NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Niraparib is a small molecule inhibitor of poly ADP-ribose polymerase that is used in the therapy of selected patients with refractory and advanced ovarian carcinoma. Niraparib therapy is associated with a low rate of transient elevations in serum aminotransferase during therapy, but has not been linked to instances of clinically apparent liver injury.
Background
Niraparib (nye rap' a rib) is an orally available, small molecule inhibitor of poly adenine diphosphate (ADP)-ribose polymerase (PARP), an enzyme involved in DNA transcription and repair. Patients with mutations of the BRCA 1 and 2 genes are at increased risk for cancer, particularly ovarian and breast cancer in women. The BRCA gene encodes DNA repair enzymes, and tumor cells with BRCA mutations have an increased dependence on PARP and increased sensitivity to its inhibition. Clinical trials of niraparib in women with advanced, refractory ovarian, fallopian tube or primary peritoneal carcinoma have shown response rates of 30% to 40% and prolongation of progression-free survival. Niraparib is also under evaluation as therapy for advanced breast cancer and other malignant diseases associated mutations in BRCA or other DNA repair enzymes. Niraparib received approval for use in the United States in 2017 for therapy of advanced and refractory advanced, refractory ovarian, fallopian tube or primary peritoneal carcinoma. Niraparib is available in 100 mg capsules under the brand name Zejula. The recommended dose is 300 mg by mouth once daily continued until disease progression or unacceptable toxicity occurs. Common side effects include anemia, fatigue, nausea, diarrhea, constipation, dyspepsia, abdominal pain, anorexia, shortness of breath and thrombocytopenia. Uncommon, but potentially severe side effects include myelodysplastic syndrome, marked bone marrow suppression, cardiovascular events and embryo-fetal toxicity.
Hepatotoxicity
In preregistration, randomized controlled clinical trials of niraparib, abnormalities in routine liver tests were common, but were mostly mild and self-limited in course. Serum ALT elevations occurred in 28% of patients (vs 15% of controls), but values were above 5 times the upper limit of normal (ULN) in only 1% (vs 2% of controls). Despite the frequency of serum enzyme elevations during therapy in clinical trials, there were no reports of hepatitis with jaundice or liver failure. Subsequent to its approval and more wide scale use, there have been no published reports of clinically apparent liver injury attributed to niraparib, but the extent and duration of its use have been limited. Thus, niraparib is a known cause of mild serum enzyme elevations but has not been linked to significant hepatotoxicity.
Likelihood score: E* (unproven but suspected cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism of injury accounting for the serum enzyme elevations during niraparib therapy is not known. Niraparib is metabolized by carboxylesterases to an inactive product. It not metabolized to an appreciable extent by the cytochrome P450 system and has minimal drug-drug interactions.
Outcome and Management
Serum aminotransferase elevations above 5 times the upper limit of normal (if confirmed) during therapy with niraparib should lead to dose reduction or temporary cessation. There does not appear to be cross reactivity in risk for hepatic injury between niraparib and other PARP inhibitors such as olaparib or rucaparib.
Drug Class: Antineoplastic Agents, Protein Kinase Inhibitors
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Niraparib – Zejula®
DRUG CLASS
Antineoplastic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Niraparib | 1038915-60-4 | C19-H20-N4-O |
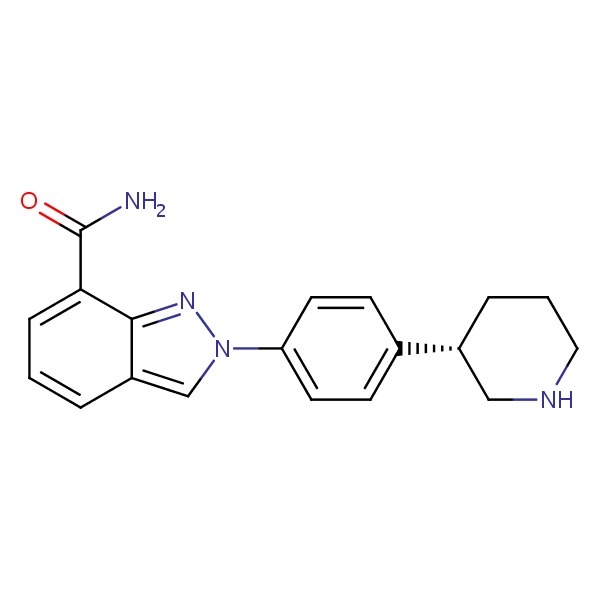 |
ANNOTATED BIBLIOGRAPHY
References updated: 20 July 2017
- Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999.(Review of hepatotoxicity published in 1999 before the availability of protein kinase or PARP inhibitors such as niraparib, olaparib and rucaparib).
- DeLeve LD. Erlotinib. Cancer chemotherapy. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 556.(Review of hepatotoxicity of cancer chemotherapeutic agents discusses several tyrosine kinase inhibitors including imatinib, gefitinib, erlotinib and crizotinib, but not olaparib or rucaparib).
- Chabner BA, Barnes J, Neal J, Olson E, Mujagic H, Sequist L, Wilson W, et al. Targeted therapies: tyrosine kinase inhibitors, monoclonal antibodies, and cytokines. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1731-54.(Textbook of pharmacology and therapeutics).
- Garnett MJ, Edelman EJ, Heidorn SJ, Greenman CD, Dastur A, Lau KW, Greninger P, et al. Systematic identification of genomic markers of drug sensitivity in cancer cells. Nature 2012; 483 (7391): 570-5. [PMC free article: PMC3349233] [PubMed: 22460902](Correlation of mutated cancer genes identified in cancer cell lines with their sensitivity to growth inhibition by antineoplastic agents revealed the possible role of PARP inhibition in several tumors including Ewing sarcoma).
- Plummer R, Lorigan P, Steven N, Scott L, Middleton MR, Wilson RH, Mulligan E, et al. A phase II study of the potent PARP inhibitor, Rucaparib (PF-01367338, AG014699), with temozolomide in patients with metastatic melanoma demonstrating evidence of chemopotentiation. Cancer Chemother Pharmacol 2013; 71: 1191-9. [PubMed: 23423489](Among 46 patients with metastatic melanoma treated with the combination of temozolomide and rucaparib [12 mg/m2 intravenously for 5 days of 28-day cycles], found objective response rates of 17%, side effects including myelosuppression were common and one patient died of “hepatorenal failure”).
- Shah RR, Morganroth J, Shah DR. Hepatotoxicity of tyrosine kinase inhibitors: clinical and regulatory perspectives. Drug Saf 2013; 36: 491-503. [PubMed: 23620168](Review of the hepatotoxicity of 18 tyrosine kinase inhibitors approved for use in cancer in the US as of 2013, discusses imatinib and sunitinib, but not olaparib or rucaparib).
- Bao Z, Cao C, Geng X, Tian B, Wu Y, Zhang C, Chen Z, Li W, et al. Effectiveness and safety of poly (ADP-ribose) polymerase inhibitors in cancer therapy: A systematic review and meta-analysis. Oncotarget 2016; 7: 7629-39 . [PMC free article: PMC4884943] [PubMed: 26399274](Systematic review of the efficacy and safety of PARP inhibitors in cancer chemotherapy mentioned that in 5 placebo controlled trials, ALT elevations were no more frequent with the PARP inhibitors than in “controls”, but neither were there any other adverse events).
- Konecny GE, Kristeleit RS. PARP inhibitors for BRCA1/2-mutated and sporadic ovarian cancer: current practice and future directions. Br J Cancer 2016; 115: 1157-73. [PMC free article: PMC5104889] [PubMed: 27736844](Review of role of BRCA 1 and 2 mutations in tumorigenesis and the mechanism of action of PARP inhibitors).
- Ledermann JA. PARP inhibitors in ovarian cancer. Ann Oncol 2016; 27 Suppl 1: i40-4. [PubMed: 27141070](Review of possible role of PARP inhibitors in ovarian cancer mentions that cells with defective BRCA proteins are deficient in repair of double-stranded breaks in DNA by homologous recombination and rely on other pathways, notably PARP that detects single DNA strand breaks and activates effector proteins to initiate repair).
- Sandhu SK, Schelman WR, Wilding G, Moreno V, Baird RD, Miranda S, Hylands L, et al. The poly (ADP-ribose) polymerase inhibitor niraparib (MK4827) in BRCA mutation carriers and patients with sporadic cancer: a phase 1 dose-escalation trial. Lancet Oncol 2013; 14: 882-92. [PubMed: 23810788](Among 100 patients with advanced or metastatic cancers refractory to chemotherapy who received escalating doses of niraparib, common side effects were anemia [48%], nausea [42%], fatigue [42%], thrombocytopenia [35%], anorexia [26%], neutropenia [24%], and constipation [23%]; severe side effects included neutropenia, prolongation of the QTc interval and severe fatigue; no mention of ALT elevations or hepatotoxicity).
- Infante JR, Burris HA 3rd. PARP inhibitors: pitfalls and promises. Lancet Oncol 2013; 14: 798-9. [PubMed: 23810789](Commentary in response to Sandhu [2013]).
- Mirza MR, Monk BJ, Herrstedt J, Oza AM, Mahner S, Redondo A, Fabbro M, et al.; ENGOT-OV16/NOVA Investigators. Niraparib maintenance therapy in platinum-sensitive, recurrent ovarian cancer. N Engl J Med 2016; 375: 2154-64. [PubMed: 27717299](Among 553 patients with recurrent ovarian cancer after platinum-based chemotherapy treated with niraparib or placebo, progression-free survival was improved by niraparib, particularly in patients with germline BRCA mutations while adverse events were mostly hematologic and manageable; no mention of ALT elevations or hepatotoxicity).
- Scott LJ. Niraparib: First Global Approval. Drugs 2017; 77: 1029-34. [PubMed: 28474297](Review of the mechanism of action, pharmacology, clinical efficacy and safety of niraparib shortly after its initial approval in the US; no mention of ALT elevations or hepatotoxicity).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Rucaparib.[LiverTox: Clinical and Researc...]Review Rucaparib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Olaparib.[LiverTox: Clinical and Researc...]Review Olaparib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Human mass balance study and metabolite profiling of (14)C-niraparib, a novel poly(ADP-Ribose) polymerase (PARP)-1 and PARP-2 inhibitor, in patients with advanced cancer.[Invest New Drugs. 2017]Human mass balance study and metabolite profiling of (14)C-niraparib, a novel poly(ADP-Ribose) polymerase (PARP)-1 and PARP-2 inhibitor, in patients with advanced cancer.van Andel L, Zhang Z, Lu S, Kansra V, Agarwal S, Hughes L, Tibben MM, Gebretensae A, Lucas L, Hillebrand MJX, et al. Invest New Drugs. 2017 Dec; 35(6):751-765. Epub 2017 Mar 16.
- Avatrombopag Optimizes Response to Niraparib by Managing Thrombocytopenia Associated with Poly-ADP Ribose Polymerase (PARP) Inhibition in Ovarian Cancer and Breast Cancer: A Case Series.[Am J Case Rep. 2020]Avatrombopag Optimizes Response to Niraparib by Managing Thrombocytopenia Associated with Poly-ADP Ribose Polymerase (PARP) Inhibition in Ovarian Cancer and Breast Cancer: A Case Series.Gabrail N, Smith C. Am J Case Rep. 2020 Nov 16; 21:e927008. Epub 2020 Nov 16.
- Review The poly (ADP ribose) polymerase inhibitor niraparib: Management of toxicities.[Gynecol Oncol. 2018]Review The poly (ADP ribose) polymerase inhibitor niraparib: Management of toxicities.Moore KN, Mirza MR, Matulonis UA. Gynecol Oncol. 2018 Apr; 149(1):214-220. Epub 2018 Feb 4.
- Niraparib - LiverToxNiraparib - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...