NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
The combination of ampicillin and sulbactam sodium combines a third generation aminopenicillin and a beta-lactamase inhibitor and is used to treat serious bacterial infections due to susceptible organisms. Given parenterally, ampicillin and sulbactam can cause mild transient aminotransferase elevations and has been linked to very rare instances of acute liver injury.
Background
The combination of ampicillin (am" pi sil' in) with sulbactam (sul bak' tam) is a parenterally administered, broad spectrum, potent antibiotic which combines a third generation, aminopenicillin with a beta lactamase inhibitor. This combination was approved for use in the United States in 1986. Current indications are for moderate-to-severe skin and skin structure, intra-abdominal and gynecological infections due to susceptible gram-positive and gram-negative bacteria, including beta-lactamase-producing strains of Staphylococcus aureus, Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, Bacteroides species, Enterobacter species, Neisseria meningitidis and gonorrhoeae, Moraxella catarrhalis and Acinetobacter calcoaceticus. The combination of ampicillin and sulbactam is available in a parenteral form generically and previously under the name Unasyn. The typical dose is 1.5 to 3 grams intramuscularly or intravenously every 6 hours for 7 to 14 days. Common side effects include diarrhea, nausea and vomiting, fatigue, headache, local reactions and rash. Rare but potentially serious adverse events include hypersensitivity reactions, anaphylaxis, severe skin rash, Stevens Johnson syndrome, C. difficile diarrhea, neutropenia, aplastic anemia and thrombocytopenic purpura.
Hepatotoxicity
Parenteral therapy with ampicillin-sulbactam has been reported to cause transient low level elevations in serum aminotransferase levels in 5% to 10% of patients, but these resolve rapidly once the therapy is stopped, and similar rates of enzyme elevations are found with comparable agents. Clinically apparent liver injury due to ampicillin-sulbactam is rare; instances have been published in individual case reports only. The reactions have been attributed to ampicillin rather than sulbactam and resemble the hepatic injury that occurs with ampicillin or amoxicillin alone. The liver injury is typically abrupt with short latency period and cholestatic features. The onset of hepatic injury may be accompanied by eosinophilia, arthralgias and skin rash, and occasionally with toxic epidermal necrolysis or Stevens-Johnson syndrome. The injury is usually self-limited in course, but fatal instances have been reported to the sponsor.
Likelihood score: C (probable rare cause of clinically apparent liver injury).
Mechanism of Injury
The cause of the liver injury associated with ampicillin use is probably hypersensitivity or allergy. Recurrence of hepatic injury has been reported after ampicillin induced liver injury with reexposure.
Outcome and Management
In the few cases that have been described, most patients have recovered although recovery has been slow in some cholestatic instances (2 to 6 months) and may be followed by persistent elevations in serum alkaline phosphatase. Acute liver failure and vanishing bile duct syndrome have been reported with aminopenicillin induced liver injury, but not specifically with ampicillin-sulbactam. Corticosteroids have often been used to treat the allergic manifestations of penicillin related immunoallergic hepatitis; while corticosteroid therapy may improve fever and rash promptly, their efficacy in ameliorating the accompanying liver disease has not been shown. Instances of recurrence of liver injury with reexposure to aminopenicillins and recurrence with exposure to cephalosporins have been reported. Patients with aminopenicillin induced hepatitis should avoid reexposure to other penicillins and should take cephalosporins with caution.
Other references relevant to the hepatotoxicity and safety of ampicillin-sulbactam are given in the chapter on ampicillin alone.
Drug Class: Antiinfective Agents, Aminopenicillins
Other Drugs in the Subclass, Aminopenicillins: Amoxicillin, Amoxicillin-Clavulanate, Ampicillin, Bacampicillin, Pivampicillin
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Ampicillin-Sulbactam – Generic, Unasyn®
DRUG CLASS
Antiinfective Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Ampicillin-Sulbactam | 94935-63-4 | C16-H19-N3-O4.S C8-H11-N-O5-S |
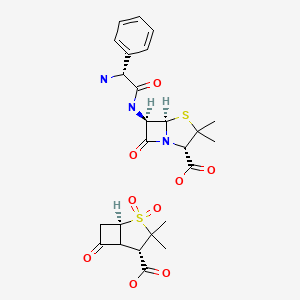
|
ANNOTATED BIBLIOGRAPHY
References updated: 20 October 2020
- Zimmerman HJ. Penicillins. In, Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott Williams and Wilkins, 1999. p. 595-6.(Expert review of penicillins and liver injury published in 1999; the penicillins commonly lead to hypersensitivity reactions but rarely to liver injury).
- Moseley RH. Hepatotoxicity of antimicrobials and antifungal agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 463-82.(Review of hepatotoxicity of antibiotics mentions that penicillins rarely cause liver injury and both hepatocellular and cholestatic patterns of injury have been described).
- McArthur JE, Dyment PG. Stevens-Johnson syndrome with hepatitis following therapy with ampicillin and cephalexin. N Z Med J. 1975;81:390–2. [PubMed: 1057088](Stevens-Johnson syndrome developed in a 9 month old child given ampicillin [rash] and cephalexin, with subsequent hepatocellular injury [bilirubin 13 mg/dL], resolving with prednisone therapy).
- Lees L, Milson JA, Knirsch AK, Greenhalgh K. Sulbactam plus ampicillin: interim review of efficacy and safety for therapeutic and prophylactic use. Rev Infect Dis. 1986;8 Suppl 5:S644–S650. [PubMed: 3026019](Review of 45 studies of ampicillin-sulbactam in 899 patients found successful outcome in 92%; ALT elevations in 6.9%, AST in 6.2%, but all resolved with stopping and similar rates were reported with use of comparative agents).
- Galante D, Esposito S, Barba D, Ruffilli MP. Clinical efficacy and safety of sulbactam/ampicillin in patients suffering from chronic liver disease. J Antimicrob Chemother. 1987;19:527–32. [PubMed: 3034850](41 patients with advanced liver disease were given sulbactam/ampicillin; there was no worsening of liver disease or enzyme elevations attributed to medication).
- Friis H, Andreasen PB. Drug-induced hepatic injury: an analysis of 1100 cases reported to the Danish Committee on Adverse Drug Reactions between 1978 and 1987. J Intern Med. 1992;232:133–8. [PubMed: 1506809](Adverse drug reaction reports in Denmark from 1978 to 1987; no mention of aminopenicillins).
- Köklü S, Köksal AS, Asil M, Kiyici H, Coban S, Arhan M. Probable sulbactam/ampicillin-associated prolonged cholestasis. Ann Pharmacother. 2004;38:2055–8. [PubMed: 15494387](74 year old developed cholestatic hepatitis arising 1 week after 7 day course of ampicillin-sulbactam with prolonged jaundice [bilirubin 31 mg/dL, ALT 33 U/L, Alk P 519 U/L], resolving after 7 months, except mild GGT elevations).
- Russo MW, Galanko JA, Shrestha R, Fried MW, Watkins P. Liver transplantation for acute liver failure from drug-induced liver injury in the United States. Liver Transpl. 2004;10:1018–23. [PubMed: 15390328](Among ~50,000 liver transplants done in the US between 1990 and 2002, 270 [0.5%] were done for drug induced acute liver failure; one case was attributed to amoxicillin-clavulanate, but none to penicillin, ampicillin or amoxicillin).
- Devarbhavi H, Dierkhising R, Kremers WK, Sandeep MS, Karanth D, Adarsh CK. Single-center experience with drug-induced liver injury from India: causes, outcome, prognosis, and predictors of mortality. Am J Gastroenterol. 2010;105:2396–404. [PubMed: 20648003](313 cases of drug induced liver injury were seen over a 12 year period at a large hospital in Bangalore, India; 3 [1%] were attributed to the combination of amoxicillin and clavulanate, but none were attributed to ampicillin or amoxicillin alone].
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury including 66 due to antimicrobial agents, including two attributed to amoxicillin but none to ampicillin; no details given).
- Ferrajolo C, Capuano A, Verhamme KM, Schuemie M, Rossi F, Stricker BH, Sturkenboom MC. Drug-induced hepatic injury in children: a case/non-case study of suspected adverse drug reactions in VigiBase. Br J Clin Pharmacol. 2010;70:721–8. [PMC free article: PMC2997312] [PubMed: 21039766](Worldwide pharmacovigilance database contained 9036 hepatic adverse drug reactions in children, amoxicillin-clavulanate accounted for 38 cases [0.4%] for an adjusted odds ratio of 1.7, whereas neither amoxicillin alone or ampicillin were listed among the 41 most common causes [linked to at least 30 cases]).
- Köksal AS, Yildiz H, Onder O, Avci S, Kayaåetin E. Sulbactam/ampicillin associated hepatocellular type liver injury. Acta Gastroenterol Belg. 2012;75:66–7. [PubMed: 22567755](47 year old woman developed jaundice 8 days after a 4 day course of ampicillin-sulbactam [bilirubin 18.9 mg/dL, ALT 1344 U/L, Alk P 208 U/L], resolving within 10 weeks of stopping).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, the most commonly implicated agent being amoxicillin with clavulanate [15 cases]; none were attributed to amoxicillin alone or ampicillin).
- Sistanizad M, Peterson GM. Drug-induced liver injury in the Australian setting. J Clin Pharm Ther. 2013;38:115–20. [PubMed: 23350857](Among 17 cases of suspected drug induced liver injury seen at a single referral hospital in Tasmania over a 12 month period, 11 were due to antibiotics including flucloxacillin in 4, amoxicillin in 2, amoxicillin-clavulanate in 2, and rifampin, moxifloxacin and ciprofloxacin in 1 each; none were attributed to ampicillin).
- Ferrajolo C, Verhamme KM, Trifirò G, 't Jong GW, Giaquinto C, Picelli G, Oteri A, et al. Idiopathic acute liver injury in paediatric outpatients: incidence and signal detection in two European countries. Drug Saf. 2013;36:1007–16. [PubMed: 23591830](Analysis of 3 electronic healthcare databases from Italy and the Netherlands from 2000-2008 identified 785 cases of unexplained acute liver injury in children, linked to 110 possible medications, with increased adjusted relative risk [RR] of recent exposure to amoxicillin-clavulanate [RR=18.6] and amoxicillin [RR=7.5]; no mention of ampicillin).
- Kaye JA, Castellsague J, Bui CL, Calingaert B, McQuay LJ, Riera-Guardia N, Saltus CW, et al. Risk of acute liver injury associated with the use of moxifloxacin and other oral antimicrobials: a retrospective, population-based cohort study. Pharmacotherapy. 2014;34:336–49. [PMC free article: PMC4260122] [PubMed: 24865821](In a US healthcare database with 1.3 million antimicrobial users, there were 607 cases of liver injury and 11 cases of liver failure, the highest relative risk for current single use being 3.2 for levofloxacin, 2.5 for amoxicillin-clavulanate, 2.5 for doxycycline, 2.3 for moxifloxacin and 2.3 for amoxicillin; no information provided on ampicillin).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury from Latin American countries published between 1996 and 2012 identified 176 cases, of which 37 [19%] were attributed to antimicrobials, including one to benzathine penicillin and 3 to amoxicillin-clavulanate, but none to ampicillin or 2nd or 4th generation penicillins).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 323 [36%] were attributed to antibiotics of which 106 [12%] were due to penicillins including one to 1st, three to 2nd [all due to oxacillin], 97 to 3rd [91 to amoxicillin-clavulanate, and 6 to amoxicillin alone] and five to 4th generation penicillins [all 5 to piperacillin/tazobactam]).
- Guéant JL, Romano A, Cornejo-Garcia JA, Oussalah A, Chery C, Blanca-López N, Guéant-Rodriguez RM, et al. HLA-DRA variants predict penicillin allergy in genome-wide fine-mapping genotyping. J Allergy Clin Immunol. 2015;135:253–9. [PubMed: 25224099](In a genome wide association study of 387 patients with immediate allergic reactions to beta-lactam antibiotics, several class 2 HLA associations [HLA-DRA regions] were found for penicillin responses, but they did not apply to cephalosporin cases).
- Nicoletti P, Aithal GP, Björnsson ES, Andrade RJ, Sawle A, Arrese M, Barnhart HX, et al. International Drug-Induced Liver Injury Consortium, Drug-Induced Liver Injury Network Investigators, and International Serious Adverse Events Consortium. Association of liver injury from specific drugs, or groups of drugs, with polymorphisms in HLA and other genes in a genome-wide association study. Gastroenterology. 2017;152:1078–89. [PMC free article: PMC5367948] [PubMed: 28043905](A genome wide association study done on 862 Caucasian patients with drug induced liver injury demonstrated a strong link with HLA-A*33:01 in those with cholestatic liver injury, particularly in cases attributed to terbinafine, fenofibrate and ticlopidine).
- Blumenthal KG, Youngster I, Rabideau DJ, Parker RA, Manning KS, Walensky RP, Nelson SB. Peripheral blood eosinophilia and hypersensitivity reactions among patients receiving outpatient parenteral antibiotics. J Allergy Clin Immunol. 2015;136:1288–94.e1. [PMC free article: PMC4640981] [PubMed: 25981739](Among 824 patients who underwent outpatient parenteral antibiotic therapy for at least 2 weeks, 210 [25%] developed eosinophilia including 58 of 207 [28%] who received “penicillins” of whom 3 developed signs of “possible” DRESS syndrome; specific penicillins accounting for the cases were not provided).
- Cirulli ET, Nicoletti P, Abramson K, Andrade RJ, Björnsson ES, Chalasani N, Fontana RJ, et al. Drug-Induced Liver Injury Network (DILIN) investigators. International DILI consortium (iDILIC). A missense variant in PTPN22 is a risk factor for drug-induced liver injury. Gastroenterology. 2019;156:1707–16.e2. [PMC free article: PMC6511989] [PubMed: 30664875](Genome wide association studies on 2048 patients with drug induced liver injury and 12,439 controls identified a variant in PTPN22 which was highly associated with liver injury, allele frequency being 0.12 among cases and 0.08 among controls with highest association in Northern Europeans and in cases of amoxicillin clavulanate, PTPN22 being a cellular kinase involved in modulation of immune reactions).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Ampicillin.[LiverTox: Clinical and Researc...]Review Ampicillin.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Amoxicillin.[LiverTox: Clinical and Researc...]Review Amoxicillin.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Penicillins (3rd Generation).[LiverTox: Clinical and Researc...]Review Penicillins (3rd Generation).. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Penicillins (4th Generation).[LiverTox: Clinical and Researc...]Review Penicillins (4th Generation).. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- In vitro activity against clinically important gram-positive and gram-negative bacteria of sulbactam, alone and in combination with ampicillin, cefotaxime, mezlocillin, and piperacillin.[Arzneimittelforschung. 1990]In vitro activity against clinically important gram-positive and gram-negative bacteria of sulbactam, alone and in combination with ampicillin, cefotaxime, mezlocillin, and piperacillin.Schmalreck AF, Wildfeuer A. Arzneimittelforschung. 1990 Oct; 40(10):1145-55.
- Ampicillin-Sulbactam - LiverToxAmpicillin-Sulbactam - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...