade HJ, Frazer ES. Toxipathic hepatitis due to Fowler's solution; a case treated with dimercaprol. Lancet 1953; 1 (6754): 269-71. [PubMed: 13012048](40 year old man developed fatigue 16 months after starting Fowler's solution for dermatitis herpetiformis with skin pigmentation and ascites, and was treated with dimercaprol with excellent response).
- Roth F. [Chronic arsenic poisoning of Moselle vineyard-workers, with special reference to arsenic cancer]. Z Krebsforsch 1956; 61 (3): 287-319. German. [PubMed: 13401997]
- Roth F. [After-effects of chronic arsenism in Moselle wine makers]. Dtsch Med Wochenschr. 1957; 82: 211-7. German. [PubMed: 13414511](Analysis of late effects of use of arsenic in pesticides in German vineyards from 1925 to 1942, including cirrhosis and lung cancer).
- Dinman BD. Arsenic: chronic human intoxication. J Occup Med 1960; 2: 137-141.
- Shandon S, Sherlock S. Portal hypertension in the myeloproliferative syndrome and the reticuloses. Am J Med 1962; 32: 758-64. [PubMed: 13911166](Description of 6 patients with a myeloproliferative disorder presenting with evidence of portal hypertension, 3 having portal thrombosis and 3 unexplained, liver tests being normal except for mild Alk P elevations).
- Mikkelsen WP, Edmondson HA, Peters RL, Redeker AG, Reynolds TB. Extra- and intrahepatic portal hypertension without cirrhosis(hepatoportal sclerosis). Ann Surg 1965; 162: 602-20. [PMC free article: PMC1476958] [PubMed: 5833586](Description of 36 patients with idiopathic portal hypertension without cirrhosis presenting with variceal hemorrhage or ascites and normal or near normal liver histology, some with portal vein obstruction and some not, but with time the liver became shrunken in some patients; the authors termed this syndrome "hepatoportal sclerosis").
- Sherlock S, Feldman CA, Moran B, Scheuer PJ. Partial nodular transformation of the liver with portal hypertension. Am J Med 1966; 40: 195-203. [PubMed: 5948135](Description of 4 cases of noncirrhotic portal hypertension which they called "partial nodular transformation" marked by variceal hemorrhage and ascites, but relatively normal liver function and minimally abnormal liver tests, histology showing nodular formation without much fibrosis).
- Williams R. Portal hypertension in idiopathic tropical splenomegaly. Lancet 1966; 1 (7433): 329-33. [PubMed: 4159474](Portal hypertension was found in the majority of patients with idiopathic splenomegaly, some but not all of which appeared to be due to increased portal blood flow).
- Boyer JL, Sen Gupta KP, Biswas SK, Pal NC, Basu Mallick KC, Iber FL, Basu AK. Idiopathic portal hypertension. Comparison with the portal hypertension of cirrhosis and extrahepatic portal vein obstruction. Ann Intern Med 1967; 66: 41-68. [PubMed: 6015813](Description of 21 patients with noncirrhotic portal hypertension, frequent finding being intrahepatic portal vein sclerosis).
- Regelson W, Kim U, Ospina J, Holland JF. Hemangioendothelial sarcoma of liver from chronic arsenic intoxication by Fowler's solution. Cancer 1968 Mar; 21 (3): 514-22. [PubMed: 5688987](49 year old with psoriasis developed fatigue, jaundice and edema 7 years after stopping Fowler's solution which he had taken off-and-on for 17 years, histology showing hemangioendothelial sarcoma of the liver [hepatic angiosarcoma]).
- Regelson W, Kim U, Ospina J, Holland JF. Hemangioendothelial sarcoma of liver from chronic arsenic intoxication by Fowler's solution. Cancer 1968; 21: 514-22. [PubMed: 5688987](49 year old man had taken Fowler's solution for 17 years for psoriasis and developed jaundice and ascites, dying 2 months later and autopsy showing massive invasion by neoplastic endothelial sarcoma cells).
- Iber FL. Obliterative portal venopathy of the liver and "idiopathic portal hypertension". Ann Intern Med 1969; 71: 660-1. [PubMed: 5809690](Editorial on idiopathic portal hypertension and the possible role of obliterative venopathy).
- Tandon BN, Lakshminarayanan R, Bhargava S, Nayak NC, Sama SK. Ultrastructure of the liver in non-cirrhotic portal fibrosis with portal hypertension. Gut 1970; 11: 905-10. [PMC free article: PMC1553129] [PubMed: 5492248](Results of electron microscopy done on 9 cases of idiopathic portal hypertension found normal hepatic cytoplasm and nuclei, but somewhat increase in collagen in widened spaces of Disse).
- Zeegen R, Stansfeld AG, Dawson AM, Hunt AH. Prolonged survival after portal decompression of patients with non-cirrhotic intrahepatic portal hypertension. Gut 1970; 11: 610-7. [PMC free article: PMC1553070] [PubMed: 5452049](Among 251 patients undergoing portacaval shunting, 25% did not have cirrhosis, many of whom had only minor changes in hepatic architecture; these patients had better survival [83% at 5 years] than those with cirrhosis [46%]).
- Sama SK, Bhargava S, Nath NG, Talwar JR, Nayak NC, Tandon BN, Wig KL. Noncirrhotic portal fibrosis. Am J Med 1971; 51: 160-9. [PubMed: 5315322](Among 300 cases of portal hypertension studied at a referral center in India, 25% had neither cirrhosis nor portal thrombosis and presented with splenomegaly and variceal hemorrhage or ascites, but with minimal hepatic dysfunction; the liver showing some degree of nodularity, mild fibrosis, inconspicuous small portal veins and thickening of walls of medium sized portal veins).
- Chronic arsenical poisoning and non-cirrhotic portal hypertension – a case for diagnosis. BMJ 1971; 4 (5789): 725-31. [PMC free article: PMC1799988] [PubMed: 5129618](67 year old woman had taken arsenicals for psoriasis for several years in her 20s and developed recurrent variceal hemorrhage in her 50s and later severe hematemesis, ascites and hepatic encephalopathy [bilirubin 1.1 mg/dL, Alk P 13 KA Units], resulting in death at age 67; autopsy showed varices, portal vein thrombosis, but no cirrhosis or signs of regeneration).
- Louria DB, Joselow MM, Browder AA. The human toxicity of certain trace elements. Ann Intern Med 1972; 76: 307-19. [PubMed: 4550590](Review of toxicity of trace elements including cobalt, copper, manganese, copper, molybdenum, vanadium selenium, nickel, arsenic, cadmium, tellurium and tin; no discussion of liver injury, cirrhosis or liver cancer).
- Feinglass EJ. Arsenic intoxication from well water in the United States. N Engl J Med 1973; 288: 828-30. [PubMed: 4348410](Among 13 workers exposed to arsenic from well water [21,000 parts per billion] over a 10 week period, 11 developed symptoms of nausea and vomiting, abdomen pain or diarrhea and 2 had neuropathy).
- Knolle J, Föer E, Roessner A, Themann H, HöP, Meyer zum Büfelde KH. [Non-cirrhotic portal fibrosis(hepatoportal sclerosis) after chronic arsenic poisoning: clinical and morbid-anatomical findings (author's transl)]. Dtsch Med Wochenschr 1974; 99: 903-8. German. [PubMed: 4546042](40 year old man had esophageal variceal hemorrhage from noncirrhotic portal hypertension attributed to a five year course of organic arsenicals for psoriasis 10 years previously).
- Morris JS, Schmid M, Newman S, Scheuer PJ, Sherlock S. Arsenic and noncirrhotic portal hypertension. Gastroenterology 1974; 66: 86-94. [PubMed: 4809505](Two patients with portal hypertension and variceal hemorrhage with minimal portal fibrosis had been treated with Fowler's solution for psoriasis for 3 and 22 years, and also suffered with skin pigmentation, skin cancers, keratosis and laryngeal and bronchial carcinomas).
- Wilkinson SP, McHugh P, Horsley S, Tubbs H, Lewis M, Thould A, Winterton M, et al. Arsine toxicity aboard the Asiafreighter. Br Med J 1975; 3 (5983): 559-63. [PMC free article: PMC1674520] [PubMed: 169942](Four sailors were exposed to arsenous hydride gas, which had leaked from a metal cylinder during a storm at sea, and developed severe fever, headache, muscle and abdominal pains, nausea and vomiting followed by dyspnea, intravascular hemolysis, renal failure and stupor or coma; all had tender hepatomegaly, but liver tests were mostly normal and all recovered).
- Huet PM, Guillaume E, Cote J, Léré, Lavoie P, Viallet A. Noncirrhotic presinusoidal portal hypertension associated with chronic arsenical intoxication. Gastroenterology 1975; 68 (5 Pt 1): 1270-7. [PubMed: 1126603](39 year old man developed noncirrhotic portal hypertension, having received organic arsenicals for psoriasis for 12 years, presenting with splenomegaly and variceal hemorrhage without hepatomegaly or abnormal liver tests).
- Lander JJ, Stanley RJ, Sumner HW, Boswell DC, Aach RD. Angiosarcoma of the liver associated with Fowler's solution (potassium arsenite). Gastroenterology 1975 Jun; 68(6): 1582-6. [PubMed: 1169181](43 year old man with psoriasis developed variceal hemorrhage 6 years after taking Fowler's solution for 15 years, with hyperkeratosis, on soles and palms, hyperpigmentation, hepatomegaly [bilirubin 1.3 mg/dL, AST 87 U/L, Alk P 332 U/L] with large hepatic angiosarcoma, but normal appearing surrounding nontumorous liver tissue).
- Villeneuve JP, Huet PM, Joly JG, Marleau D, CôJ, Léré, Lafortune M, et al. Idiopathic portal hypertension. Am J Med 1976; 61: 459-64. [PubMed: 1086057](Five cases of idiopathic portal hypertension presenting with variceal hemorrhage, but without cirrhosis, including one attributed to chronic arsenic exposure).
- Datta DV. Letter: Arsenic and non-cirrhotic portal hypertension. Lancet 1976; 1 (7956): 433. [PubMed: 55707](Arsenic levels were high in the liver of a patient with arsenic related noncirrhotic portal hypertension [247 vs 10 µg/100 g], but were also elevated in kidney, brain, intestine and heart).
- Hine CH, Pinto SS, Nelson KW. Medical problems associated with arsenic exposure. J Occup Med 1977; 19: 391-6 . [PubMed: 141494](Monitoring of employees in a large smeltering plant found little evidence of arsenic toxicity, AST elevations in 2.3%, but seemingly unrelated to the exposure).
- Pimentel JC, Menezes AP. Liver disease in vineyard sprayers. Gastroenterology 1977; 72: 275-83. [PubMed: 556610](Histologic description of livers from 30 vineyard sprayers' exposed chronically to high levels of copper, found copper granules in Kupffer cells in all 30, with granulomas, fibrosis [portal], nodular regeneration ["liver function was usually normal"] angiosarcoma, cirrhosis and NCPH, although the rates of these findings were not given).
- Ulmer DD. Trace elements. N Engl J Med 1977; 297: 318-21. [PubMed: 876314](Brief review of trace elements, their metabolic roles, deficiencies and toxicities).
- Popper H, Thomas LB, Telles NC, Falk H, Selikoff IJ. Development of hepatic angiosarcoma in man induced by vinyl chloride, thorotrast, and arsenic. Comparison with cases of unknown etiology. Am J Pathol 1978; 92: 349-76. [PMC free article: PMC2018292] [PubMed: 567014](Review of the histologic features of hepatic angiosarcoma of varying causes indicated a commonality of early changes, suggesting shared pathogenesis in those cases of unknown cause).
- Axelson O, Dahlgren E, Jansson CD, Rehnlund SO. Arsenic exposure and mortality: a case-referent study from a Swedish copper smelter. Br J Ind Med 1978; 35: 8-15. [PMC free article: PMC1008317] [PubMed: 629894](Case control study of causes of death among Swedish copper smelters with different levels of arsenic exposure suggested an increased rate of lung cancer and cardiovascular disease and a slight increase in cirrhosis).
- Datta DV, Mitra SK, Chhuttani PN, Chakravarti RN. Chronic oral arsenic intoxication as a possible aetiological factor in idiopathic portal hypertension (non-cirrhotic portal fibrosis) in India. Gut 1979; 20: 378-84. [PMC free article: PMC1412437] [PubMed: 468068](Analysis of liver tissue from 9 patients with non-cirrhotic portal hypertension found elevated arsenic levels in 4 which was linked to increased concentrations in drinking water and perhaps to arsenic contamination of Ayurvedic medications).
- Cowlishaw JL, Pollard EJ, Cowen AE, Powell LW. Liver disease associated with chronic arsenic ingestion. Aust N Z J Med 1979; 9:310-3. [PubMed: 223536](Two cases; 64 and 45 year old men with 12 and 10 years of arsenic therapy developed variceal hemorrhage, biopsies showing hepatocellular carcinoma in one and mild fibrosis, but no cirrhosis in the other).
- Chainuvati T, Viranuvatti V. Idiopathic portal hypertension and chronic arsenic poisoning. Report of a case. Dig Dis Sci 1979; 24: 70-3. [PubMed: 154997](28 year old Thai woman with psoriasis on long term arsenicals developed variceal bleed and non-cirrhotic portal hypertension [bilirubin 1.0 mg/dL, AST 27, Alk P normal] and underwent splenorenal shunt with excellent outcome).
- Szuler IM, Williams CN, Hindmarsh JT, Park-Dincsoy H. Massive variceal hemorrhage secondary to presinusoidal portal hypertension due to arsenic poisoning. Can Med Assoc J 1979; 120: 168-71. [PMC free article: PMC1818860] [PubMed: 310707](64 year old Canadian man developed variceal bleed having taken an over-the-counter arsenical for 55 years [bilirubin, AST and Alk P normal] and underwent splenorenal shunt with excellent outcome: "Overseas Asthma Relief").
- Upshaw CB Jr, Bryant MF, Claiborne TS Jr. Noncirrhotic portal hypertension after arsenic ingestion. South Med J 1979; 72: 1332-4. [PubMed: 482995](46 year old man developed non-cirrhotic portal hypertension 3 years after finishing a 2 year course of Fowler's solution [liver tests normal], with resolution of bleeding episodes after splenectomy and splenic-renal vein anastomosis: Case 1).
- Falk H, Herbert J, Crowley S, Ishak KG, Thomas LB, Popper H, Caldwell GG. Epidemiology of hepatic angiosarcoma in the United States: 1964-1974. Environ Health Perspect 1981; 51: 107-13. [PMC free article: PMC1568861] [PubMed: 7199426](Survey of hepatic angiosarcoma in the United States between 1964 and 1974 found 168 cases, male predominance, peak age 50-59 years, 25% due to known environmental cause [vinyl chloride in 12, arsenic in 6, anabolic steroids in 4 and thorotrast in 20]).
- Falk H, Caldwell GG, Ishak KG, Thomas LB, Popper H. Arsenic-related hepatic angiosarcoma. Am J Ind Med 1981; 2: 43-50. [PubMed: 6891179](In a nationwide survey, 7 cases of hepatic angiosarcoma attributable to arsenic exposure were identified between 1964-1974, including 5 who were treated with Fowler's solution for 9-29 years, generally for asthma or psoriasis).
- Falk H, Herbert JT, Edmonds L, Heath CW Jr, Thomas LB, Popper H. Review of four cases of childhood hepatic angiosarcoma--elevated environmental arsenic exposure in one case. Cancer 1981; 47: 382-91. [PubMed: 7193080](Review of 4 cases of hepatic angiosarcoma occurring in infants, ages 1-30 months, which had histologic features distinct from those in adults, one case attributed to arsenic exposure and three idiopathic).
- Datta DV, Narang AP, Sahni MM, Banerjee CK, Walia BN. Role of arsenic and copper in the pathogenesis of Indian childhood cirrhosis. Indian Pediatr 1981; 18: 53-7. [PubMed: 7262995](Hepatic arsenic levels were elevated in 11 and copper in 15 of 19 children with Indian Childhood Cirrhosis, levels also being elevated in several Ayurvedic medicines used by mothers of the children during the first trimester of pregnancy).
- Roat JW, Wald A, Mendelow H, Pataki KI. Hepatic angiosarcoma associated with short-term arsenic ingestion. Am J Med 1982; 73: 933-6. [PubMed: 6890767](45 year old man, who had taken Fowler's solution for 6 months at age 12, developed jaundice and fatigue [bilirubin 6.6 mg/dL, ALT 110 U/L, Alk P 497 U/L], liver biopsy showing hepatic angiosarcoma).
- Lüth H. The consequences of chronic arsenic poisoning among Moselle wine growers. Pathoanatomical investigations of post-mortem examinations performed between 1960 and 1977. J Cancer Res Clin Oncol 1983; 105: 173-82. [PubMed: 6826638](Arsenic was eliminated from pesticides in Germany in 1942, but residual toxicity persisted including high rates of cirrhosis and lung cancer [the most common cause of death] up to 25 years later).
- Koshy A, Narang AP, Bhusnurmath SR. Hepatic arsenic in non-cirrhotic portal fibrosis. Toxicol Lett 1983; 19: 201. [PubMed: 6658826](Arsenic levels were elevated in livers from autopsies of patients with cirrhosis [81 µg], noncirrhotic portal hypertension [26 µg] and other liver diseases [56 µg] compared to controls [2 µg/100g], casting doubt on its role in non-cirrhotic portal hypertension).
- Narang AP, Datta DV. Arsenic and liver. J Assoc Physicians India 1983 Feb; 31(2): 87-90. [PubMed: 6885713](Review of the problem of arsenic in the environment, in opium samples and Ayurvedic medicines and the effects of arsenic on the liver, including portal hypertension and its possible role in causing Indian childhood cirrhosis).
- Kasper ML, Schoenfield L, Strom RL, Theologides A. Hepatic angiosarcoma and bronchioloalveolar carcinoma induced by Fowler's solution. JAMA 1984; 252: 3407-8. [PubMed: 6094851](67 year old man developed weakness, anorexia, ascites and jaundice [bilirubin 8.5 mg/dL, AST 34 U/L, Alk P 130 U/L] and gave a history of taking Fowler's solution for 8 years, 40 years earlier, autopsy showing hepatic angiosarcoma and bronchioalveolar carcinoma).
- Okuda K, Kono K, Ohnishi K, Kimura K, Omata M, Koen H, Nakajima Y, et al. Clinical study of eighty-six cases of idiopathic portal hypertension and comparison with cirrhosis with splenomegaly. Gastroenterology 1984; 86: 600-10. [PubMed: 6698361](Description of 86 cases of idiopathic portal hypertension seen between 1965 and 1982 at Chiba University Hospital, 16 men and 70 women, ages 7 to 74 years, often presenting with variceal hemorrhage, ascites and abdominal pain, with splenomegaly and thrombocytopenia, but normal or near normal liver tests [ALT normal in 72% and Alk P in 49%], histology showing portal fibrosis and survival being better than matched control group with cirrhosis and portal hypertension).
- Armstrong CW, Stroube RB, Rubio T, Siudyla EA, Miller GB Jr. Outbreak of fatal arsenic poisoning caused by contaminated drinking water. Arch Environ Health 1984; 39: 276-9. [PubMed: 6497443](Nine family members developed arsenic poisoning caused by contamination of well water [by pesticide], 5 developing renal injury and 4 hepatitis; the most common symptoms were vomiting and diarrhea, periorbital swelling, epistaxis and anemia followed by seizures, fever, rash and coma; 2 dying of heart and renal failure with sepsis).
- Winship KA. Toxicity of inorganic arsenic salts. Adverse Drug React Acute Poisoning Rev 1984; 3: 129-60. [PubMed: 6397979](Review of the acute and chronic effects of arsenic exposure, both environmental and medicinal).
- el Zayadi A, Khalil A, el Samny N, Hamza MR, Selim O. Hepatic angiosarcoma among Egyptian farmers exposed to pesticides. Hepatogastroenterology 1986; 33: 148-50. [PubMed: 3758905](14 Egyptian farmers were diagnosed with hepatic angiosarcoma at a single referral hospital between 1980 and 1984; 10 had a history of arsenic exposure).
- Guha Mazumder DN, Chakraborty AK, Ghose A, Gupta JD, Chakraborty DP, Dey SB, Chattopadhyay N. Chronic arsenic toxicity from drinking tubewell water in rural West Bengal. Bull World Health Organ 1988; 66: 499-506. [PMC free article: PMC2491171] [PubMed: 3262450](Among 13 Indian patients [ages 15-50 years] with chronic arsenic skin toxicity, all had liver and 5 spleen enlargement, but routine liver tests were normal, while liver biopsies showed mild inflammation and fibrosis without cirrhosis; an epidemiological study of the patients' villages showed high levels of arsenic in the well water [2 mg/L] and frequent skin discoloration and hepatomegaly [both 93%], which were not found in villages with low arsenic levels in drinking water).
- Mueller PD, Benowitz NL. Toxicologic causes of acute abdominal disorders. Emerg Med Clin North Am 1989; 7: 667-82. [PubMed: 2663462](Review of gastrointestinal toxicity of agents including iron, mercury and copper).
- Piontek M, Hengels KJ, Borchard F, Strohmeyer G. [Noncirrhotic liver fibrosis after chronic arsenic poisoning]. Dtsch Med Wochenschr 1989; 114: 1653-7. German. [PubMed: 2806096](67 year old woman who was treated with Fowler's solution since childhood for psoriasis developed non-cirrhotic portal hypertension and recurrent variceal hemorrhage; bleeding episodes resolving after portal decompression surgery).
- Poklis A, Saady JJ. Arsenic poisoning: acute or chronic? Suicide or murder? Am J Forensic Med Pathol 1990; 11: 226-32. [PubMed: 2220708](62 year old man developed intermittent bouts of abdominal pain, vomiting, dehydration and diarrhea with skin pigmentation and keratosis, neutropenia and peripheral neuropathy and on autopsy had elevated arsenic concentrations in hair and tissue; he being the 5th husband of an often widowed wife).
- Nevens F, Fevery J, Van Steenbergen W, Sciot R, Desmet V, De Groote J. Arsenic and non-cirrhotic portal hypertension. A report of eight cases. J Hepatol 1990; 11: 80-5. [PubMed: 2398270](Among 47 patients [3 women, 4 men, ages 24-55 years] with non-cirrhotic portal hypertension seen over a 10 year period, 8 gave a history of taking Fowler's solution for psoriasis; all had esophageal varices and splenomegaly with normal liver tests and liver history showing portal fibrosis without cirrhosis; estimated intake was 3-27 grams, over 2 to 15 years, and clinical presentation 2 to 16 years later with massive variceal bleeding in 7 and ovarian cancer in 1).
- Labadie H, Stoessel P, Callard P, Beaugrand M. Hepatic venoocclusive disease and perisinusoidal fibrosis secondary to arsenic poisoning. Gastroenterology 1990; 99: 1140-3. [PubMed: 2394335](38 year old alcoholic man underwent 3 liver biopsies for unexplained liver test abnormalities and during an admission for suspected self-inflicted arsenic poisoning, biopsies showed perisinusoidal fibrosis and sinusoidal dilatation, which subsequently resolved).
- Salgado M, Sans M, Forns X, Bruguera M, Castells A, Navasa M, RodéJ. [Hepatic angiosarcoma: a report of a case associated with treatment with arsenic salts and a review of the literature]. Gastroenterol Hepatol 1995; 18: 132-5. Spanish. [PubMed: 7621289](63 year old man presented with hemoperitoneum, emergency laparotomy demonstrating a large hepatic angiosarcoma; the only known toxic exposure was a course of intravenous arsenic containing Neosalvarrsan at the age of 17, 45 years before presentation).
- Upshaw CB Jr, Claiborne TS Jr. Medicinal arsenic poisoning: 27-year follow-up. South Med J 1995; 88: 892-3. [PubMed: 7631226](Letter with follow-up on patient who had non-cirrhotic portal hypertension after a 5 year course of arsenic therapy [Upshaw 1979], who subsequently had no further bleeding, but developed mildly abnormal liver tests and died from a farm accident 15 years later).
- Loguercio C, De Girolamo V, Federico A, Feng SL, Cataldi V, Del Vecchio Blanco C, Gialanella G. Trace elements and chronic liver diseases. J Trace Elem Med Biol 1997; 11: 158-61. [PubMed: 9442462](Blood levels of chromium, manganese, cooper and rubidium were similar in patients with hepatitis C related cirrhosis as controls, but selenium and zinc levels were lower).
- Hernáez-Zavala A, Del Razo LM, Aguilar C, GarcíVargas GG, Borja VH, CebriáME. Alteration in bilirubin excretion in individuals chronically exposed to arsenic in Mexico. Toxicol Lett 1998; 99: 79-84. [PubMed: 9817078](Among 51 persons chronically exposure to high arsenic levels in drinking water, serum direct bilirubin and alkaline phosphatase were mildly elevated with little or no change in ALT, AST or GGT).
- Huang SY, Yang CH, Chen YC. Arsenic trioxide therapy for relapsed acute promyelocytic leukemia: an useful salvage therapy. Leuk Lymphoma 2000; 38: 283-93. [PubMed: 10830735](Review of arsenic trioxide as therapy of promyelocytic leukemia; despite a lack of controlled trials the authors conclude that it is useful as salvage therapy; liver dysfunction was reported in 8-46% of treated patients in 3 case series).
- Jensen K. [Arsenic as an environmental problem]. Ugeskr Laeger 2000 Dec 4; 162 (49): 6672-5. Danish. [PubMed: 11188053](Review of contamination of ground and well water with arsenic that was particularly common in the well drilling in the Ganges delta during the 1960s).
- Loguercio C, De Girolamo V, Federico A, Feng SL, Crafa E, Cataldi V, Gialanella G, et al. Relationship of blood trace elements to liver damage, nutritional status, and oxidative stress in chronic nonalcoholic liver disease. Biol Trace Elem Res 2001; 81: 245-54. [PubMed: 11575681](Analysis of trace element concentrations in 50 patients with chronic liver disease [39 with cirrhosis] and 10 controls found slight decreases in iron, zinc and selenium in patients with cirrhosis).
- Guha Mazumder DN. Arsenic and liver disease. J Indian Med Assoc 2001 Jun; 99 (6): 311, 314-5, 318-20. [PubMed: 11678619](Clinical description of 248 Indian patients with chronic arsenic toxicity found hepatomegaly in 77%, splenomegaly 30%, ascites 2%; liver tests done in 93 found ALT elevations in 26% and Alk P 29%; liver biopsy done in 69 cases showed portal fibrosis in 91% and cirrhosis in 3%).
- Guha Mazumder DN. Chronic arsenic toxicity: clinical features, epidemiology, and treatment: experience in West Bengal. J Environ Sci Health A Tox Hazard Subst Environ Eng 2003; 38: 141-63. [PubMed: 12635824](Clinical description of 248 Indian patients with chronic arsenic toxicity found hepatomegaly in 77%, splenomegaly 30%, ascites 2%; liver tests done in 93 found ALT elevations in 26% and Alk P 29%; liver biopsy done in 69 cases showed portal fibrosis in 91% and cirrhosis in 3%; in epidemiological studies, rates of hepatomegaly correlated with higher arsenic levels in drinking water [105] compared to controls [3%]).
- Srivastava A, Peshin SS, Kaleekal T, Gupta SK. An epidemiological study of poisoning cases reported to the National Poisons Information Centre, All India Institute of Medical Sciences, New Delhi. Hum Exp Toxicol 2005; 24: 279-85. [PubMed: 16004194](Among 2719 calls to an Indian poisoning center over a 3 year period, 48 [2%] were for copper sulfate and 6 [<0.5%] for heavy metals including arsenic, lead, mercury and thallium).
- De Capitani EM, Vieira RJ, Madureira PR, Mello SM, Kira CS, Soubhia PC, Toledo AS. Auditory neurotoxicity and hepatotoxicity after MSMA(monosodium methanarsenate) high dose oral intake. Clin Toxicol (Phila) 2005; 43: 287-9. [PubMed: 16035206](36 year old man took a suicidal overdose of the herbicide monosodium methanarsenate [MSMA] and rapidly developed nausea, vomiting and drowsiness, followed by deafness and abnormal liver tests [bilirubin 9.8 mg/dL, ALT 394 U/L, Alk P 327 U/L, creatinine 1.4 mg/dL] that mostly improved with dimercaprol chelation therapy [bilirubin 1.0 mg/dL, ALT 58 U/L, Alk P 377 U/L]).
- Mukherjee A, Sengupta MK, Hossain MA, Ahamed S, Das B, Nayak B, Lodh D, et al. Arsenic contamination in groundwater: a global perspective with emphasis on the Asian scenario. J Health Popul Nutr 2006; 24: 142-63. [PubMed: 17195556](Overview of arsenic contamination in groundwater from published reports from 42 areas from 6 continents).
- Mathews V, Desire S, George B, Lakshmi KM, Rao JG, Viswabandya A, Bajel A, et al. Hepatotoxicity profile of single agent arsenic trioxide in the treatment of newly diagnosed acute promyelocytic leukemia, its impact on clinical outcome and the effect of genetic polymorphisms on the incidence of hepatotoxicity. Leukemia 2006; 20: 881-3. [PubMed: 16525498](Among 83 patients with newly diagnosed acute promyelocytic leukemia who were treated with arsenic trioxide, 96% achieved remission and hepatotoxicity occurred in 29 [39%], but resolved despite continuing therapy in 21 and, of 8 who were rechallenged, only 1 had recurrence; toxicity was grade 4 [severe] in 8 patients, but none died from liver injury).
- Kapaj S, Peterson H, Liber K, Bhattacharya P. Human health effects from chronic arsenic poisoning--a review. J Environ Sci Health A Tox Hazard Subst Environ Eng 2006; 41: 2399-428. [PubMed: 17018421](Thorough review of the complications of chronic arsenic in take).
- Ahamed S, Kumar Sengupta M, Mukherjee A, Amir Hossain M, Das B, Nayak B, et al. Arsenic groundwater contamination and its health effects in the state of Uttar Pradesh(UP) in upper and middle Ganga plain, India: a severe danger. Sci Total Environ 2006; 370(2-3): 310-22. [PubMed: 16899281](Analysis of well water arsenic found high levels in 3 districts in Uttar Padesh with arsenical skin lesions in 20% of adults and 6% of children; no mention of liver related complications).
- Chen Y, Parvez F, Gamble M, Islam T, Ahmed A, Argos M, Graziano JH, et al. Arsenic exposure at low-to-moderate levels and skin lesions, arsenic metabolism, neurological functions, and biomarkers for respiratory and cardiovascular diseases: review of recent findings from the Health Effects of Arsenic Longitudinal Study (HEALS) in Bangladesh. Toxicol Appl Pharmacol 2009; 239: 184-92. [PMC free article: PMC3904798] [PubMed: 19371619](Assessment of well water arsenic exposure and possible complications in Bangladesh, does not discuss hepatic side effects).
- Islam K, Haque A, Karim R, Fajol A, Hossain E, Salam KA, Ali N, et al. Dose-response relationship between arsenic exposure and the serum enzymes for liver function tests in the individuals exposed to arsenic: a cross sectional study in Bangladesh. Environ Health 2011; 10: 64. [PMC free article: PMC3146918] [PubMed: 21740555](In a study of 200 Bangladesh residents, a positive association was found between higher drinking water arsenic levels [>50 vs 10-50 vs <10 µg/L] and higher serum enzyme levels [ALT 34 vs 27 vs 24 U/L and Alk P 108 vs 91 vs 83 U/L]).
- Das N, Paul S, Chatterjee D, Banerjee N, Majumder NS, Sarma N, Sau TJ, Basu S, et al. Arsenic exposure through drinking water increases the risk of liver and cardiovascular diseases in the population of West Bengal, India. BMC Public Health 2012; 12: 639. [PMC free article: PMC3441389] [PubMed: 22883023](Comparison of 103 Bengali villagers with high arsenic drinking water exposure to 107 with low exposure found higher mean levels of ALT [37 vs 32 U/L] and Alk P [274 vs 217 U/L] in the higher arsenic exposed group).
- Lin HJ, Sung TI, Chen CY, Guo HR. Arsenic levels in drinking water and mortality of liver cancer in Taiwan. J Hazard Mater 2013 Nov 15; 262: 1132-8. [PubMed: 23352725](Analysis of arsenic levels in drinking water and mortality rates for liver cancer between 1971 and 1990 in 1103 persons from 138 villages in Taiwan found a positive association with liver cancer rates and arsenic levels in water above 640 µg/L, but not at lower levels of exposure).
- Hong YS, Song KH, Chung JY. Health effects of chronic arsenic exposure. J Prev Med Public Health 2014; 47: 245-52. [PMC free article: PMC4186552] [PubMed: 25284195](Review of the complications of chronic arsenic exposure including skin, lung, bladder, liver and prostate cancer, leukemia, neurologic effects, diabetes, skin conditions, cardiovascular disease and reproduction, but not liver disease or cirrhosis).
- Burnett AK, Russell NH, Hills RK, Bowen D, Kell J, Knapper S, Morgan YG, et al.; UK National Cancer Research Institute Acute Myeloid Leukaemia Working Group. Arsenic trioxide and all-trans retinoic acid treatment for acute promyelocytic leukaemia in all risk groups (AML17): results of a randomised, controlled, phase 3 trial. Lancet Oncol 2015; 16: 1295-305. [PubMed: 26384238](Have).
- Wang H, Liu Y, Wang X, Liu D, Sun Z, Wang C, Jin G, Zhang B, Yu S. Randomized clinical control study of locoregional therapy combined with arsenic trioxide for the treatment of hepatocellular carcinoma. Cancer 2015; 121: 2917-25. [PubMed: 26033499](Have).
- Liu B, Huang JW, Li Y, Hu BS, He X, Zhao W, Zheng YB, et al. Arsenic trioxide transarterial chemoembolization with and without additional intravenous administration of arsenic trioxide in unresectable hepatocellular carcinoma with lung metastasis: a single-blind, randomized trial. J Cancer Res Clin Oncol 2015; 141: 1103-8. [PubMed: 25504506](Have).
- Duncan A, Taylor A, Leese E, Allen S, Morton J, McAdam J. Homicidal arsenic poisoning. Ann Clin Biochem 2015; 52 (Pt 4): 510-5. [PubMed: 25344454](Have).
- Goel A, Christudoss P, George R, Ramakrishna B, Amirtharaj GJ, Keshava SN, Ramachandran A, et al. Arsenicosis, possibly from contaminated groundwater, associated with noncirrhotic intrahepatic portal hypertension. Indian J Gastroenterol 2016; 35: 207-15. [PubMed: 27225799](Have).
- Hsu LI, Wang YH, Hsieh FI, Yang TY, Wen-Juei Jeng R, Liu CT, Chen CL, Hsu KH, Chiou HY, Wu MM, Chen CJ. Effects of arsenic in drinking water on risk of hepatitis or cirrhosis in persons with and without chronic viral hepatitis. Clin Gastroenterol Hepatol 2016; 14: 1347-55.e4. [PubMed: 27060428](Have).
- Cappelletti R, Ceppi M, Claudatus J, Gennaro V. Health status of male steel workers at an electric arc furnace (EAF) in Trentino, Italy. J Occup Med Toxicol 2016; 11: 7. [PMC free article: PMC4761198] [PubMed: 26900394](Have).
- Li Y, Ye F, Wang A, Wang D, Yang B, Zheng Q, Sun G, Gao X. Chronic Arsenic Poisoning probably caused by arsenic-based pesticides: findings from an investigation study of a household. Int J Environ Res Public Health 2016; 13. pii: E133. [PMC free article: PMC4730524] [PubMed: 26784217](Have).
- Lin YC, Lian IB, Kor CT, Chang CC, Su PY, Chang WT, Liang YF, Su WW, Soon MS. Association between soil heavy metals and fatty liver disease in men in Taiwan: a cross sectional study. BMJ Open 2017; 7: e014215. [PMC free article: PMC5278238] [PubMed: 28115335](Have).
- Hu HT, Yao QJ, Meng YL, Li HL, Zhang H, Luo JP, Guo CY, Geng X. Arsenic trioxide intravenous infusion combined with transcatheter arterial chemoembolization for the treatment of hepatocellular carcinoma with pulmonary metastasis: Long-term outcome analysis. J Gastroenterol Hepatol 2017; 32: 295-300. [PubMed: 27517972](Have).
- Kumthekar P, Grimm S, Chandler J, Mehta M, Marymont M, Levy R, Muro K, et al. A phase II trial of arsenic trioxide and temozolomide in combination with radiation therapy for patients with malignant gliomas. Neurooncol 2017; 133: 589-94. [PubMed: 28510787](Have).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Arsenicosis: review of recent advances.[J Assoc Physicians India. 2010]Arsenicosis: review of recent advances.Pimparkar BD, Bhave A. J Assoc Physicians India. 2010 Oct; 58:617-24, 629.
- Associations between and risks of trace elements related to skin and liver damage induced by arsenic from coal burning.[Ecotoxicol Environ Saf. 2021]Associations between and risks of trace elements related to skin and liver damage induced by arsenic from coal burning.Hu Y, Xiao T, Zhang A. Ecotoxicol Environ Saf. 2021 Jan 15; 208:111719. Epub 2020 Dec 8.
- Arsenic: a beneficial therapeutic poison - a historical overview.[Adler Mus Bull. 2009]Arsenic: a beneficial therapeutic poison - a historical overview.Thomas X, Troncy J. Adler Mus Bull. 2009 Jun; 35(1):3-13.
- Review Strategies for safe and effective therapeutic measures for chronic arsenic and lead poisoning.[J Occup Health. 2005]Review Strategies for safe and effective therapeutic measures for chronic arsenic and lead poisoning.Kalia K, Flora SJ. J Occup Health. 2005 Jan; 47(1):1-21.
- Review The duplicitous nature of inorganic arsenic.[Mol Interv. 2005]Review The duplicitous nature of inorganic arsenic.Scheindlin S. Mol Interv. 2005 Apr; 5(2):60-4.
- Arsenic - LiverToxArsenic - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...