NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Ruxolitinib is a small molecule Janus kinase inhibitor that is used in the treatment of intermediate or high risk myelofibrosis and resistant forms of polycythemia vera and graft-vs-host disease. Ruxolitinib is associated with transient and usually mild elevations in serum aminotransferase during therapy and to rare instances of self-limited, clinically apparent idiosyncratic acute liver injury as well as to cases of reactivation of hepatitis B in susceptible individuals.
Background
Ruxolitinib (rux” oh li’ ti nib) is an orally available, specific inhibitor of Janus kinase subtypes 1 and 2 (JAK1 and JAK2). JAK1 and JAK2 are non-receptor tyrosine kinases that are critical components of pathways that lead to production and secretion of hematologic growth factors and inflammatory cytokines. These pathways are important in hematologic cell differentiation and proliferation, intracellular signaling by interferon alpha and gamma, and in cytokine-production and inflammatory reactions. Mutations in JAK1 and JAK2 are frequent in patients with myelofibrosis, and inhibition of these kinases can result in antiproliferative and antiapoptotic effects in malignant cells. Ruxolitinib has been shown to improve symptoms, cause shrinkage of spleen size and decrease circulating cytokine levels in patients with myelofibrosis and polycythemia vera independent of the known presence of Janus kinase mutations. It has also been shown to be effective in both acute and chronic graft-vs-host disease. Ruxolitinib was approved for use in the United States in 2011 for therapy of intermediate and high risk myelofibrosis. Subsequently, indications were extended to include polycythemia vera resistant or intolerant to conventional therapy as well as corticosteroid-resistant acute and refractory chronic graft-vs-host disease. Ruxolitinib is currently available in tablets of 5, 10, 15, 20 and 25 mg under the brand name Jakafi. Typical doses of ruxolitinib range from 5 to 20 mg given orally twice daily. The recommended dose varies by indication and clinical status including platelet count and tolerance. Dose adjustments for liver or kidney dysfunction and for possible drug-drug interactions are also recommended. Common side effects include myelosuppression, anemia, thrombocytopenia, fatigue, diarrhea, bruising, dizziness, dyspnea, headache and peripheral edema. Sudden withdrawal of ruxolitinib is associated with rapid relapse of symptoms which can be severe with fever, respiratory distress, anemia and features of the systemic inflammatory response syndrome. Uncommon but potentially severe adverse reactions include reactivation of tuberculosis, hepatitis B and herpes zoster as well as severe thrombocytopenia, neutropenia and anemia, opportunistic infections, fetal and embryonal toxicity, and progressive multifocal leukoencephalopathy.
More recently, ruxolitinib has been evaluated as therapy for the hyperinflammatory state associated with SARS-CoV-2 infection and severe COVID-19 pneumonia. Results of these studies have not been released and only anecdotal reports of its use in patients with COVID-19 have been published.
Hepatotoxicity
In the large clinical trials, serum ALT elevations occurred in 25% to 48% of ruxolitinib treated subjects versus 7% to 9% of placebo recipients. The ALT elevations were generally self-limited, asymptomatic and mild and were above 5 times ULN in only 1.3% of patients. In the prelicensure clinical trials, no cases of clinically apparent liver injury were reported. Among causes of death in one trial of ruxolitinib for myelofibrosis, one was attributed to hepatic failure; this instance, however, was considered unrelated to ruxolitinib. Since its approval and more wide scale use, rare cases of clinically apparent ruxolitinib induced acute liver injury have been reported, but without documentation of clinical features or careful exclusion of other causes. Importantly, there also have been several published reports of reactivation of hepatitis B, in patients with and without HBsAg (but with anti-HBc) in serum. A rise in HBV DNA levels was identified within 1 to 6 months of starting ruxolitinib and was associated with elevations in ALT levels and jaundice in some patients. HBV DNA levels decreased rapidly upon starting anti-HBV therapy with entecavir and all patients recovered. In one instance, HBV DNA levels declined with lowering of the dose of ruxolitinib, but then rose again when the dose was increased.
So far, reports of the use of ruxolitinib for COVID-19 have included only small numbers of patients and have provided little information on hepatic adverse events or risk of reactivation of hepatitis B.
Likelihood score: C (probable cause of reactivation of hepatitis B in susceptible patients).
Mechanism of Injury
The causes of serum enzyme elevations during ruxolitinib therapy are not known. Ruxolitinib is metabolized in the liver largely through the CYP 3A4 pathway and liver injury may be related to production of a toxic intermediate. Ruxolitinib is susceptible to drug-drug interactions with agents that inhibit or induce hepatic CYP 3A4 activity. Because of its effects on intracellular signaling involved in immune responses, ruxolitinib (and possibly other JAK1 and JAK2 inhibitors) is capable to increasing HBV replication which can result in clinically apparent reactivation of hepatitis B.
Outcome and Management
Serum aminotransferase elevations above 5 times the upper limit of normal (if confirmed) or any elevations accompanied by jaundice or symptoms should lead to dose reduction or temporary cessation. There does not appear to be cross reactivity in risk for hepatic injury between ruxolitinib and other kinase inhibitors. Ruxolitinib is capable of causing reactivation of hepatitis B and other opportunistic infections and patients should be screened for evidence of HBV infection before starting chemotherapy, including testing for HBsAg and anti-HBc. Those who are reactive for these virologic markers should be tested for serum HBV DNA and be considered for prophylaxis against HBV reactivation with a nucleoside analog such as tenofovir or entecavir particularly if they are HBsAg-positive. Reactivation of hepatitis B with ruxolitinib therapy is rare in patients with anti-HBc without HBsAg in serum and such patients can be monitored for HBV DNA levels and therapy initiated with a significant rise (one or two log10 IU/mL compared to baseline).
Drug Class: Antineoplastic Agents, Protein Kinase Inhibitors, COVID-19 Drugs
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Ruxolitinib – Jakafi®
DRUG CLASS
Antineoplastic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
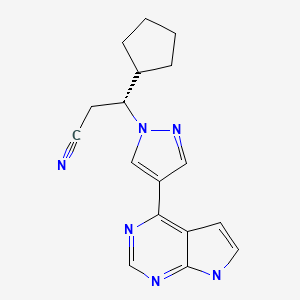
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Ruxolitinib | 941678-49-5 | C17-H18-N6 |
|
ANNOTATED BIBLIOGRAPHY
References updated: 30 August 2022
Abbreviations: EAP, early access programs; EUA, emergency use authorization; GvHD, graft-vs-host disease; HCT, hematopoietic cell transplantation; JAK, Janus kinase.
- Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999.(Review of hepatotoxicity published in 1999 before the availability of tyrosine kinase inhibitors such as ruxolitinib).
- DeLeve LD. Erlotinib. Cancer chemotherapy. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 556.(Review of hepatotoxicity of cancer chemotherapeutic agents discusses several tyrosine kinase inhibitors including imatinib, gefitinib, erlotinib and crizotinib, but not ruxolitinib).
- Wellstein A, Giaccone G, Atkins MB, Sausville EA. Pathway-targeted therapies: monoclonal antibodies, protein kinase inhibitors, and various small molecules. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1203-36.(Textbook of pharmacology and therapeutics).
- Verstovsek S, Kantarjian H, Mesa RA, Pardanani AD, Cortes-Franco J, Thomas DA, Estrov Z, et al. Safety and efficacy of INCB018424, a JAK1 and JAK2 inhibitor, in myelofibrosis. N Engl J Med. 2010;363:1117–27. [PMC free article: PMC5187954] [PubMed: 20843246](Among 153 patients with myelofibrosis treated with varying doses of ruxolitinib, the optimal regimen was 15 mg twice daily, with subsequent dose modifications, a regimen that yielded a 50% rapid, objective response regardless of JAK mutation status; side effects included dose related thrombocytopenia and anemia while nonhematologic side effects were uncommon [<6%] and included diarrhea, fatigue, headache, and peripheral edema; no mention of ALT elevations of hepatotoxicity).
- Tefferi A, Pardanani A. Serious adverse events during ruxolitinib treatment discontinuation in patients with myelofibrosis. Mayo Clin Proc. 2011;86:1188–91. [PMC free article: PMC3228619] [PubMed: 22034658](Among 47 patients with myelofibrosis who discontinued ruxolitinib treatment, most patients had an acute relapse of symptoms within a few days or weeks of stopping and 5 required hospitalization because of suspected systemic inflammatory response syndrome with high fevers, respiratory distress, thromboses and anemia, often responding to corticosteroid therapy).
- Verstovsek S, Mesa RA, Gotlib J, Levy RS, Gupta V, DiPersio JF, Catalano JV, et al. A double-blind, placebo-controlled trial of ruxolitinib for myelofibrosis. N Engl J Med. 2012;366:799–807. [PMC free article: PMC4822164] [PubMed: 22375971](In a study of 309 patients with intermediate or high risk myelofibrosis treated for up to 1 year, objective responses [reduction in spleen volume] occurred in 42% of ruxolitinib, but <1% of placebo treated subjects; adverse events more common with ruxolitinib included thrombocytopenia [70% vs 30%], anemia [96% vs 87%], bruising [19% vs 9%] and dizziness [15% vs <1%]; no mention of ALT elevations or hepatotoxicity).
- Ruxolitinib (Jakafi) for myelofibrosis. Med Lett Drugs Ther. 2012;54(1387):27–8. [PubMed: 22469651](Concise review of efficacy and safety of ruxolitinib as therapy for myelofibrosis, mentions severe withdrawal symptoms when the drug is stopped that may require corticosteroids).
- Harrison C, Kiladjian JJ, Al-Ali HK, Gisslinger H, Waltzman R, Stalbovskaya V, McQuitty M, et al. JAK inhibition with ruxolitinib versus best available therapy for myelofibrosis. N Engl J Med. 2012;366:787–98. [PubMed: 22375970](Among 219 patients with intermediate or high risk myelofibrosis treated with ruxolitinib or best available therapy for at least one year, improvement in clinical symptoms and shrinkage of spleen size occurred with ruxolitinib, but rarely without; listing of severe adverse events included one death from hepatic failure, but it was considered unrelated to ruxolitinib therapy).
- Verstovsek S, Mesa RA, Gotlib J, Levy RS, Gupta V, DiPersio JF, Catalano JV, et al. Efficacy, safety and survival with ruxolitinib in patients with myelofibrosis: results of a median 2-year follow-up of COMFORT-I. Haematologica. 2013;98:1865–71. [PMC free article: PMC3856961] [PubMed: 24038026](Among 155 patients with myelofibrosis treated with ruxolitinib, 100 continued on therapy with a median follow up of 2 years; most common side effects were dose related thrombocytopenia and anemia and nonhematologic side effects of bruising, headache and diarrhea; no mention of hepatotoxicity or ALT elevations).
- Kantarjian HM, Silver RT, Komrokji RS, Mesa RA, Tacke R, Harrison CN. Ruxolitinib for myelofibrosis--an update of its clinical effects. Clin Lymphoma Myeloma Leuk. 2013;13:638–45. [PMC free article: PMC5556922] [PubMed: 24238036](Review of the efficacy and safety of ruxolitinib as therapy of myelofibrosis, the major severe side effects being hematologic; no discussion of hepatotoxicity or ALT elevations).
- Spraggs CF, Xu CF, Hunt CM. Genetic characterization to improve interpretation and clinical management of hepatotoxicity caused by tyrosine kinase inhibitors. Pharmacogenomics. 2013;14:541–54. [PubMed: 23556451](Review of genetic associations of serum ALT and bilirubin elevations during therapy with tyrosine kinase inhibitors focusing on lapatinib and pazopanib).
- Shah RR, Morganroth J, Shah DR. Hepatotoxicity of tyrosine kinase inhibitors: clinical and regulatory perspectives. Drug Saf. 2013;36:491–503. [PubMed: 23620168](Review of the hepatotoxicity of 18 tyrosine kinase inhibitors approved for use in cancer in the US as of 2013; aminotransferase elevations occurred in 18% of patients in registration trials of ruxolitinib, but were rarely above 5 times ULN and cases of clinically apparent liver injury have not been reported).
- Cervantes F, Vannucchi AM, Kiladjian JJ, Al-Ali HK, Sirulnik A, Stalbovskaya V, McQuitty M, et al. COMFORT-II investigators. Three-year efficacy, safety, and survival findings from COMFORT-II, a phase 3 study comparing ruxolitinib with best available therapy for myelofibrosis. Blood. 2013;122:4047–53. [PubMed: 24174625](In a 3 year open label extension of a trial of ruxolitinib versus placebo in patients with myelofibrosis [Harrison 2012], 106 patients remained on ruxolitinib for an average of 3 years, responses were maintained with continuation of therapy and adverse events were mostly mild, the most common being diarrhea; no mention of ALT elevations or hepatotoxicity).
- Verstovsek S, Passamonti F, Rambaldi A, Barosi G, Rosen PJ, Rumi E, Gattoni E, et al. A phase 2 study of ruxolitinib, an oral JAK1 and JAK2 Inhibitor, in patients with advanced polycythemia vera who are refractory or intolerant to hydroxyurea. Cancer. 2014;120:513–20. [PMC free article: PMC4231215] [PubMed: 24258498](Among 34 patients with polycythemia vera treated with ruxolitinib, 97% had an objective response and side effects were not common and generally mild; no mention of ALT elevations or hepatotoxicity).
- Galli S, McLornan D, Harrison C. Safety evaluation of ruxolitinib for treating myelofibrosis. Expert Opin Drug Saf. 2014;13:967–76. [PubMed: 24896661](Review of the mode of action, pharmacology, clinical efficacy and safety of ruxolitinib does not discuss frequency of ALT elevations during therapy or clinically apparent hepatotoxicity).
- Caocci G, Murgia F, Podda L, Solinas A, Atzeni S, La Nasa G. Reactivation of hepatitis B virus infection following ruxolitinib treatment in a patient with myelofibrosis. Leukemia. 2014;28:225–7. [PubMed: 23929216](49 year old woman with thrombocytopenic myelofibrosis and HBsAg in serum [HBeAg and HBV DNA <10 IU/mL] developed rising levels of HBV DNA within 5 months of starting ruxolitinib [20 mg twice daily], decreasing with lowering dose [15 mg twice daily] and increasing again with full dose, but without liver test abnormalities [ALT normal, HBV DNA 38,300 IU/mL] and HBV DNA levels declining with lowering dose again).
- Shen CH, Hwang CE, Chen YY, Chen CC. Hepatitis B virus reactivation associated with ruxolitinib. Ann Hematol. 2014;93:1075–6. [PubMed: 24173089](72 year old man with essential thrombocythemia and HBsAg in serum [ALT 22 U/L] developed abnormal liver tests 8 months after starting ruxolitinib [peak bilirubin 1.8 mg/dL, ALT 291 U/L, HBV DNA 7 log10 copies/mL], resolving within 8 weeks of stopping ruxolitinib and 6 weeks of starting entecavir).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 49 were attributed to antineoplastic agents [5.5%], 3 of which were attributed to kinase inhibitors [imatinib, lapatinib], but none to ruxolitinib).
- Kirito K, Sakamoto M, Enomoto N. Elevation of the hepatitis B virus DNA during the treatment of polycythemia vera with the JAK kinase inhibitor ruxolitinib. Intern Med. 2016;55:1341–4. [PubMed: 27181544](64 year old woman with polycythemia vera [ALT normal, HBeAg negative, HBV DNA 5.4 log10 copies/mL] developed liver test abnormalities 1 month after starting ruxolitinib [bilirubin normal, ALT 352 U/L, HBV DNA 7.2 log10 copies/mL], responding within 2 weeks of starting entecavir with normal ALT and HBV DNA 3.6 log10 copies/mL).
- Perricone G, Vinci M, Pungolino E. Occult hepatitis B infection reactivation after ruxolitinib therapy. Dig Liver Dis. 2017;49:719. [PubMed: 28410914](Two men, ages 57 and 73 years, with polycythemia vera and anti-HBc without HBsAg in serum developed increasing levels of HBV DNA [from 39 to 840 IU/mL and <10 to 42.2 million IU/mL] 2 and 5 months after starting ruxolitinib, both responding to entecavir therapy, but one developing self-limited, but severe acute hepatitis).
- Tremblay D, Putra J, Vogel A, Winters A, Hoffman R, Schiano TD, Fiel MI, et al. The implications of liver biopsy results in patients with myeloproliferative neoplasms being treated with ruxolitinib. Case Rep Hematol. 2019;2019:3294046. [PMC free article: PMC6339753] [PubMed: 30723558](Description of 4 cases of liver injury associated with ruxolitinib therapy, 49 to 74 year old men with rising ALT or Alk P during therapy and liver biopsies showing extramedullary hematopoiesis attributed to the underlying myelofibrosis in 3 and granulomatous hepatitis with loss of bile ducts attributed to drug induced liver injury in one, but few details given).
- Foltz L, Pica GM, Zerazhi H, Van Droogenbroeck J, Visanica S, Báez de la Fuente E, Leber B, et al. Safety and efficacy findings from the open-label, multicenter, phase 3b, expanded treatment protocol study of ruxolitinib for treatment of patients with polycythemia vera who are resistant/intolerant to hydroxyurea and for whom no alternative treatments are available. Leuk Lymphoma. 2019;60:3493–502. [PubMed: 31359808](Among 161 patients with polycythemia vera enrolled in an expanded access study of ruxolitinib for a median follow up of 25 weeks, adverse events were common and led to dose interruption or reduction in 40% of patients, most common adverse events being anemia [32%], thrombocytopenia [7%], headache [25%], diarrhea [14%]; no mention of ALT elevations or hepatotoxicity).
- Lussana F, Cattaneo M, Rambaldi A, Squizzato A. Ruxolitinib-associated infections: a systematic review and meta-analysis. Am J Hematol. 2018;93:339–47. [PubMed: 29150886](Systematic review of the literature on infections arising during ruxolitinib therapy focusing largely on bacterial infections and herpes zoster, mentions that there have been 5 case reports of reactivation of hepatitis B).
- Gill H, Leung GMK, Seto WK, Kwong YL. Risk of viral reactivation in patients with occult hepatitis B virus infection during ruxolitinib treatment. Ann Hematol. 2019;98:215–8. [PubMed: 29946910](Among 40 Chinese patients with myelodysplastic disorders treated with ruxolitinib, 3 were HBsAg positive and were given prophylactic entecavir, and 17 had anti-HBc without HBsAg in serum and were monitored closely 4 developing evidence of reactivation with de novo appearance of HBV DNA after 7-13 months of being treated, all were started on entecavir within 8-35 days and HBV DNA was cleared within 4 weeks, 2 subjects having mild, transient ALT elevations).
- Jianguo L, Zhixuan Z, Rong L, Xiaodong S. Ruxolitinib in alleviating the cytokine storm of hemophagocytic lymphohistiocytosis. Pediatrics. 2020;146:e20191301. [PubMed: 32680878](6 year old boy with idiopathic hemophagocytic lymphohistiocytic and chronic hepatitis B was treated with ruxolitinib and entecavir and had a sustained remission and improvement in serum HBV DNA and no worsening of ALT levels).
- Kiladjian JJ, Zachee P, Hino M, Pane F, Masszi T, Harrison CN, Mesa R, et al. Long-term efficacy and safety of ruxolitinib versus best available therapy in polycythaemia vera (RESPONSE): 5-year follow up of a phase 3 study. Lancet Haematol. 2020;7(3):e226–e237. [PMC free article: PMC8938906] [PubMed: 31982039](Among 222 patients with polycythemia vera treated with ruxolitinib or best available therapy for at least 80 weeks with cross over to ruxolitinib and continuation for 5 years in 65% of patients, durable response rates were seen only with ruxolitinib therapy and side effects were common but there were no treatment- or liver related deaths and no mention of ALT elevations or hepatotoxicity).
- Al-Ali HK, Griesshammer M, Foltz L, Palumbo GA, Martino B, Palandri F, Liberati AM, et al. Primary analysis of JUMP, a phase 3b, expanded-access study evaluating the safety and efficacy of ruxolitinib in patients with myelofibrosis, including those with low platelet counts. Br J Haematol. 2020;189:888–903. [PubMed: 32017044](Among 2233 patients with myelofibrosis treated in an expanded access study of ruxolitinib with a median duration of exposure of 12.4 months, ALT elevations were reported in 6% of patients and were above 5 times the ULN in 1.1%).
- Jagasia M, Perales MA, Schroeder MA, Ali H, Shah NN, Chen YB, Fazal S, et al. Ruxolitinib for the treatment of steroid-refractory acute GVHD (REACH1): a multicenter, open-label phase 2 trial. Blood. 2020;135:1739–49. [PMC free article: PMC7229262] [PubMed: 32160294](Among 71 patients with corticosteroid-resistant GvHD treated with ruxolitinib, the overall response rate by day 28 was 55% and ultimately in 73% while adverse events were common [97%] including anemia, thrombocytopenia and neutropenia, often leading to drug discontinuation [32%], while ALT elevations arose in 18 [25%] and were above 5 times ULN in 4 subjects [6%]).
- Zeiser R, von Bubnoff N, Butler J, Mohty M, Niederwieser D, Or R, Szer J, et al. REACH2 Trial Group. Ruxolitinib for glucocorticoid-refractory acute graft-versus-host disease. N Engl J Med. 2020;382:1800–10. [PubMed: 32320566](Among 309 patients with acute steroid-resistant GvHD treated with ruxolitinib or placebo for an average of 63 days, overall response rates were higher with ruxolitinib while adverse event rates were similar including any ALT elevation [7% vs 7%] and elevations above 5 times ULN [4% vs 3%] and there were no instances of clinically apparent liver injury).
- Zhao Y, Wu H, Shi J, Luo Y, Li X, Lan J, Ni W, et al. Ruxolitinib combined with etanercept induce a rapid response to corticosteroid-refractory severe acute graft vs host disease after allogeneic stem cell transplantation: Results of a multi-center prospective study. Am J Hematol. 2020;95:1075–84. [PubMed: 32510625](Among 64 patients with acute, corticosteroid-resistant GvHD after HCT who were treated with the combination of etanercept and ruxolitinib, the response rate was 88% and while infectious adverse events were common, there was no mention of ALT elevations or hepatotoxicity).
- Barraco F, Greil R, Herbrecht R, Schmidt B, Reiter A, Willenbacher W, Raymakers R, et al. Real-world non-interventional long-term post-authorisation safety study of ruxolitinib in myelofibrosis. Br J Haematol. 2020;191(5):764–74. [PubMed: 32583458](Among 426 patients with myelofibrosis with an average follow up of 26 months, those treated with ruxolitinib [n=259] compared to non-exposed patients [n=167] were more likely to have serious adverse events [65% to 80% vs 43%] including severe infections [49-68% vs 27.5%] and bleeding [31-41% vs 22%] and malignancies [14-27% vs 7%), but ALT and hepatotoxicity were not mentioned).
- Hou C, Dou L, Jia M, Li F, Wang S, Gao X, Wang L, Jin X, Wang L, Gao C, Liu D. Ruxolitinib combined with corticosteroids as first-line therapy for acute graft-versus-host disease in haploidentical peripheral blood stem cell transplantation recipients. Transplant Cell Ther. 2021;27(1):75.e1–75.e10. [PubMed: 32961370](Among 32 patients with acute GvHD after HCT treated with methylprednisolone and ruxolitinib, response rate at 6 months was 97% and “no hepatotoxicity was observed”).
- Cao Y, Wei J, Zou L, Jiang T, Wang G, Chen L, Huang L, et al. Ruxolitinib in treatment of severe coronavirus disease 2019 (COVID-19): A multicenter, single-blind, randomized controlled trial. J Allergy Clin Immunol. 2020;146:137–146.e3. [PMC free article: PMC7250105] [PubMed: 32470486](Among 41 adults with severe COVID-19 pneumonia treated with ruxolitinib [5 mg twice daily] or placebo, time to recovery [12 vs 15 days] and mortality [0% vs 14.5%] were lower numerically but not significantly with ruxolitinib and serum ALT elevations arose in 35% vs 9.5%, although all elevations were less than 5 times ULN and no patient had clinically apparent liver injury attributable to treatment).
- Giudice V, Pagliano P, Vatrella A, Masullo A, Poto S, Polverino BM, Gammaldi R, et al. Combination of ruxolitinib and eculizumab for treatment of severe SARS-CoV-2-related acute respiratory distress syndrome: a controlled study. Front Pharmacol. 2020;11:857. [PMC free article: PMC7291857] [PubMed: 32581810](Among 17 adults with moderate-to-severe COVID-19 pneumonia, 7 who were treated with ruxolitinib and eculizumab were compared to 10 with standard care, demonstrating more rapid recovery of oxygenation levels in the treatment group, but similar rates of death [14% vs 10%] and ALT elevations [57% vs 40%]).
- La Rosée F, Bremer HC, Gehrke I, Kehr A, Hochhaus A, Birndt S, Fellhauer M, et al. The Janus kinase 1/2 inhibitor ruxolitinib in COVID-19 with severe systemic hyperinflammation. Leukemia. 2020;34:1805–15. [PMC free article: PMC7282206] [PubMed: 32518419](Among 14 patients with severe COVID-19 and evidence of hyperinflammation who were treated with ruxolitinib for up to 14 days, 10 had rapid improvement and recovery and one died; mean ALT levels increased on therapy [from 50 to 109 U/L] rising above 5 times ULN in one subject).
- Neubauer A, Wiesmann T, Vogelmeier CF, Mack E, Skevaki C, Gaik C, Keller C, et al. Ruxolitinib for the treatment of SARS-CoV-2 induced acute respiratory distress syndrome (ARDS). Leukemia. 2020;34:2276–8. [PMC free article: PMC7298698] [PubMed: 32555296](Letter reporting case of a 65 year old Asian woman with severe COVID-19 pneumonia requiring mechanical ventilation who was treated with ruxolitinib and had rapid decrease in inflammatory markers in serum and subsequent clinical improvement).
- Saraceni F, Scortechini I, Mancini G, Mariani M, Federici I, Gaetani M, Barbatelli P, et al. Severe COVID-19 in a patient with chronic graft-versus-host disease after hematopoietic stem cell transplant successfully treated with ruxolitinib. Transpl Infect Dis. 2021;23:e13401. [PMC free article: PMC7361240] [PubMed: 32629531](59 year old man with myelofibrosis and hematopoietic cell transplant on ruxolitinib developed COVID-19 and respiratory failure with temporary discontinuation of ruxolitinib, but marked improvement when it was restarted with “no significant alteration of other laboratory tests” suggesting that it is not only safe but may be beneficial for SARS-CoV-2 infection).
- Innes AJ, Cook LB, Marks S, Bataillard E, Crossette-Thambiah C, Sivasubramaniam G, Apperley J, et al. Ruxolitinib for tocilizumab-refractory severe COVID-19 infection. Br J Haematol. 2020;190:e198–e200. [PMC free article: PMC7361819] [PubMed: 32593183](53 year old man with hematopoietic cell transplant on immunosuppressive agents developed COVID-19 pneumonia with a progressive downhill course that reversed soon after ruxolitinib [10 mg twice daily] was started] and “liver function” remained stable).
- Capochiani E, Frediani B, Iervasi G, Paolicchi A, Sani S, Roncucci P, Cuccaro A, et al. Ruxolitinib rapidly reduces acute respiratory distress syndrome in COVID-19 disease. analysis of data collection from RESPIRE Protocol. Front Med (Lausanne). 2020;7:466. [PMC free article: PMC7417512] [PubMed: 32850921](Among 18 patients with severe and progressive COVID-19 pneumonia treated with ruxolitinib [20 mg twice daily initially] there was rapid improvement in 16 patients; no mention of hepatic adverse events).
- Vannucchi AM, Sordi B, Morettini A, Nozzoli C, Poggesi L, Pieralli F, Bartoloni A, et al. RUXO-COVID Study Group. Compassionate use of JAK1/2 inhibitor ruxolitinib for severe COVID-19: a prospective observational study. Leukemia. 2021;35(4):1121–33. [PMC free article: PMC7437386] [PubMed: 32814839](Among 34 patients with severe COVID-19 pneumonia treated with ruxolitinib [5-10 mg bid] for an average of 13 days, 84% had clinical improvement by day 28, 3 had prolonged illness, and 2 died; ALT elevations were present in 29% at baseline and arose de novo in 15%, but none were above 5 times ULN).
- Gozzetti A, Capochiani E, Bocchia M. The Janus kinase 1/2 inhibitor ruxolitinib in COVID-19. Leukemia. 2020;34:2815–6. [PMC free article: PMC7467142] [PubMed: 32879427](Letter in response to mentioning their study [Capochiani] in which a higher dose of ruxolitinib was used [20 mg bid deescalating to 5 mg bid for a total of 14 days]).
- Sammartano V, Santoni A, Frediani B, Sicuranza A, Emanuele C, Franchi F, Capochiani E, et al. Efficacy and safety of ruxolitinib for Covid-19 related acute respiratory distress syndrome in a patient with blastic plasmacytoid dendritic cell neoplasm (leukemic variant). Leuk Lymphoma. 2020;61:3523–5. [PubMed: 32902339](Case of 59 year old man with blastic plasmacytoid dendritic cell neoplasm on chemotherapy developed COVID-19 related respiratory failure and failed to respond to standard care, corticosteroids and tocilizumab, demonstrated clinical improvement within days of starting ruxolitinib [20 mg twice daily]; no mention of hepatic adverse events).
- Betelli M, De Stefano F, Tedeschi A. Late worsening of COVID-19 pneumonia: successful treatment with ruxolitinib and steroid. Eur J Case Rep Intern Med. 2020;7:001938. [PMC free article: PMC7655002] [PubMed: 33194871](Case report of 67 year old man with COVID-19 pneumonia who had a recurrence of symptoms and signs a week after recovery but without detectable SARS-CoV-2 positivity responding to antibiotics, dexamethasone and ruxolitinib; no mention of liver test abnormalities).
- Caradec E, Mouren D, Zrounba M, Azoulay LD, Blandin C, Ivanoff S, Levy V, et al. COVID-19 in a patient with idiopathic pulmonary fibrosis successfully treated with ruxolitinib. Respir Med Res. 2021;79:100799. [PMC free article: PMC7647390] [PubMed: 33242734](69 year old man with idiopathic pulmonary fibrosis and COVID-19 pneumonia with progressive pulmonary dysfunction was treated with ruxolitinib [10 mg twice daily] and had rapid improvement in lung function and was discharged without supplement oxygen 2 weeks later).
- Peterson D, Damsky W, King B. The use of Janus kinase inhibitors in the time of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). J Am Acad Dermatol. 2020;82:e223–e226. [PMC free article: PMC7144601] [PubMed: 32278797](Letter expressing caution about use of Janus kinase inhibitors during COVID-19 infection based upon their mechanism of action in blocking intracellular signaling pathways mediated by Janus kinases, but also mentioning 3 patients with alopecia areata who developed COVID-19 infection while on an inhibitor and had a relative mild, normal course of infection).
- Satarker S, Tom AA, Shaji RA, Alosious A, Luvis M, Nampoothiri M. JAK-STAT pathway inhibition and their implications in COVID-19 therapy. Postgrad Med. 2021;133(5):489–507. [PMC free article: PMC7784782] [PubMed: 33245005](Review of the mechanism of action and pleomorphic activities of Janus kinase inhibitors and their possible role in treating severe COVID-19 infection which is often accompanied by high levels of proinflammatory cytokines [cytokine storm], with listing of ongoing trials including several of ruxolitinib).
- Wong HS, Guo CL, Lin GH, Lee KY, Okada Y, Chang WC. Transcriptome network analyses in human coronavirus infections suggest a rational use of immunomodulatory drugs for COVID-19 therapy. Genomics. 2021;113:564–75. [PMC free article: PMC7817445] [PubMed: 33482326](Analysis of the temporal pattern of gene expression in cells infected with SARS-CoV-2 suggests that medications most likely to affect these changes include among others dexamethasone, baricitinib, tofacitinib, sarilumab, ritonavir, naproxen, avelumab, durvalumab and atezolizumab).
- Banerjee A, Goswami RP, Chatterjee M. Network theoretic analysis of JAK/STAT pathway and extrapolation to drugs and viruses including COVID-19. Sci Rep. 2021;11:2512. [PMC free article: PMC7844052] [PubMed: 33510353](A theoretic analysis of the pathways affected by various rheumatologic medications and pathways affected by viral infections suggests that baricitinib would have the highest likelihood of efficacy in SARS-CoV-2 infection with lower efficacy of the other Janus kinase inhibitors, tofacitinib and ruxolitinib).
- D'Alessio A, Del Poggio P, Bracchi F, Cesana G, Sertori N, Di Mauro D, Fargnoli A, et al. Low-dose ruxolitinib plus steroid in severe SARS-CoV-2 pneumonia. Leukemia. 2021;35:635–8. [PMC free article: PMC7654848] [PubMed: 33173161](Among 32 patients with severe COVID-19 pneumonia treated with ruxolitinib [5 mg twice daily for 7 and once daily for 3 days], recovery without ICU admission was higher than in an untreated control group [75% vs 63%] and mortality was less [9% vs 30%), and they “did not observe any major adverse events”).
- Rizk JG, Forthal DN, Kalantar-Zadeh K, Mehra MR, Lavie CJ, Rizk Y, Pfeiffer JP, et al. Expanded Access Programs, compassionate drug use, and Emergency Use Authorizations during the COVID-19 pandemic. Drug Discov Today. 2021;26:593–603. [PMC free article: PMC7694556] [PubMed: 33253920](Review of expanded access programs [EAP] and emergency use authorization [EUA] for COVID-19 interventions by the FDA during 2020 mentions that both baricitinib and ruxolitinib were allowed EAPs, but only baricitinib was granted an EUA).
- Mortara A, Mazzetti S, Margonato D, Delfino P, Bersano C, Catagnano F, Lauriola M, et al. Compassionate use of ruxolitinib in patients with SARS-Cov-2 infection not on mechanical ventilation: Short-term effects on inflammation and ventilation. Clin Transl Sci. 2021;14(3):1062–1068. [PMC free article: PMC8212747] [PubMed: 33403775](Among 31 patients hospitalized with severe COVID-19 pneumonia and hypoxemia treated with ruxolitinib [5 mg twice daily for up to 15 days], symptomatic improvement occurred by 7 days in 81%, “no adverse events were recorded” and there were no significant changes in laboratory test results).
- Raghuvanshi R, Bharate SB. Recent developments in the use of kinase inhibitors for management of viral infections. J Med Chem. 2022;65:893–921. [PubMed: 33539089](Review of the kinase inhibitors approved for use in the US, their mechanisms of action and possible role in inhibiting viral replication).
- Iastrebner M, Castro J, García Espina E, Lettieri C, Payaslian S, Cuesta MC, Gutiérrez Fernández P, et al. Ruxolitinib in severe COVID-19: results of a multicenter, prospective, single arm, open-label clinical study to investigate the efficacy and safety of ruxolitinib in patients with COVID-19 and severe acute respiratory syndrome. Rev Fac Cien Med Univ Nac Cordoba. 2021;78:294–302. [PMC free article: PMC8760921] [PubMed: 34617700](Among 51 hospitalized adults with COVID-19 treated with ruxolitinib or placebo added to standard of care, the mortality rate was 0% but rates of ICU admission, mechanical ventilation and duration of hospitalization were similar to those in historical controls, while ALT or AST elevations occurred in 58% on ruxolitinib vs 48% in controls).
- Neubauer A, Johow J, Mack E, Burchert A, Meyn D, Kadlubiec A, Torje I, Wulf H, et al. The janus-kinase inhibitor ruxolitinib in SARS-CoV-2 induced acute respiratory distress syndrome (ARDS). Leukemia. 2021;35:2917–2923. [PMC free article: PMC8358255] [PubMed: 34385593](Among 16 adults with COVID-19 pneumonitis on mechanical ventilation treated with ruxolitinib [10 mg twice daily], the 29 day mortality was 19% and adverse events included one patient with ALT elevations).
- Gatti M, Turrini E, Raschi E, Sestili P, Fimognari C. Janus kinase inhibitors and coronavirus disease (COVID)-19: rationale, clinical evidence and safety issues. Pharmaceuticals (Basel). 2021;14:738. [PMC free article: PMC8401109] [PubMed: 34451835](Review of the theoretic basis for use of JAK inhibitors in COVID-19 disease, clinical efficacy and safety of baricitinib and ruxolitinib mentions rare instances of ALT elevations and one case of drug induced liver injury).
- Garcia-Horton A, Smith E, Maze D, McNamara C, Sibai H, Gupta V. Risk of hepatitis B virus reactivation in HBsAg-negative, anti-HBc-positive patients with myeloproliferative neoplasms treated with ruxolitinib. Leuk Lymphoma. 2021;62:495–497. [PubMed: 33459565](Among 58 patients with myeloproliferative neoplasms who had anti-HBc without HBsAg, only one of 20 treated with ruxolitinib developed reactivation of hepatitis B which was mild and transient [peak HBV DNA 530 IU/mL, normal ALT and bilirubin], while none of 38 anti-HBc positive patients receiving other antineoplastic therapies developed reactivation).
- Duan MH, Cao XX, Chang L, Zhou DB. Risk of hepatitis B virus reactivation following ruxolitinib treatment in patients with myeloproliferative neoplasms. Hematology. 2021;26:460–464. [PubMed: 34184610](Among 224 patients with myeloproliferative neoplasms treated with ruxolitinib between 2013 and 2020, 2 of 6 HBsAg-positive patients developed reactivation of hepatitis B [both did not receive prophylaxis while the other 4 did], but none of 56 with anti-HBc without HBsAg developed reactivation despite not receiving antiviral prophylaxis).
- Sjoblom M, Chtioui H, Fraga M, Stalder G, Grandoni F, Blum S. Hepatitis B reactivation during ruxolitinib treatment. Ann Hematol. 2022;101:2081–2086. [PubMed: 35488090](79 year old man with polycythemia vera and secondary myelofibrosis who was HBsAg negative but anti-HBc positive developed reactivation of hepatitis B with HBV DNA [19 million IU/mL], HBsAg and ALT elevations [385 U/L] but without symptoms or jaundice after 4 years of successful ruxolitinib therapy, responding to stopping chemotherapy and starting tenofovir and later able to restart ruxolitinib).
- Hoisnard L, Lebrun-Vignes B, Maury S, Mahevas M, El Karoui K, Roy L, Zarour A, et al. Adverse events associated with JAK inhibitors in 126,815 reports from the WHO pharmacovigilance database. Sci Rep. 2022;12:7140. [PMC free article: PMC9065106] [PubMed: 35504889](Among 126,815 individual case safety reports on ruxolitinib, tofacitinib and baricitinib made to the WHO pharmacovigilance registry, infections were most frequent including viral, fungal, bacterial and mycobacterial complications, while there was no increase in hepatobiliary reports).
- Levy G, Guglielmelli P, Langmuir P, Constantinescu S. JAK inhibitors and COVID-19. J Immunother Cancer. 2022;10:e002838. [PMC free article: PMC9035837] [PubMed: 35459733](Review of the mechanism of action of JAK inhibitors and results of their use in severe COVID-19 infection focusing upon baricitinib; ruxolitinib has not been shown to ameliorate the course of COVID-19 in hospitalized patients whereas baricitinib has, the reasons for the difference being unclear as they both have activity against JAK1 and JAK2).
- Raghuvanshi R, Bharate SB. Recent developments in the use of kinase inhibitors for management of viral infections. J Med Chem. 2022;65:893–921. [PubMed: 33539089](Review of the kinase inhibitors approved for use in the US, their mechanisms of action and possible role in inhibiting viral replication).
- Han MK, Antila M, Ficker JH, Gordeev I, Guerreros A, Bernus AL, Roquilly A, et al. Ruxolitinib in addition to standard of care for the treatment of patients admitted to hospital with COVID-19 (RUXCOVID): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Rheumatol. 2022;4:e351–e361. [PMC free article: PMC8963773] [PubMed: 35368384](Among 432 hospitalized patients with COVID-19 not on mechanical ventilation or in the ICU treated with ruxolitinib [5 mg twice daily] or placebo for 14 days, there were no differences in mortality rates with [3% vs 2%] or rates of ICU admission or mechanical ventilation in the two groups and adverse event rates were similar [65% vs 62%], as were serious adverse events [11% vs 10.5%] and ALT elevations [6% vs 4%]).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Momelotinib.[LiverTox: Clinical and Researc...]Review Momelotinib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Elevation of the Hepatitis B Virus DNA during the Treatment of Polycythemia Vera with the JAK Kinase Inhibitor Ruxolitinib.[Intern Med. 2016]Elevation of the Hepatitis B Virus DNA during the Treatment of Polycythemia Vera with the JAK Kinase Inhibitor Ruxolitinib.Kirito K, Sakamoto M, Enomoto N. Intern Med. 2016; 55(10):1341-4. Epub 2016 May 15.
- Review Recent progress of JAK inhibitors for hematological disorders.[Immunol Med. 2023]Review Recent progress of JAK inhibitors for hematological disorders.Kirito K. Immunol Med. 2023 Sep; 46(3):131-142. Epub 2022 Oct 28.
- JAK inhibition with ruxolitinib versus best available therapy for myelofibrosis.[N Engl J Med. 2012]JAK inhibition with ruxolitinib versus best available therapy for myelofibrosis.Harrison C, Kiladjian JJ, Al-Ali HK, Gisslinger H, Waltzman R, Stalbovskaya V, McQuitty M, Hunter DS, Levy R, Knoops L, et al. N Engl J Med. 2012 Mar 1; 366(9):787-98.
- Review Janus kinase inhibitors: jackpot or potluck?[Oncol Rev. 2012]Review Janus kinase inhibitors: jackpot or potluck?Pavithran K, Pande SB. Oncol Rev. 2012 Mar 5; 6(1):e13. Epub 2012 Jun 20.
- Ruxolitinib - LiverToxRuxolitinib - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...