NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Zonisamide is a new generation anticonvulsant that is typically used in combination with other antiepileptic medications for partial onset seizures. Zonisamide has not been associated with elevations in serum aminotransferase levels and clinically apparent drug induced liver disease has been reported with its use but is very rare.
Background
Zonisamide (zoe nis' a mide) is synthetic sulfonamide derivative related somewhat in structure to acetazolamide, but not to other anticonvulsant medications. Zonisamide appears to block the spread of seizure discharges by affecting repetitive firing of voltage-sensitive sodium and calcium channels and stabilizing neuronal membranes. Zonisamide was approved for use in epilepsy in Japan in 1989 and in the United States in 2000. Current indications include adjunctive therapy for partial seizures in adults. Zonisamide is used off-label for therapy of migraine headaches, mood disturbances and recently for weight loss. Zonisamide is available as capsules of 25, 50 and 100 mg generically and under the brand name of Zonegran. The recommended initial dose in adults with epilepsy is 100 mg in one or two doses daily, with dose escalation based upon tolerance and effect to a maximum of 200 mg twice daily. Common side effects include drowsiness, dizziness, headache, nausea, poor appetite and weight loss. Rare, but serious side effects include Stevens-Johnson syndrome, toxic epidermal necrolysis, aplastic anemia and agranulocytosis.
Hepatotoxicity
Prospective studies suggest that chronic zonisamide therapy may be accompanied by mild increases in serum alkaline phosphatase levels, but it has not been linked to significant increases in serum aminotransferase levels during treatment. Clinically apparent hepatotoxicity from zonisamide is rare, but several case reports of hepatic injury linked to zonisamide have been published. Zonisamide is typically used in combination with other anticonvulsants and its separate role in causing liver injury is often difficult to delineate. Zonisamide has been linked to a single case report of cholestatic hepatitis associated with vanishing bile duct syndrome that ultimately resolved. More commonly, zonisamide has been linked to cases of hypersensitivity (DRESS syndrome or Stevens-Johnson syndrome) with rash, fever, eosinophilia, renal failure and/or mild liver test abnormalities. In most instances, the hepatic injury was cholestatic and arose 3 to 8 weeks after starting therapy. Autoantibodies are usually not present. Interestingly, a similar cholestatic liver injury has been described in dogs receiving zonisamide.
Likelihood score: D (possible rare cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism of zonisamide hepatotoxicity is unknown but is likely to be hypersensitivity. Cases of drug hypersensitivity to zonisamide have been linked to HLA-A*02:07 in Japanese subjects.
Outcome and Management
A few cases of cholestatic liver injury attributed to zonisamide has been published, with complete recovery in most patients but with persistent liver test abnormalities in at least one patient. Zonisamide has not been linked to acute liver failure or chronic liver injury. Patients who develop the anticonvulsant hypersensitivity syndrome should avoid other aromatic anticonvulsants or start them only with careful monitoring. Hypersensitivity reactions to anticonvulsants including zonisamide may benefit from corticosteroid therapy, but the efficacy of such therapy in altering the outcome of liver injury has not been proven.
Drug Class: Anticonvulsants
CASE REPORT
Case 1. Cholestatic hepatitis and bile duct injury attributed to zonisamide.(1)
An obese 35 year old man was being treated with phentermine and topiramate for weight loss. When switched from topiramate to zonisamide, he developed fatigue, dark urine and abdominal pain followed by jaundice and itching. After 3 weeks of symptoms, laboratory testing showed significant elevations in serum bilirubin, ALT and alkaline phosphatase levels (Table). There was no rash or fever. Tests for hepatitis A, B and C and for autoantibodies were negative. Abdominal ultrasound showed echogenicity of the liver compatible with hepatic steatosis, but no evidence of biliary obstruction. Endoscopic retrograde cholangiopancreatography was normal and a liver biopsy showed cholestasis with paucity of bile ducts. He persisted in having elevations in serum enzymes and underwent repeat liver biopsies 3 and 7 months after presentation, which showed ductular proliferation and improvement in cholestasis.
Key Points
| Medication: | Zonisamide (dose not provided) |
|---|---|
| Pattern: | Mixed→Cholestatic (R=2.3, initially; later R <1.0) |
| Severity: | 3+ (jaundice and hospitalization) |
| Latency: | 3 weeks |
| Recovery: | Incomplete; alkaline phosphatase still elevated one year later |
| Other medications: | Phentermine, topiramate (stopped 3 weeks earlier) |
Laboratory Values
| Time After Starting | Time After Stopping | ALT (U/L) | Alk P (U/L) | Bilirubin (mg/dL) | Other |
|---|---|---|---|---|---|
| 3 weeks | 0 | 531 | 578 | 7.1 | |
| 4 weeks | 1 week | 240 | 490 | 9.0 | |
| 5 weeks | 2 week | 270 | 390 | 9.5 | Biopsy #1 |
| 6 weeks | 3 week | 100 | 320 | 8.2 | |
| 7 weeks | 4 week | 80 | 300 | 7.3 | |
| 11 weeks | 8 week | 90 | 320 | 5.6 | |
| 13 weeks | 10 weeks | 200 | 420 | 3.0 | |
| 15 weeks | 12 weeks | 110 | 510 | 2.0 | |
| 21 weeks | 18 weeks | 75 | 340 | 1.7 | Biopsy #2 |
| 6 months | 5 months | 105 | 440 | 1.2 | |
| 1 year | 11 months | 120 | 640 | 0.9 | Biopsy #3 |
| Normal Values | <50 | <125 | <1.2 | ||
Comment
This was a well documented example of cholestatic hepatitis presenting with histological features of bile duct injury and loss which evolved into a partially reversible bile duct vanishing syndrome. The patient had persistence of serum enzyme elevations and chronic ductular injury with decrease in numbers of bile ducts that was still present almost a year after onset. The injury was attributed to zonisamide, but the patient had also received topiramate that was withdrawn shortly before onset of symptoms and may have played a role in this injury. The ultimate prognosis of vanishing bile duct syndrome is variable; some patients appear to recover, others develop chronic cholestasis and cirrhosis, requiring liver transplantation.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Zonisamide – Generic, Zonegran®
DRUG CLASS
Anticonvulsants
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
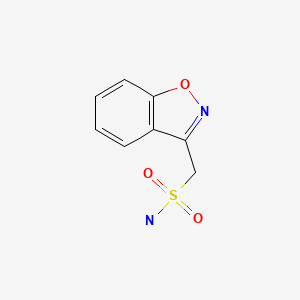
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Zonisamide | 68291-97-4 | C8-H8-N2-O3-S |
|
CITED REFERENCE
- 1.
- Vuppalanchi R, Chalasani N, Saxena R. Restoration of bile ducts in drug-induced vanishing bile duct syndrome due to zonisamide. Am J Surg Pathol. 2006;30:1619–23. [PubMed: 17122520]
ANNOTATED BIBLIOGRAPHY
References updated: 31 July 2020
Abbreviations used: DRESS, drug rash with eosinophilia and systemic symptoms; SJS/TEN, Stevens-Johnson syndrome and toxic epidermal necrolysis.
- Zimmerman HJ. Anticonvulsants. In, Zimmerman, HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999: pp. 498-516.(Expert review of anticonvulsants and liver injury published in 1999; zonisamide is not mentioned).
- Pirmohamed M, Leeder SJ. Anticonvulsant agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013: pp 423-41.(Review of anticonvulsant induced liver injury does not specifically discuss zonisamide).
- Smith MD, Metcalf CS, Wilcox KS. Pharmacology of the epilepsies. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 303-26.(Textbook of pharmacology and therapeutics).
- Natsch S, Hekster YA, Keyser A, Deckers CL, Meinardi H, Renier WO. Newer anticonvulsant drugs: role of pharmacology, drug interactions and adverse reactions in drug choice. Drug Saf. 1997;17:228–40. [PubMed: 9352959](Review of pharmacology, drug interactions and adverse effects anticonvulsants introduced after 2007, including felbamate, gabapentin, lamotrigine, oxcarbazepine, topiramate and zonisamide; no mention of hepatotoxicity of zonisamide).
- Knowles SR, Shapiro LE, Shear NH. Anticonvulsant hypersensitivity syndrome: incidence, prevention and management. Drug Saf. 1999;21:489–501. [PubMed: 10612272](Review of anticonvulsant hypersensitivity syndrome: triad of fever, rash and internal organ injury occurring 1-8 weeks after exposure to anticonvulsant; liver being most common internal organ involved. Occurs in 1:1000-1:10,000 initial exposures to phenytoin, carbamazepine, phenobarbital or lamotrigine, unrelated to dose, perhaps predisposed by valproate; liver injury arises 1-4 weeks after onset of rash and ranges in severity from asymptomatic ALT elevations to icteric hepatitis to acute liver failure. High mortality rate with jaundice; other organs include muscle, kidney, brain, heart and lung. Role of corticosteroids uncertain; cross reactivity among the aromatic anticonvulsant agents should be assumed, but not with zonisamide).
- Hamer HM, Morris HH. Hypersensitivity syndrome to antiepileptic drugs: a review including new anticonvulsants. Cleve Clin J Med. 1999;66:239–45. [PubMed: 10199060](Clinical review of anticonvulsant hypersensitivity syndrome, which occurs in 1-5/10,000 of users, higher risk in African Americans and affected siblings; liver involvement common, but most cases are anicteric; other manifestations include facial edema, lymphadenopathy, bone marrow aplasia, pseudolymphoma, thyroiditis, interstitial nephritis; switching to valproate and benzodiazepines is safe, zonisamide is also an option).
- Leppik IE. Zonisamide: chemistry, mechanism of action, and pharmacokinetics. Seizure. 2004;13 Suppl 1:S5–9. [PubMed: 15511691](Review of the pharmacology and pharmacokinetics of zonisamide).
- Vuppalanchi R, Chalasani N, Saxena R. Restoration of bile ducts in drug-induced vanishing bile duct syndrome due to zonisamide. Am J Surg Pathol. 2006;30:1619–23. [PubMed: 17122520](35 year old obese man developed fatigue and dark urine shortly after starting zonisamide and 3 weeks later had jaundice and itching [bilirubin 7.1 mg/dL, ALT 531 U/L, Alk P 531], biopsy showing bile duct loss, Alk P and ALT were still abnormal 10 months later; patient also had received topiramate 3 weeks before presentation: Case 1).
- LaRoche SM. A new look at the second-generation antiepileptic drugs: a decade of experience. Neurologist. 2007;13:133–9. [PubMed: 17495757](Review of second generation anticonvulsants approved since 1994 including felbamate, gabapentin, lamotrigine, topiramate, tiagabine, levetiracetam, oxcarbazepine, zonisamide and pregabalin; zonisamide associated with kidney stones, but no mention of liver toxicity).
- Björnsson E. Hepatotoxicity associated with antiepileptic drugs. Acta Neurol Scand. 2008;118:281–90. [PubMed: 18341684](Review of all anticonvulsants; suggests that there have been no cases of hepatoxicity associated with zonisamide).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, valproate accounted for 6, lamotrigine 5, phenytoin 5, gabapentin and topiramate 1 each; zonisamide not mentioned).
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury including 11 due to anticonvulsants, 8 from phenytoin, 2 valproate and 3 carbamazepine, but none were attributed to lamotrigine, levetiracetam, topiramate, or zonisamide).
- Fujita Y, Hasegawa M, Nabeshima K, Tomita M, Murakami K, Nakai S, Yamakita T, Matsunaga K. Acute kidney injury caused by zonisamide-induced hypersensitivity syndrome. Intern Med. 2010;49:409–13. [PubMed: 20190474](29 year old man developed rash, facial edema and fever 2 months after starting zonisamide, with subsequent renal failure requiring dialysis and serum cholestatic enzyme elevations [bilirubin 0.4 mg/dL, ALT 88 U/L, Alk P 661 U/L, 26% eosinophils], with response to corticosteroid therapy and ultimate resolution).
- Schwartz M, Muñana KR, Olby NJ. Possible drug-induced hepatopathy in a dog receiving zonisamide monotherapy for treatment of cryptogenic epilepsy. J Vet Med Sci. 2011;73:1505–8. [PubMed: 21720107](9 year old female dog developed jaundice 3 weeks after starting zonisamide [bilirubin 4.3 mg/dL, ALT 1275 U/L, Alk P 5182 U/L], with full recovery within 4 weeks of stopping).
- Miller ML, Center SA, Randolph JF, Lepherd ML, Cautela MA, Dewey CW. Apparent acute idiosyncratic hepatic necrosis associated with zonisamide administration in a dog. J Vet Intern Med. 2011;25:1156–60. [PubMed: 21985145](4 year old male dog developed anorexia and vomiting 10 days after starting zonisamide for epilepsy [bilirubin 2.3 mg/dL, ALT 16,328 U/L, Alk P 354 U/L], with progressive multiorgan failure and death the next day, autopsy showing massive necrosis).
- Lu Y, Xiao Z, Yu W, Xiao F, Xiao Z, Hu Y, Chen Y, Wang X. Efficacy and safety of adjunctive zonisamide in adult patients with refractory partial-onset epilepsy: a randomized, double-blind, placebo-controlled trial. Clin Drug Investig. 2011;31:221–9. [PubMed: 21166480](Controlled trial of zonisamide in 104 patients with refractory epilepsy; liver enzyme elevations occurred in 35% of zonisamide- vs 37% of placebo-recipients and none developed clinically apparent liver injury).
- Uhara H, Saiki M, Kawachi S, Ashida A, Oguchi S, Okuyama R. Clinical course of drug-induced hypersensitivity syndrome treated without systemic corticosteroids. J Eur Acad Dermatol Venereol. 2013;27:722–6. [PubMed: 22540194](Series of 12 patients with drug induced hypersensitivity caused by carbamazepine [6], sulfonamide [4], mexiletine [1], and zonisamide [1]; in a 62 year old woman with a brain tumor who developed fever and rash 22 days after starting zonisamide [bilirubin and Alk P not given, ALT 240 U/L], resolving without therapy).
- Kaniwa N, Saito Y. Pharmacogenomics of severe cutaneous adverse reactions and drug-induced liver injury. J Hum Genet. 2013;58:317–26. [PubMed: 23635947](Review of genetic associations with severe skin and liver injury from drugs, focusing upon allopurinol [B*58:01], abacavir and flucloxacillin [B*57:01] and lapatinib [DQA1*02:01]; the association of B*15:02 with carbamazepine induced SJS has not been extended to carbamazepine induced liver injury; zonisamide not discussed).
- Sekula P, Dunant A, Mockenhaupt M, Naldi L, Bouwes Bavinck JN, Halevy S, Kardaun S, Sidoroff A, Liss Y, Schumacher M, Roujeau JC. Comprehensive survival analysis of a cohort of patients with Stevens-Johnson syndrome and toxic epidermal necrolysis. J Invest Dermatol. 2013;133:1197–204. [PubMed: 23389396](Analysis of mortality rates in 460 patients with SJS/TEN [67% due to drugs and 19% due to anticonvulsants] in a European observational database found that age, severity, underlying malignancy and renal or hepatic involvement correlated with poor survival; overall mortality at one year being 24% for SJS, 43% for overlap and 49% for TEN cases).
- Lee T, Lee YS, Yoon SY, Kim S, Bae YJ, Kwon HS, Cho YS, et al. Characteristics of liver injury in drug-induced systemic hypersensitivity reactions. J Am Acad Dermatol. 2013;69:407–15. [PubMed: 23632341](Analysis of 136 patients with hypersensitivity reactions to drugs seen at a single referral center in Korea found liver involvement in 61 [45%], including 11 with SJS/TEN, 29 with DRESS and 17 with rash only; 20 cases were attributed to anticonvulsants, but specific agents were not mentioned).
- Gaitatzis A, Sander JW. The long-term safety of antiepileptic drugs. CNS Drugs. 2013;27:435–55. [PubMed: 23673774](Review of the long term safety and adverse event profile of anticonvulsants mentions that valproate can cause fatty liver disease, but that most cases of clinically apparent liver injury including acute liver failure occur within the first few months of treatment with anticonvulsants such as valproate and felbamate).
- Kaniwa N, Sugiyama E, Saito Y, Kurose K, Maekawa K, Hasegawa R, Furuya H, et al. Japan Pharmacogenomics Data Science Consortium. Specific HLA types are associated with antiepileptic drug-induced Stevens-Johnson syndrome and toxic epidermal necrolysis in Japanese subjects. Pharmacogenomics. 2013;14:1821–31. [PubMed: 24236482](Analysis of HLA types among 12 Japanese patients with SJS/TEN due to zonisamide four 42% to have HLA-A*02:07 compared to 6.8% of controls).
- Drugs for epilepsy. Treat Guidel Med Lett. 2013;11:9–18. Erratum in Treat Guidel Med Lett 2013; 11: 112. [PubMed: 23348233](Concise review of drugs of choice for epilepsy; mentions that the adverse effects of zonisamide include fatal instances of toxic epidermal necrolysis and Stevens-Johnson syndrome).
- Shibuya R, Tanizaki H, Nakajima S, Koyanagi I, Kataoka TR, Miyachi Y, Kabashima K. DIHS/DRESS with remarkable eosinophilic pneumonia caused by zonisamide. Acta Derm Venereol. 2015;95:229–30. [PubMed: 24696158](46 year old woman developed rash, fever and cough 41 days after restarting zonisamide [bilirubin normal, ALT 133 U/L, Alk P 220 U/L, 11% eosinophils], resolving with prednisone therapy).
- Baulac M, Patten A, Giorgi L. Long-term safety and efficacy of zonisamide versus carbamazepine monotherapy for treatment of partial seizures in adults with newly diagnosed epilepsy: Results of a phase III, randomized, double-blind study. Epilepsia. 2014;55:1534–43. [PubMed: 25109239](Among 295 patients with partial seizures treated with either zonisamide or carbamazepine for 6 months, adverse events were similar with both drugs; no mention of ALT elevations or hepatotoxicity).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, 7 [4%] of which were attributed to anticonvulsants including 3 to phenytoin, 3 to valproate and 1 to carbamazepine, but none were attributed to zonisamide).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 40 [4.5%] were due to anticonvulsants including 12 due to phenytoin, 9 lamotrigine, 7 valproate, 4 carbamazepine, 3 gabapentin, 2 topiramate and 1 each for ethosuximide, fosphenytoin, and pregabalin).
- Lee HJ, Son JM, Mun J, Kim DW. Safety and efficacy of zonisamide in patients with epilepsy: a post-marketing surveillance study. J Epilepsy Res. 2015;5:89–95. [PMC free article: PMC4724857] [PubMed: 26819941](Among 1948 Korean adults treated with zonisamide and monitored in a postmarketing study, 65 patients [3.3%] reported an adverse event, 11 of which [0.5%] were considered serious, including one case of Stevens-Johnson syndrome; no mention of hepatotoxicity or ALT elevations).
- Dash A, Ravat S, Srinivasan AV, Shetty A, Kumar V, Achtani R, Mathur VN, et al. Evaluation of safety and efficacy of zonisamide in adult patients with partial, generalized, and combined seizures: an open labeled, noncomparative, observational Indian study. Ther Clin Risk Manag. 2016;12:327–34. [PMC free article: PMC4778773] [PubMed: 27013882](Among 655 adults with partial, generalized or combined seizures treated with zonisamide [add on to other agents in 79%] for 24 weeks, most patients had improvement in seizure control and adverse events included loss of appetite [7%], weight loss [4%], sedation [2%], dizziness [2%] and skin rash [<1%] but no mention of hepatotoxicity or ALT elevations).
- Vidaurre J, Gedela S, Yarosz S. Antiepileptic drugs and liver disease. Pediatr Neurol. 2017;77:23–36. [PubMed: 29097018](Review of the use of anticonvulsants in patients with liver disease recommends use of agents that have little hepatic metabolism such as levetiracetam, lacosamide, topiramate, gabapentin and pregabalin, levetiracetam, being an "ideal" first line therapy for patients with liver disease because of its safety and lack of pharmacokinetic interactions).
- Drugs for epilepsy. Med Lett Drugs Ther. 2017;59(1526):121–30. [PubMed: 28746301](Concise review of the drugs available for therapy of epilepsy mentions that zonisamide is approved as adjunctive therapy of partial seizures but has a broad spectrum of action, while common adverse events include somnolence, dizziness, confusion, anorexia, nausea, diarrhea, weight loss, agitation, irritability and rash, rare but severe events include Stevens-Johnson syndrome aplastic anemia, agranulocytosis, metabolic acidosis and renal stones).
- Borrelli EP, Lee EY, Descoteaux AM, Kogut SJ, Caffrey AR. Stevens-Johnson syndrome and toxic epidermal necrolysis with antiepileptic drugs: An analysis of the US Food and Drug Administration Adverse Event Reporting System. Epilepsia. 2018;59:2318–24. [PMC free article: PMC6420776] [PubMed: 30395352](Review of adverse event reports to the FDA between 2014 and 2018 identified ~2.9 million reports, 1034 for SJS/TEN, the most common class of drugs being anticonvulsants with 17 of 34 having at least one report, those most frequently linked being lamotrigine [n=106], carbamazepine [22], levetiracetam [14], phenytoin [14], valproate [9], clonazepam [8] and zonisamide [7]; no mention of accompanying liver injury or whether attribution was as a single agent or one of several).
- Han XD, Koh MJ, Wong SMY. Drug reaction with eosinophilia and systemic symptoms in a cohort of Asian children. Pediatr Dermatol. 2019;36:324–9. [PubMed: 30920020](Among 10 children with DRESS syndrome seen at a single, Singapore referral center between 2006 and 2016, 3 cases were attributed to sulfamethoxazole/trimethoprim, 2 to carbamazepine, 1 sulfasalazine, 2 phenobarbital, 1 to levetiracetam [latency 28 days] but none to zonisamide; all had ALT elevations [88 to 1172 U/L], bilirubin was elevated in 7, but none had acute liver failure and none were fatal).
- Cano-Paniagua A, Amariles P, Angulo N, Restrepo-Garay M. Epidemiology of drug-induced liver injury in a University Hospital from Colombia: Updated RUCAM being used for prospective causality assessment. Ann Hepatol. 2019;18:501–7. [PubMed: 31053545](Among 286 patients with liver test abnormalities seen in a single hospital in Colombia over a 1 year period, 17 were diagnosed with drug induced liver injury, the most common cause being antituberculosis therapy [n=6] followed by anticonvulsants [n=3, 1 each due to phenytoin, gabapentin and valproate]).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Levetiracetam.[LiverTox: Clinical and Researc...]Review Levetiracetam.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Brivaracetam.[LiverTox: Clinical and Researc...]Review Brivaracetam.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Zonisamide. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic potential in epilepsy.[Drugs. 1993]Review Zonisamide. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic potential in epilepsy.Peters DH, Sorkin EM. Drugs. 1993 May; 45(5):760-87.
- Review [Research and development of zonisamide, a new type of antiepileptic drug].[Yakugaku Zasshi. 1996]Review [Research and development of zonisamide, a new type of antiepileptic drug].Shimizu M, Uno H, Ito T, Masuda Y, Kurokawa M. Yakugaku Zasshi. 1996 Jul; 116(7):533-47.
- Zonisamide - a review of experience and use in partial seizures.[Neuropsychiatr Dis Treat. 2006]Zonisamide - a review of experience and use in partial seizures.Wilfong AA, Willmore LJ. Neuropsychiatr Dis Treat. 2006 Sep; 2(3):269-80.
- Zonisamide - LiverToxZonisamide - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...