NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Maraviroc is a chemokine co-receptor 5 (CCR5) antagonist, the first of a new class of agents active against the human immunodeficiency virus (HIV) and the acquired immunodeficiency syndrome (AIDS). Maraviroc was approved for use in the United States in 2007 but has had limited use. Maraviroc has been associated with elevations in serum aminotransferase levels and to several cases of acute, clinically apparent liver injury.
Background
Maraviroc (mar" a vir' ok) is relatively new antiretroviral drug that targets one of the receptors for HIV that is present on the surface of lymphocytes. Maraviroc interrupts the binding of HIV to target cells by blocking the chemokine coreceptor 5 (CCR5), a necessary receptor in the uptake of HIV into cells. Maraviroc has both in vitro and in vivo activity against HIV and several randomized controlled trials have shown that it leads to significant decline in HIV RNA levels and rises in peripheral CD4 T cell counts. Maraviroc was given accelerated approval for use in HIV infection in the United States in 2007 and is currently used in a relatively small proportion of antiretroviral regimens, being recommended largely for HIV-treatment experienced adult patients with CCR5-tropic strains of HIV. Maraviroc is available as 150 and 300 mg tablets generically and under the brand name Selzentry. The recommended dose is 150 to 600 mg twice daily in combination with other classes of antiretroviral agents. Common side effects include cough, fever, rash and dizziness. Rare but potentially severe adverse events include myocardial ischemia or infarction, hypotension, hepatotoxicity and severe hypersensitivity reactions including Stevens Johnson syndrome and toxic epidermal necrolysis.
Hepatotoxicity
Therapy with maraviroc was associated with alanine aminotransferase (ALT) elevations in up to 10% of patients, but elevations above 5 times normal are less common. Furthermore, rates of ALT elevations with maraviroc were similar to rates in comparator groups receiving similar background optimized antiretroviral therapy [2.6% vs 3.4% above 5 times ULN in one study and 3.9% vs 4.0% in a second]. These elevations have not been associated with clinical symptoms and generally did not require dose modification. Nevertheless, two cases of acute hepatocellular injury arose in patients receiving maraviroc in prelicensure clinical trials. Both were women, ages 24 and 27, who developed fever, fatigue and rash followed by liver tests abnormalities within 1 to 3 weeks of starting maraviroc. One patient remained anicteric (peak bilirubin 1.5 mg/dL) while the other developed marked jaundice (peak bilirubin 31 mg/dL) and underwent emergency liver transplantation 16 days after onset. In both instances, other potential causes were present but no other diagnosis was confirmed. For these reasons, hepatitis and hepatic failure are listed as adverse events in the product label which includes a boxed warning about hepatotoxicity. Aplaviroc, the initial CCR5 antagonist developed, was abandoned during preclinical testing because of concerns about hepatotoxicity. The clinical features of hepatotoxicity related to maraviroc have not been described in detail and the drug has had limited use. There have been no further reports of liver failure attributed to maraviroc therapy.
Likelihood score: D (possible rare cause of clinically apparent liver injury).
Mechanism of Injury
Maraviroc is extensively metabolized in the liver via the CYP 450 system and is a substrate for P-glycoprotein, making it susceptible to multiple drug-drug interactions. Thus, liver injury from maraviroc may be due to its hepatic conversion to a toxic or immunogenic intermediate. The reported cases have had features suggestive of a hypersensitivity reaction.
Outcome and Management
The serum aminotransferase abnormalities that occur during maraviroc therapy are usually mild and self-limited, not requiring dose modification or discontinuation. The course and outcome of more clinically apparent hepatotoxicity has not been characterized. There is unlikely to be any cross sensivity to hepatic injury between maraviroc and other antiretroviral agents.
Drug Class: Antiviral Agents
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Maraviroc – Selzentry®
DRUG CLASS
Antiviral Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Maraviroc | 376348-65-1 | C29-H41-F2-N5-O |
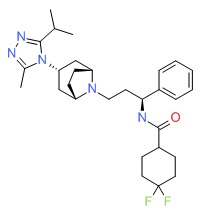 |
ANNOTATED BIBLIOGRAPHY
References updated: 06 June 2019
- Núñez M. Hepatic toxicity of antiviral agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 505-18.(Review of hepatotoxicity of antiviral agents including maraviroc).
- Flexner C. Antiretroviral agents and treatment of HIV infection. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1137-57.(Textbook of pharmacology and therapeutics).
- https://www
.accessdata .fda.gov/drugsatfda_docs /nda/2007/022128_selzentry_toc.cfm. (FDA website with the formal review of the safety and efficacy of maraviroc with descriptions of the two patients who developed clinically apparent liver injury during the prelicensure clinical trials). - http://aidsinfo
.nih.gov/guidelines. (Clinical guidelines on the use of antiretroviral agents in HIV-1 infected adults, adolescents and children). - Horster S, Goebel FD. Serious doubts on safety and efficacy of CCR5 antagonists: CCR5 antagonists teeter on a knife-edge. Infection 2006; 34; 110-3. [PubMed: 16703305](Review of safety of CCR5 antagonists: aplaviroc, maraviroc and vicriviroc; among 336 patients enrolled in two studies of aplaviroc, 12 developed hepatotoxicity arising after an average of 13 weeks [1 coinfected with HBV and 1 with HCV] with jaundice in 4; a single case of acute liver failure arose after 4 doses of maraviroc in a patient on isoniazid and trimethoprim-sulfamethoxazole, but little evidence for a class effect in causing hepatotoxicity).
- Crabb C. GlaxoSmithKline ends aplaviroc trials. AIDS 2006; 20: 641. [PubMed: 16514292](News article that Glaxo stopped trial of aplaviroc, a CCR5 inhibitor for HIV infection, after 3 patients given drug for 4 weeks developed ALT elevations; none had jaundice or developed liver failure).
- Telenti A, Egger M. Identifying safety concerns from genetic data: lessons from the development of CCR5 inhibitors. Antivir Ther 2007; 12: 147-8. [PubMed: 17503656](Editorial discussing the safety of inhibition of CCR5; CCR5 plays an important role in host immune defenses and its inhibition may have adverse effects on susceptibility to other infections, although this has yet to be shown).
- Hammer SM, Eron JJ Jr, Reiss P, Schooley RT, Thompson MA, Walmsley S, Cahn P, et al.; International AIDS Society-USA. Antiretroviral treatment of adult HIV infection: 2008 recommendations of the International AIDS Society-USA panel. JAMA 2008; 300: 555-70. [PubMed: 18677028](Recommendations on use of antiviral therapy in adults with HIV infection including maraviroc).
- Two new drugs for HIV infection. Med Lett Drugs Ther 2008; 50: 2-4. [PubMed: 18197163](Concise summary on the safety and efficacy of ralegravir and maraviroc in treatment-refractory or treatment-experienced patients with HIV infection; hepatotoxicity reported with maraviroc [with rash and eosinophilia], but not with raltegravir).
- Gulick RM, Lalezari J, Goodrich J, Clumeck N, DeJesus E, Horban A, Nadler J, et al.; MOTIVATE Study Teams. Maraviroc for previously treated patients with R5 HIV-1 infection. N Engl J Med. 2008; 359: 1429-41. [PMC free article: PMC3078519] [PubMed: 18832244](Two controlled trials of maraviroc versus placebo combined with optimized antiretroviral therapy in 1049 patients treated for 48 weeks; there were "no significant differences in the rates of treatment-related adverse events"; ALT elevations >5 times ULN occurred in 3.5% on maraviroc vs 3.3% on placebo; no mention of clinically apparent hepatotoxicity).
- Emmelkamp JM, Rockstroh JK. Maraviroc, risks and benefits: a review of the clinical literature. Expert Opin Drug Saf 2008; 7: 559-69. [PubMed: 18759708](Review of structure, mode of action, clinical efficacy and safety of maraviroc, the first CCR5 coreceptor antagonist approved for HIV infection; elevations in serum ALT levels occurred as frequently in control as in maraviroc-treated patients; discuss a case of acute liver failure occurring in a patient receiving maraviroc in registration trial who was also on isoniazid and trimethoprim-sulfamethoxazole).
- Abel S, van der Ryst E, Rosario MC, Ridgway CE, Medhurst CG, Taylor-Worth RJ, Muirhead GJ. Assessment of the pharmacokinetics, safety and tolerability of maraviroc, a novel CCR5 antagonist, in healthy volunteers. Br J Clin Pharmacol 2008; 65 Suppl 1: 5-18. [PMC free article: PMC2311414] [PubMed: 18333861](Results of single and multiple dose pharmacokinetic studies of maraviroc in normal controls; no serious adverse events but ALT elevations occurred in 11% and levels were >3 times ULN in one; high dose arm was discontinued because of postural hypotension).
- Hughes CA, Robinson L, Tseng A, MacArthur RD. New antiretroviral drugs: a review of the efficacy, safety, pharmacokinetics, and resistance profile of tipranavir, darunavir, etravirine, rilpivirine, maraviroc, and raltegravir. Expert Opin Pharmacother 2009; 10: 2445-66. [PubMed: 19678794](Review of tipranavir, darunavir, etravirine, rilpivirine, maraviroc and raltegravir; hepatotoxicity seen with aplaviroc does not appear to be a class effect and only one case of severe hepatotoxicity reported in registration trials of maraviroc; no differences in side effects in cohorts with HCV or HBV coinfection, but maraviroc was approved with a "black box" warning about hepatotoxicity).
- Saag M, Goodrich J, Fäenheuer G, Clotet B, Clumeck N, Sullivan J, Westby M, et al.; A4001029 Study Group. A double-blind, placebo-controlled trial of maraviroc in treatment-experienced patients infected with non-R5 HIV-1. J Infect Dis 2009; 199: 1638-47. [PubMed: 19432546](Placebo controlled trial of maraviroc [in two doses] in 167 treatment-experienced patients with non-R5 strains of HIV [strains not requiring CCR5 for cell entry] for 24 weeks found no difference in HIV RNA suppression; ALT elevations >5 times ULN in 1% on maraviroc vs 5% on placebo and no clinically apparent liver injury or liver related deaths).
- Ayoub A, Alston S, Goodrich J, Heera J, Hoepelman AI, Lalezari J, Mchale M, et al. Hepatic safety and tolerability in the maraviroc clinical development program. AIDS 2010; 24: 2743-50. [PubMed: 20935557](Summary of the hepatic safety of maraviroc from prelicensure controlled trials found no difference in rates of liver enzyme elevations between maraviroc and control treated arms; however, two participants had severe hepatotoxicity that was possibly related to maraviroc, but other potential causes of liver injury were present).
- Sierra-Madero J, Di Perri G, Wood R, Saag M, Frank I, Craig C, Burnside R, et al. Efficacy and safety of maraviroc versus efavirenz, both with zidovudine/lamivudine: 96-week results from the MERIT study. HIV Clin Trials 2010; 11: 125-32. [PubMed: 20736149](In a controlled trial of maraviroc vs efavirenz combined with optimized background therapy continued to 96 weeks, ALT elevations >5 times ULN occurred in 4% of both groups, most elevations occurring during the first 48 weeks).
- Hardy WD, Gulick RM, Mayer H, Fätkenheuer G, Nelson M, Heera J, Rajicic N, Goodrich J. Two-year safety and virologic efficacy of maraviroc in treatment-experienced patients with CCR5-tropic HIV-1 infection: 96-week combined analysis of MOTIVATE 1 and 2. J Acquir Immune Defic Syndr 2010; 55: 558-64. [PMC free article: PMC3321258] [PubMed: 20703158](In an extended treatment of patients in two controlled trials of maraviroc to 96 weeks, the rate of ALT elevations >3 times ULN per 100 patients years was 7.8 for maraviroc vs 10.0 for placebo combined with optimized background therapy).
- Ortu F, Weimer LE, Floridia M, Manconi PE. Raltegravir, tenofovir, and emtricitabine in an HIV-infected patient with HCV chronic hepatitis, NNRTI intolerance and protease inhibitors-induced severe liver toxicity. Eur J Med Res 2010; 15: 81-3. [PMC free article: PMC3352050] [PubMed: 20452889](43 year old woman with HIV/HCV coinfection who developed symptomatic elevations of serum enzymes on saquinavir, fosamprenavir and again on darunavir, was adequately maintained on tenofovir/emtricitabine and raltegravir).
- Wasmuth JC, Rockstroh JK, Hardy WD. Drug safety evaluation of maraviroc for the treatment of HIV infection. Expert Opin Drug Saf 2012; 11: 161-74. [PubMed: 22118500](Systematic review of the safety of maraviroc from randomized controlled trials in the published literature and from presentations at meetings concluded that “no relevant toxicities or co-morbidities such as ... hepatotoxicty have been described”).
- Lazzarin A, Than S, Valluri SR, Heera J, Mukwaya G. Safety profile of maraviroc in patients coinfected with HIV-1 and hepatitis B or C included in the maraviroc expanded access program. HIV Clin Trials 2012; 13: 83-9. [PubMed: 22510355](Analysis of maraviroc expanded access program of 1032 patients found hepatobiliary events more common in HIV-infected patients with HCV coinfection [10 vs 3.1 per 100 patient years]; rates of ALT elevations >5 times ULN were similar in patients receiving expanded access maraviroc vs placebo recipients in the Motivate trial [Hardy 2010] including those with HIV monoinfection [1.5% vs 3.1%], HIV/HBV coinfection [5.9% vs 8.3%] and HIV/HCV coinfection [8.7% vs 3.3%]).
- Mangiafico L, Perja M, Fusco F, Riva S, Mago D, Gringeri A. Safety and effectiveness of raltegravir in patients with haemophilia and anti-HIV multidrug resistance. Haemophilia 2012; 18: 108-11. [PubMed: 21762404](Among 7 patients with hemophilia and HIV-HCV coinfection on antiretroviral regimens including raltegravir, only 1 had an increase in liver enzyme levels and “cholestasis”, which resolved promptly when maraviroc was discontinued while raltegravir was continued).
- Surgers L, Lacombe K. Hepatoxicity of new antiretrovirals: a systematic review. Clin Res Hepatol Gastroenterol 2013; 37: 126-33. [PubMed: 23522569](Review of the rates of liver test abnormalities in large clinical trials of new antiretroviral agents [etravirine, rilpivirine, maraviroc, raltegravir, elvitegravir, dolutegravir and darunavir] concludes that "the overall hepatic tolerance is far bettter with the novel drugs in this review than with former ARV regimens"; only darunavir and maraviroc had warnings about liver injury when they were released).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 12 [1.3%] cases were attributed to antiretroviral agents, but none to the maraviroc or other CCR5 coreceptor antagonists).
- Neukam K, Mira JA, Collado A, Rivero-Juárez A, Monje-Agudo P, Ruiz-Morales J, Ríos MJ, et al; HEPAVIR SEG-HEP-2007 Study Group of the Sociedad Andaluza de Enfermedades Infecciosas (SAEI). Liver toxicity of current antiretroviral regimens in HIV-infected patients with chronic viral hepatitis in a real-life setting: The HEPAVIR SEG-HEP Cohort. PLoS One 2016; 11: e0148104. [PMC free article: PMC4743911] [PubMed: 26848975](Among 192 "real-life" patients with HIV who were coinfected with HBV or HCV and were started on a new antiretroviral regimen, 10 [5%] developed ALT or AST elevations above 5 times ULN, including 1 of 9 started on maraviroc, but none required drug discontinuation because of the elevations or developed clinically apparent liver injury).
- Rockstroh JK, Plonski F, Bansal M, Fätkenheuer G, Small CB, Asmuth DM, Pialoux G, et al. Hepatic safety of maraviroc in patients with HIV-1 and hepatitis C and/or B virus: 144-week results from a randomized, placebo-controlled trial. Antivir Ther 2017; 22: 263-9. [PubMed: 27924779](Among 137 patients with HIV and HBV or HCV coinfection who were treated with maraviroc or placebo in addition to their standard antiretroviral regimen for 144 weeks, rates of ALT or AST elevations and hepatobiliary adverse events were similar in the two groups).
- Bunchorntavakul C, Reddy KR. Drug Hepatotoxicity: Newer Agents. Clin Liver Dis 2017; 21: 115-34. [PubMed: 27842767](Review of the hepatotoxicity of selected newly approved medications including maraviroc which was implicated in a few cases of hepatotoxicity including acute liver failure in prelicensure clinical trials).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Maraviroc (UK-427,857), a potent, orally bioavailable, and selective small-molecule inhibitor of chemokine receptor CCR5 with broad-spectrum anti-human immunodeficiency virus type 1 activity.[Antimicrob Agents Chemother. 2...]Maraviroc (UK-427,857), a potent, orally bioavailable, and selective small-molecule inhibitor of chemokine receptor CCR5 with broad-spectrum anti-human immunodeficiency virus type 1 activity.Dorr P, Westby M, Dobbs S, Griffin P, Irvine B, Macartney M, Mori J, Rickett G, Smith-Burchnell C, Napier C, et al. Antimicrob Agents Chemother. 2005 Nov; 49(11):4721-32.
- Review Chemokine receptor CCR5 antagonist maraviroc: medicinal chemistry and clinical applications.[Curr Top Med Chem. 2014]Review Chemokine receptor CCR5 antagonist maraviroc: medicinal chemistry and clinical applications.Xu GG, Guo J, Wu Y. Curr Top Med Chem. 2014; 14(13):1504-14.
- Marginal Effects of Systemic CCR5 Blockade with Maraviroc on Oral Simian Immunodeficiency Virus Transmission to Infant Macaques.[J Virol. 2018]Marginal Effects of Systemic CCR5 Blockade with Maraviroc on Oral Simian Immunodeficiency Virus Transmission to Infant Macaques.Brocca-Cofano E, Xu C, Wetzel KS, Cottrell ML, Policicchio BB, Raehtz KD, Ma D, Dunsmore T, Haret-Richter GS, Musaitif K, et al. J Virol. 2018 Sep 1; 92(17). Epub 2018 Aug 16.
- Review Maraviroc: a CCR5-receptor antagonist for the treatment of HIV-1 infection.[Clin Ther. 2008]Review Maraviroc: a CCR5-receptor antagonist for the treatment of HIV-1 infection.Lieberman-Blum SS, Fung HB, Bandres JC. Clin Ther. 2008 Jul; 30(7):1228-50.
- Reduced maximal inhibition in phenotypic susceptibility assays indicates that viral strains resistant to the CCR5 antagonist maraviroc utilize inhibitor-bound receptor for entry.[J Virol. 2007]Reduced maximal inhibition in phenotypic susceptibility assays indicates that viral strains resistant to the CCR5 antagonist maraviroc utilize inhibitor-bound receptor for entry.Westby M, Smith-Burchnell C, Mori J, Lewis M, Mosley M, Stockdale M, Dorr P, Ciaramella G, Perros M. J Virol. 2007 Mar; 81(5):2359-71. Epub 2006 Dec 20.
- Maraviroc - LiverToxMaraviroc - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...