NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Macitentan is an endothelin receptor antagonist that is used in the therapy of pulmonary arterial hypertension (PAH). Macitentan has been associated with a low rate of serum enzyme elevations during therapy, but has yet to be implicated in cases of clinically apparent acute liver injury.
Background
Macitentan (ma" si ten' tan) is a nonselective inhibitor of the endothelin-1 receptors, both type A and B. Inhibition of endothelin receptors disrupts the intracellular pathways that lead to vasoconstriction, thus causing vasodilation. Because macitentan has high affinity for pulmonary endothelin receptors, it preferentially causes vasodilation in the pulmonary vasculature, thereby decreasing pulmonary vascular pressure. In prospective, randomized controlled trials, macitentan was effective in alleviating symptoms, improving exercise capacity and prolonging the time to clinical worsening in patients with idiopathic PAH. Macitentan was the third endothelin receptor antagonist to be approved in the United States (2013). The current indications are for symptomatic pulmonary arterial hypertension, classified as WHO group 1 (idiopathic). Use of macitentan in forms of PAH due to heart failure, thromboembolic disease or connective tissue disease should be considered experimental as its efficacy in these forms of PAH has not been adequately shown. Macitentan is available in tablets of 10 mg under the brand name Opsumit and the recommended dose is 10 mg once daily. Because of the potential for teratogenicity, macitentan is available for treating women only as a part of a risk evaluation and mitigation strategy (REMS) program in which documentation of adequate methods for birth control are required. Common side effects include headaches, dizziness, anemia, edema, flushing, rhinitis and dyspepsia that are frequent with most vasodilator therapies. Uncommon, but potentially severe adverse reactions include embryo-fetal toxicity, decrease in sperm counts, anemia and hypersensitivity reactions.
Hepatotoxicity
Macitentan is associated with a low rate of serum aminotransferase elevations (0% to 4%) that, in clinical trials, was similar to the rate among placebo recipients. These elevations were usually mild, transient and not associated with symptoms, but were above 8 times the ULN in 2% of subjects (vs 0.4% of controls) in at least one long term study. For these reasons, the product label recommends that patients have serum enzymes tested before starting therapy and be alerted to the possibility and symptoms of liver injury during therapy. While there have been no published reports of clinically apparent liver injury with jaundice associated with macitentan, it has had limited general use. Other endothelin receptor antagonists (bosentan, sitaxentan) have been linked to several instances of acute liver injury, some of which have been severe. The onset of illness was usually within 1 to 6 months of starting bosentan and the enzyme pattern was typically hepatocellular or mixed. Immunoallergic features were not present and autoantibodies absent or present in low titer. Macitentan and ambrisentan have not been linked to similar cases.
Likelihood score: E* (unlikely but suspected cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism by which macitentan might cause liver injury is not known. Macitentan is metabolized by the cytochrome P450 system (CYP 2C9 and 3A4), which may lead to production of a toxic intermediate and can also cause drug-drug interactions, particularly with strong inducers or inhibitors of CYP 3A4. One possible reason for why macitentan is associated with a relatively low rate of ALT elevations and hepatotoxicity is its higher potency and lower daily dose (10 mg) in comparison to bosentan (125 to 250 mg).
Outcome and Management
The serum enzyme elevations associated with macitentan use have been mild-to-moderate and self-limited in course, often resolving despite drug continuation. There is no information on cross sensitivity to hepatic injury among the various endothelin receptor antagonists.
Drug Class: Pulmonary Arterial Hypertension Agents
Other Drugs in the Class: Endothelin Receptor Antagonists: Ambrisentan, Bosentan
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Macitentan – Opsumit®
DRUG CLASS
Pulmonary Arterial Hypertension Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Macitentan | 441798-33-0 | C19-H20-Br2-N6-O4-S |
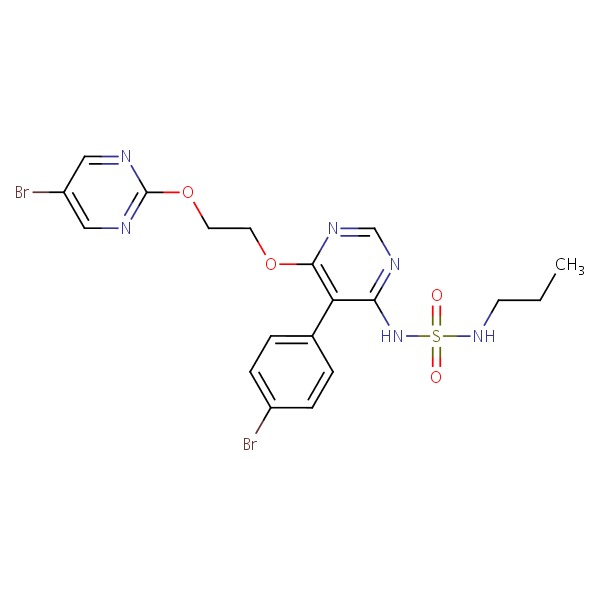 |
ANNOTATED BIBLIOGRAPHY
References updated: 30 September 2017
Abbreviations used: PAH, pulmonary arterial hypertension
- Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999.(Textbook of hepatotoxicity published in 1999, before the availability of endothelin receptor antagonists).
- Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013.(Textbook on drug induced liver injury; clinical features of liver injury due to the endothelin receptor antagonists are not specifically discussed).
- Barnes PJ. Pharmacotherapy of pulmonary arterial hypertension. Pulmonary Pharmacology. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1059-61.(Textbook of pharmacology and therapeutics).
- Channick RN, Simonneau G, Sitbon O, Robbins IM, Frost A, Tapson VF, Badesch DB, et al. Effects of the dual endothelin-receptor antagonist bosentan in patients with pulmonary hypertension: a randomised placebo-controlled study. Lancet 2001; 358: 1119-23. [PubMed: 11597664](Controlled trial of bosentan [250 mg daily] vs placebo for at least 12 weeks in 32 patients with pulmonary arterial hypertension [PAH]; 2 of 21 patients receiving bosentan developed ALT elevations which resolved without need for discontinuation).
- Galié N, Badesch D, Oudiz R, Simonneau G, McGoon MD, Keogh AM, Frost AE, et al. Ambrisentan therapy for pulmonary arterial hypertension. J Am Coll Cardiol 2005; 46: 529-35. [PubMed: 16053970](Among 64 patients with PAH treated with 1 of 4 doses of ambrisentan for 12 weeks, 3.1% developed ALT elevations above 3 times ULN and 2 patients discontinued therapy because of ALT values, but none had symptoms or jaundice).
- Nagai Y, Okada E, Mihara S, Sato K, Ohi S, Ishikawa O. Severe liver dysfunction due to bosentan in a patient with mixed connective tissue disease. Eur J Dermatol 2008; 18: 190-1. [PubMed: 18424383](A 70 year old woman with connective tissue disease and digital ulcers developed ALT elevations [77 U/L] 2 months after starting bosentan, which rapidly worsened [ALT 3597 U/L, bilirubin and Alk P not given] despite stopping bosentan, and progressed to multiorgan failure and death within 2 weeks).
- Galié N, Rubin Lj, Hoeper M, Jansa P, Al-Hiti H, Meyer G, Chiossi E, et al. Treatment of patients with mildly symptomatic pulmonary arterial hypertension with bosentan (EARLY study): a double-blind, randomised controlled trial. Lancet 2008; 371: 2093-100. [PubMed: 18572079](Controlled trial of bosentan [n=93] vs placebo [n=92] for 6 months in patients with PAH; serum ALT levels above 3 times ULN arose in 13% of bosentan- vs 2% of placebo-treated patients, mostly in first 20 weeks and resolving spontaneously in many without dose adjustment and without clinically apparent liver injury).
- Galié N, Olschewski H, Oudiz RJ, Torres F, Frost A, Ghofrani HA, Badesch DB, et al.; Ambrisentan in Pulmonary Arterial Hypertension, Randomized, Double-Blind, Placebo-Controlled, Multicenter, Efficacy Studies (ARIES) Group. Ambrisentan for the treatment of pulmonary arterial hypertension: results of the ambrisentan in pulmonary arterial hypertension, randomized, double-blind, placebo-controlled, multicenter, efficacy (ARIES) study 1 and 2. Circulation 2008; 117: 3010-9. [PubMed: 18506008](Combined analysis of two controlled trials of different doses of ambrisentan vs placebo for 12 weeks in a total of 261 patients with PAH found that no patient developed ALT elevation above 3 times ULN).
- Eriksson C, Gustavsson A, Kronvall T, Tysk C. Hepatotoxicity by bosentan in a patient with portopulmonary hypertension: a case-report and review of the literature. J Gastrointestin Liver Dis 2011; 20: 77-80. [PubMed: 21451802](A 29 year old woman developed jaundice 18 months after starting bosentan [bilirubin ~10 mg/dL, ALT 600 U/L, Alk P 480 U/L, INR 1.3], worsening for several weeks and then improving rapidly after starting prednisolone which ultimately could be withdrawn without relapse).
- Raghu G, Million-Rousseau R, Morganti A, Perchenet L, Behr J; MUSIC Study Group. Macitentan for the treatment of idiopathic pulmonary fibrosis: the randomised controlled MUSIC trial. Eur Respir J 2013; 42: 1622-32. [PubMed: 23682110](Among 178 patients with pulmonary fibrosis treated with macitentan or placebo for one year, there were no differences in changes in lung function or time to worsening or death between the two groups, and serum ALT elevations above 3 times ULN occurred in 3.4% on macitentan vs 5% on placebo).
- Pulido T, Adzerikho I, Channick RN, Delcroix M, Galiè N, Ghofrani HA, Jansa P, et al.; SERAPHIN Investigators. Macitentan and morbidity and mortality in pulmonary arterial hypertension. N Engl J Med 2013; 369: 809-18. [PubMed: 23984728](Among 742 patients with PAH treated with two doses of macitentan [3 or 10 mg daily] or placebo for one year, exercise tolerance was improved and time to clinical worsening delayed by macitentan, while side effects included headache, rhinitis and anemia; ALT elevations above 3 times ULN occurred in 3.4-3.6% of macitentan vs 4.5% of placebo recipients and were accompanied by bilirubin elevations in 1.7-2.1% vs 1.7%).
- Macitentan (Opsumit) for pulmonary arterial hypertension. Med Lett Drugs Ther 2014; 56 (1436): 15-6. [PubMed: 24663031](Concise review of the mechanism of action, clinical efficacy, safety and costs of macitentan shortly after its approval for use in the US; mentions that rates of ALT elevations during macitentan therapy are no higher than with placebo, but elevations above 8 times ULN occurred in 2.1% with macitentan vs 0.4% with placebo).
- Macías Saint-Gerons D, de la Fuente Honrubia C, Montero Corominas D, Catalá-López F. [Hepatotoxicity in patients treated with endothelin receptor antagonists: Systematic review and meta-analysis of randomized clinical trials.]. Med Clin (Barc) 2014; 142: 333-42. Spanish. [PubMed: 23540381](Systematic review of the literature, including 21 trials in 3644 patients, found relative risk of ALT or AST elevations above 3 times ULN to be 2.98 for endothelin receptor antagonists compared to placebo controls).
- Hill NS, Badesch D, Benza RL, D'Eletto TA, Farber HW, Gomberg-Maitland M, Hassoun PM, Preston I. Perspectives on oral pulmonary hypertension therapies recently approved by the U.S. Food and Drug Administration. Ann Am Thorac Soc 2015; 12: 269-73. [PubMed: 25590376](Review of recently approved drugs for PAH including macitentan, riociguat and oral treprostinil; mentions that macitentan was not associated with a higher rate of serum enzyme elevations in comparison to placebo therapy, but that testing of serum enzymes before treatment is recommended and intermittent monitoring is prudent).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, one was attributed to bosentan, but none to macitentan or other agents used primarily to treat pulmonary artery hypertension).
- Selej M, Romero AJ, Channick RN, Clozel M. Development of macitentan for the treatment of pulmonary arterial hypertension. Ann N Y Acad Sci 2015; 1358: 68-81. [PubMed: 26291180](Review of the clinical features, natural history, pathogenesis and therapy of PAH, and the development of macitentan, identified by modifying the molecular structure of bosentan and screening for high affinity for endothelin-1 receptor binding).
- Tahara N, Dobashi H, Fukuda K, Funauchi M, Hatano M, Ikeda S, Joho S, et al. Efficacy and Safety of a novel endothelin receptor antagonist, macitentan, in Japanese patients with pulmonary arterial hypertension. Circ J 2016; 80: 1478-83. [PubMed: 27180890](Among 30 Japanese patients with PAH treated with macitentan for at least 6 months, exercise tolerance and pulmonary function improved, and ALT elevations occurred in only one patient [3%] compared to 16% of bosentan treated subjects monitored in Japanese postmarketing studies).
- Wei A, Gu Z, Li J, Liu X, Wu X, Han Y, Pu J. Clinical adverse effects of endothelin receptor antagonists: insights from the meta-analysis of 4894 patients from 24 randomized double-blind placebo-controlled clinical trials. J Am Heart Assoc 2016; 5. pii: e003896. [PMC free article: PMC5210319] [PubMed: 27912207](Systematic review of 24 randomized trials of endothelin receptor antagonists indicated higher rates of "abnormal liver function" in patients receiving bosentan and macitentan, but not ambrisentan).
- Safdar Z, Thakur A, Frost A. Tolerability of switch to macitentan from bosentan in pulmonary arterial hypertension. South Med J 2017; 110: 223-228. [PubMed: 28257550](Among 24 patients with PAH switched from bosentan to macitentan for unstated reasons, mean serum ALT and AST did not change although one patient had to stop macitentan because of ALT elevations).
- Review Macitentan in the treatment of pulmonary arterial hypertension.[Future Cardiol. 2021]Review Macitentan in the treatment of pulmonary arterial hypertension.Zebadúa R, Hernández-Pérez AP, García A, Zayas N, Sandoval J, López J, Pulido T. Future Cardiol. 2021 Jan; 17(1):49-58. Epub 2020 Jul 17.
- Slow receptor dissociation kinetics differentiate macitentan from other endothelin receptor antagonists in pulmonary arterial smooth muscle cells.[PLoS One. 2012]Slow receptor dissociation kinetics differentiate macitentan from other endothelin receptor antagonists in pulmonary arterial smooth muscle cells.Gatfield J, Mueller Grandjean C, Sasse T, Clozel M, Nayler O. PLoS One. 2012; 7(10):e47662. Epub 2012 Oct 15.
- Long-term treatment of pulmonary arterial hypertension with macitentan in Japanese patients.[Curr Med Res Opin. 2020]Long-term treatment of pulmonary arterial hypertension with macitentan in Japanese patients.Tahara N, Dobashi H, Fukuda K, Funauchi M, Hatano M, Ikeda S, Joho S, Kihara Y, Kondo T, Matsushita M, et al. Curr Med Res Opin. 2020 Jun; 36(6):921-928. Epub 2020 May 12.
- Review Pharmacokinetic and pharmacodynamic evaluation of macitentan , a novel endothelin receptor antagonist for the treatment of pulmonary arterial hypertension.[Expert Opin Drug Metab Toxicol...]Review Pharmacokinetic and pharmacodynamic evaluation of macitentan , a novel endothelin receptor antagonist for the treatment of pulmonary arterial hypertension.Sidharta PN, Krähenbühl S, Dingemanse J. Expert Opin Drug Metab Toxicol. 2015 Mar; 11(3):437-49. Epub 2015 Jan 21.
- Macitentan: An important addition to the treatment of pulmonary arterial hypertension.[J Pharmacol Pharmacother. 2015]Macitentan: An important addition to the treatment of pulmonary arterial hypertension.Khadka A, Singh Brashier DB, Tejus A, Sharma AK. J Pharmacol Pharmacother. 2015 Jan-Mar; 6(1):53-7.
- Macitentan - LiverToxMacitentan - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...