NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Metoclopramide is an oral prokinetic and antiemetic agent used in the therapy of gastroesophageal reflux disease, gastroparesis and severe or chemotherapy induced nausea. Metoclopramide has been linked to rare instances of clinically apparent liver injury that are typically cholestatic and can be associated with bile duct loss.
Background
Metoclopramide is a benzamide (a para-aminobenzoic acid derivative) which acts as a prokinetic agent on the gastrointestinal tract and an antiemetic, particularly in persons with gastrointestinal dysmotility. Its mechanism of action is uncertain; it is a serotonin type 4 (5-HT4) receptor agonist, but also has antagonist activity against vagal and central 5HT3 receptors and dopamine type 2 (D2) receptors. It increases the tone and amplitude of gastric contractions, relaxes the pyloric sphincter and increases peristalsis in the duodenum and jejunum, resulting in improved gastrointestinal motility and accelerated gastric emptying. Metoclopramide was approved for use in the United States in 2005 and is widely used in therapy of nausea, vomiting and gastrointestinal motility disorders including gastroparesis, with more than 6 million prescriptions being filled yearly. Metoclopramide is available as 5 and 10 mg tablets in generic forms and under the brand name Reglan. It is also available as a liquid solution for oral use and in injectable forms. The typical oral dose for gastroesophageal reflux and gastroparesis in adults is 10 to 15 mg taken 30 minutes before meals. Intravenous and intramuscular formulations are used for therapy of postoperative or chemotherapy induced nausea and vomiting. Therapy should not exceed 12 weeks in duration. Common side effects include restlessness, drowsiness, dizziness, headache, fatigue, diarrhea and polyuria. Chronic therapy has been associated with episodes of dystonia, oculogyric crises and extrapyramidal syndromes including tardive dyskinesia and Parkinson like symptoms for which it has a “black box” warning.
Hepatotoxicity
Serum aminotransferase elevations during metoclopramide therapy are uncommon and rates of such elevations were not reported in the large clinical trials demonstrating its efficacy in motility disorders. Metoclopramide has been listed as a cause of clinically apparent liver injury in several large series of drug induced liver disease, but without documentation of the nature of the injury or degree of causality assessment. Clinical descriptions of liver injury attributable to metoclopramide are few, but the latency to onset of liver injury is usually less than 30 days and the pattern of liver enzyme elevations cholestatic. Immunoallergic features are not prominent. Prolonged jaundice and persistent pruritus suggestive of bile duct loss and vanishing bile duct syndrome has been described. Metoclopramide has not been listed as a cause of acute liver failure in large clinical series.
Likelihood score: C (probable cause of clinically apparent liver injury).
Mechanism of Injury
Metoclopramide has little active hepatic metabolism and is excreted largely unchanged in the urine. The clinically apparent liver disease attributed to metoclopramide is probably immune mediated.
Outcome and Management
Most instances of liver injury due to metoclopramide have been self-limiting and resolve upon withdrawal of the agent. A single instance of vanishing bile duct syndrome has been described. Little is known about cross sensitivity with other prokinetic medications.
Drug Class: Gastrointestinal Agents, Antiemetics
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Metoclopramide – Generic, Reglan®
DRUG CLASS
Gastrointestinal Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Metoclopramide | 364-62-5 | C14-H22-Cl-N3-O2 |
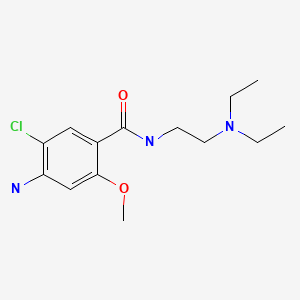
|
ANNOTATED BIBLIOGRAPHY
References updated: 03 February 2020
- Zimmerman HJ. Antiemetic and prokinetic compounds. Miscellaneous drugs and diagnostic chemicals. In, Zimmerman, HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999: pp. 721.(Expert review of hepatotoxicity published in 1999 mentions that metoclopramide by itself has not been incriminated in any cases of hepatitis).
- Sharkey KA, MacNaughton WK. Gastrointestinal motility and water flux, emesis and biliary and pancreatic disease. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 921-44.(Textbook of pharmacology and therapeutics; metoclopramide is a prokinetic agent which improves gastric emptying and the symptoms of nausea and vomiting caused by gastrointestinal dysmotility syndromes).
- Feurle GE. Arteriovenous shunting and cholestasis in hepatic hemangiomatosis associated with metoclopramide. Gastroenterology 1990; 99: 258-62. 2344931. [PubMed: 2344931](22 year old woman developed abdominal pain 4 months after starting metoclopramide and oral contraceptives, and was found to have multiple hepatic hemangiomatosis which worsened during therapy [bilirubin rising to 2.6 mg/dL, AST 26 U/L, Alk P 325 rising to 1700 U/L] and appeared to improve after metoclopramide was stopped, but patient still had marked Alk P elevations 2 years later).
- Hainsworth J, Harvey W, Pendergrass K, Kasimis B, Oblon D, Monaghan G, Gandara D, et al. A single-blind comparison of intravenous ondansetron, a selective serotonin antagonist, with intravenous metoclopramide in the prevention of nausea and vomiting associated with high-dose cisplatin chemotherapy. J Clin Oncol 1991; 9: 721-8. 1826739. [PubMed: 1826739](Among 307 patients receiving cisplatin chemotherapy, ALT elevations above twice ULN occurred in 6% of those receiving ondansetron vs 0% on metoclopramide for prevention of nausea and vomiting, but all abnormalities were asymptomatic and resolved within 2 weeks).
- Desta Z, Wu GM, Morocho AM, Flockhart DA. The gastroprokinetic and antiemetic drug metoclopramide is a substrate and inhibitor of cytochrome P450 2D6. Drug Metab Dispos 2002; 30: 336-43. 11854155. [PubMed: 11854155](Metoclopramide is metabolized by CYP 2D6 and may affect the clearance of drugs that are cleared by this isoenzyme).
- Lata PF, Pigarelli DL. Chronic metoclopramide therapy for diabetic gastroparesis. Ann Pharmacother 2003; 37: 122-6. 12503946. [PubMed: 12503946](Review of efficacy and safety of metoclopramide in gastroparesis mentions that it has adverse effects in up to 20% of patients, mostly drowsiness and lethargy, but that tardive dyskinesia can occur with long term use; no mention of ALT abnormalities or hepatotoxicity).
- Henzi I, Walder B, Tramèr MR. Metoclopramide in the prevention of postoperative nausea and vomiting: a quantitative systematic review of randomized, placebo-controlled studies. Br J Anaesth 1999; 83: 761-71. 10690140. [PubMed: 10690140](Systematic review of 66 studies, including 3260 patients receiving metoclopramide for postoperative nausea and vomiting and 3006 controls, reported no differences in rates of adverse events, but ALT elevations and hepatotoxicity were not mentioned).
- Chevallier B, Cappelaere P, Splinter T, Fabbro M, Wendling JL, Cals L, Catimel G, et al. A double-blind, multicentre comparison of intravenous dolasetron mesilate and metoclopramide in the prevention of nausea and vomiting in cancer patients receiving high-dose cisplatin chemotherapy. Support Care Cancer 1997; 5: 22-30. 9010986. [PubMed: 9010986](Among 226 patients with cancer receiving cisplatin, 4% of 157 receiving dolasetron vs 1% receiving metoclopramide developed liver test abnormalities).
- Bruera ED, MacEachern TJ, Spachynski KA, LeGatt DF, MacDonald RN, Babul N, Harsanyi Z, et al. Comparison of the efficacy, safety, and pharmacokinetics of controlled release and immediate release metoclopramide for the management of chronic nausea in patients with advanced cancer. Cancer 1994; 74: 3204-11. 7982184. [PubMed: 7982184](Among 34 patients with cancer treated with controlled or immediate release metoclopramide to prevent nausea and vomiting from chemotherapy, side effects were similar with the two formulations; no mention made of ALT elevations or hepatotoxicity).
- Sledge GW Jr, Einhorn L, Nagy C, House K. Phase III double-blind comparison of intravenous ondansetron and metoclopramide as antiemetic therapy for patients receiving multiple-day cisplatin-based chemotherapy. Cancer 1992; 70: 2524-8. 1423181. [PubMed: 1423181](Among 45 patients with cancer receiving cisplatin based chemotherapy, 1 of 22 patients who were treated with metoclopramide versus 3 of 23 on ondansetron developed serum ALT elevations, but none developed signs of symptoms of liver injury).
- de Abajo FJ, Montero D, Madurga M, García Rodríguez LA. Acute and clinically relevant drug-induced liver injury: a population based case-control study. Br J Clin Pharmacol 2004; 58: 71-80. 15206996. [PMC free article: PMC1884531] [PubMed: 15206996](Analysis of General Practice Research Database from UK on 1.6 million persons from 1994-2000 found 128 cases of drug induced liver injury; 5 cases were due to metoclopramide including 2 hepatocellular and 3 cholestatic, 4 with jaundice and 4 with latency of <30 days; odds ratio compared to population was 6.2; incidence of 12 per 100,000 users).
- Sabaté M, Ibáñez L, Pérez E, Vidal X, Buti M, Xiol X, Mas A, et al. Risk of acute liver injury associated with the use of drugs: a multicentre population survey. Aliment Pharmacol Ther 2007; 25: 1401-9. 17539979. [PubMed: 17539979](Population based survey of 126 cases of acute liver injury [24 with acute liver failure] due to drugs between 1993-1999 in Spain calculated relative risk of injury compared to the general population: 7 cases were attributed to metoclopramide, giving a relative risk 4.1 and incidence 1.7 per 100,000 person years of exposure).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J; Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008; 135: 1924-34. 18955056. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, no cases were attributed to an antiemetic or metoclopramide).
- Reuben A, Koch DG, Lee WM; Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology 2010; 52: 2065-76. 20949552. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, but none were attributed to antiemetic agents or metoclopramide).
- Ferrajolo C, Capuano A, Verhamme KM, Schuemie M, Rossi F, Stricker BH, Sturkenboom MC. Drug-induced hepatic injury in children: a case/non-case study of suspected adverse drug reactions in VigiBase. Br J Clin Pharmacol 2010; 70: 721-8. 21039766. [PMC free article: PMC2997312] [PubMed: 21039766](Among 624,673 adverse event reports in children between 2000 and 2006 in the WHO VigiBase, 1% were hepatic, but neither metoclopramide or any antiemetic was listed among the 41 most commonly implicated agents).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 2013; 144: 1419-25. 23419359. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, but none were attributed to antiemetics or metoclopramide).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol 2014; 13: 231-9. 24552865. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, the most common implicated agents being nimesulide [n=53: 30%], cyproterone [n=18], nitrofurantoin [n=17], antituberculosis drugs [n=13] and flutamide [n=12: 7%]; antiemetics and metoclopramide were not listed).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52. e7. 25754159. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, one case was attributed to metoclopramide: a 51 year old man developed jaundice one month after starting metoclopramide for gastroparesis [bilirubin 6.9 mg/dL, ALT 779 U/L, Alk P 859], with jaundice lasting 5 months followed by intermittent but persistent pruritus and Alk P elevations suggestive of bile duct paucity).
- Bonkovsky HL, Kleiner DE, Gu J, Odin JA, Russo MW, Navarro VM, Fontana RJ, et al.; U.S. Drug Induced Liver Injury Network Investigators. Clinical presentations and outcomes of bile duct loss caused by drugs and herbal and dietary supplements. Hepatology 2017; 65: 1267-77. 27981596. [PMC free article: PMC5360519] [PubMed: 27981596](Among 26 patients with drug induced liver injury and liver biopsy findings of bile duct loss, one was attributed to metoclopramide: Chalasani [2015]).
- Meegada S, Heda RP, Satapathy S, Verma R. Metoclopramide-induced serotonin syndrome. Cureus 2019; 11: e6359. 31938643. [PMC free article: PMC6957036] [PubMed: 31938643](28 year old woman with suicidal acetaminophen overdose [initial bilirubin 3.4, ALT 7982 U/L, Alk P 142 U/L, INR 5.3] and was recovering rapidly and being treated with intravenous metoclopramide when she developed tachycardia, hypertension, tremor, hyperreflexia and clonus suggestive of serotonin syndrome, which resolved within 36 hours of stopping metoclopramide and did not appear to worsen the liver injury).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Metoclopramide: a dopamine receptor antagonist.[Am Fam Physician. 1990]Review Metoclopramide: a dopamine receptor antagonist.DiPalma JR. Am Fam Physician. 1990 Mar; 41(3):919-24.
- Gastric electrical stimulation: an evidence-based analysis.[Ont Health Technol Assess Ser....]Gastric electrical stimulation: an evidence-based analysis.Medical Advisory Secretariat. Ont Health Technol Assess Ser. 2006; 6(16):1-79. Epub 2006 Aug 1.
- Review Prokinetic therapy for gastroesophageal reflux disease.[Am Fam Physician. 1995]Review Prokinetic therapy for gastroesophageal reflux disease.Robinson M. Am Fam Physician. 1995 Sep 1; 52(3):957-62, 965-6.
- Metoclopramide nasal spray is effective in symptoms of gastroparesis in diabetics compared to conventional oral tablet.[Neurogastroenterol Motil. 2014]Metoclopramide nasal spray is effective in symptoms of gastroparesis in diabetics compared to conventional oral tablet.Parkman HP, Carlson MR, Gonyer D. Neurogastroenterol Motil. 2014 Apr; 26(4):521-8. Epub 2013 Dec 25.
- Metoclopramide suppositories in the treatment of diabetic gastroparesis.[Arch Intern Med. 1986]Metoclopramide suppositories in the treatment of diabetic gastroparesis.Trapnell BC, Mavko LE, Birskovich LM, Falko JM. Arch Intern Med. 1986 Nov; 146(11):2278-9.
- Metoclopramide - LiverToxMetoclopramide - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...