NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Linezolid is an oxazolidinone class antibiotic that is used for serious or problematic infections caused by resistant enterococcal or staphylococcal organisms. Prolonged therapy with linezolid has been linked to rare instances of lactic acidosis and liver injury probably as a result of hepatic mitochondrial toxicity.
Background
Linezolid (lin ayz' oh lid) is a synthetic antibiotic that belongs to the oxazolidinone class. It has broad bacteriocidal activity against gram positive organisms such as enterococci and staphylococci and most streptococci. It also has moderate activity against Mycobacterium tuberculosis. Linezolid acts by blocking bacterial protein synthesis, probably as a result of blocking the formation of the functional ribosomal 70S subunit. Linezolid was approved for use in the United States in 2000 and is currently indicated for treatment of vancomycin-resistant enterococcal infections, for nosocomial pneumonia due to staphylococci (either methicillin-sensitive or -resistant) and skin and tissue infections caused by Staphylococcus aureus or pyogenes. Because of its activity against multidrug resistant enterococci and staphylococci, the use of linezolid is usually reserved for severe infections where methicillin or penicillin resistance is found. Linezolid is also used in some regimens for therapy of multidrug resistant tuberculosis. Linezolid is available in tablets of 400 and 600 mg generically and under the name Zyvox. It is also available as an oral suspension and a solution for intravenous administration. Linezolid is typically given as a 7 to 14 day course of 400 or 600 mg twice daily. Longer courses are sometimes used for persistent infections. Common minor side effects include nausea, diarrhea, abdominal upset, headache and skin rash. Rare, but severe side effects include serotonin syndrome, thrombocytopenia, optic and peripheral neuropathy, pancreatitis and lactic acidosis.
Hepatotoxicity
Therapy with linezolid has been associated with mild and transient elevations in serum aminotransferase and alkaline phosphatase levels in 1% to 10% of patients, although similar rates of elevations occur in patients with infections treated with comparable agents, and enzyme elevations were not found in normal volunteers given linezolid for short periods. On the other hand, ALT elevations during therapy have been higher with higher doses of linezolid, but in all instances the elevations occurred without symptoms and resolved with discontinuation of the drug.
Although the agent has been available for a limited time and its use has been restricted, several instances of clinically apparent liver disease with jaundice have been reported with linezolid therapy. A case of a hypersensitivity response with rash, eosinophilia and renal insufficiency (DRESS syndrome) with mild serum enzyme elevations has been reported. More frequently, linezolid has been linked to cases of lactic acidosis, generally arising after 1 to 8 weeks of therapy and sometimes associated with evidence of liver injury and jaundice. Lactic acidosis is usually due to injury and dysfunction of hepatic mitochondria, with resulting microvesicular steatosis and disturbed hepatic function (not necessarily accompanied by jaundice or even ALT or alkaline phosphatase elevations). Other serious side effects associated with mitochondrial damage due to linezolid therapy include peripheral and optic neuropathy, pancreatitis, serotonin syndrome and renal injury. Risk factors for developing lactic acidosis from linezolid include higher doses, longer courses of therapy and underlying chronic liver or renal disease. The mitochondrial injury is believed to be due to the inhibition of mitochondrial ribosomal function that matches the known effect of linezolid on bacterial ribosomal function. Lactic acidosis occurs after 1 to 8 weeks of treatment and can be severe, although it often resolves rapidly with discontinuation. In contrast, the optic and peripheral neuropathy due to linezolid resolves more slowly and can be permanent. Lactic acidosis can be fatal and hepatic dysfunction and jaundice have been mentioned in severe cases of lactic acidosis attributed to linezolid.
Likelihood score: A (well established cause of clinically apparent liver injury usually in association with lactic acidosis).
Mechanism of Injury
The etiology of serum enzyme elevations during linezolid therapy is not known and may relate more to the underlying condition rather than injury from linezolid. Lactic acidosis and peripheral neuropathy from linezolid are probably due to inhibition of mitochondrial ribosomal function and protein synthesis. Indeed, a mitochondrial 16S ribosomal RNA polymorphism [A2706G] has been identified in a high proportion of patients who developed lactic acidosis while on linezolid that may have represented a genetic predisposition to this adverse event. The polymorphism is in the linezolid binding site of the homologous region of bacterial 23S ribosomal RNA and thus the inhibition of mitochondrial ribosomal function may be an off-target but direct toxic effect of linezolid.
Outcome and Management
The serum aminotransferase and alkaline phosphatase elevations that occur during linezolid therapy are self-limited and resolve once therapy is stopped. There are no reports of cross sensitization and hepatic injury from linezolid in persons with hepatic injury from other antibiotics or sulfonamides. The lactic acidosis due to linezolid has been linked to injury to hepatic mitochondria and with microvesicular steatosis, but is usually rapidly reversed with withdrawal of therapy. Treatment with carnitidine, antioxidants, thiamine and prednisone has been used, but has not been shown to be effective. Use of intravenous 20% glucose infusions, which are effective in treating the lactic acidosis of acute fatty liver of pregnancy, Reye syndrome and fialuridine therapy, has not been studied. In some instances hemodialysis has been used to rapidly decrease linezolid levels and help correct electrolyte and fluid imbalance.
Drug Class: Antiinfective Agents, Miscellaneous, Oxazolidinones
Other Drugs in the Subclass, Oxazolidinones: Tedizolid
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Linezolid – Zyvox®
DRUG CLASS
Antiinfective Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Linezolid | 165800-03-3 | C16-H20-F-N3-O4 |
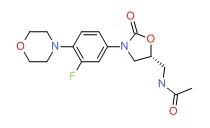 |
ANNOTATED BIBLIOGRAPHY
References updated: 6 June 2019
- Zimmerman HJ. Hepatic injury from the treatment of infectious and parasitic diseases. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999. pp 589-637.(Expert review of hepatotoxicity published in 1999, before the availability of linezolid which is not mentioned).
- Moseley RH. Antibacterial and Antifungal Agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd Edition. Amsterdam: Elsevier, 2013. p. 463-81.(Review of hepatotoxicity of antibiotics; linezolid is not discussed).
- MacDougall C, Chambers HF. Oxazolidinones (Linezolid). Protein synthesis inhibitors; miscellaneous antibacterial agents. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1049-65.(Textbook of pharmacology and therapeutics).
- Stevens DL, Smith LG, Bruss JB, McConnell-Martin MA, Duvall SE, Todd WM, et al. Randomized comparison of linezolid (PNU-100766) versus oxacillin-dicloxacillin for treatment of complicated skin and soft tissue infections. Antimicrob Agents Chemother 2000; 44: 3408-13. [PMC free article: PMC90213] [PubMed: 11083648](836 patients treated for average of 13 days at 133 centers, 2/3 cured, no serious adverse events attributed to linezolid and no "significant" changes in chemistry tests).
- Antony SJ, Diaz-Vasquez E, Stratton C. Clinical experience with linezolid in the treatment of resistant gram-positive infections. J Natl Med Assoc 2001; 93: 386-91. [PMC free article: PMC2594062] [PubMed: 11688919](Among 19 patients with serious resistant Gram positive infections treated with linezolid on a compassionate use basis, 79% had clinical cure; two patients had mild elevations in liver tests, but no details given).
- Kaplan SL, Patterson L, Edwards KM, Azimi PH, Bradley JS, Blumer JL, et al.; Linezolid Pediatric Pneumonia Study Group. Pharmacia and Upjohn. Linezolid for the treatment of community-acquired pneumonia in hospitalized children. Linezolid Pediatric Pneumonia Study Group. Pediatr Infect Dis J 2001; 20: 488-94. [PubMed: 11368105](Phase II trial of iv followed by oral linezolid in 78 children treated for 6 to 41 days; ALT elevations occurred in 6.4% [75-253 U/L], but all resolved in follow up).
- Rubinstein E, Cammarata S, Oliphant T, Wunderink R; Linezolid Nosocomial Pneumonia Study Group. Linezolid (PNU-100766) versus vancomycin in the treatment of hospitalized patients with nosocomial pneumonia: a randomized, double-blind, multicenter study. Clin Infect Dis 2001; 32: 402-12. [PubMed: 11170948](396 patients treated with either linezolid or vancomycin at 90 sites had similar rates of clinical response and side effects; liver tests were abnormal in 1.0% of linezolid vs 1.6% of vancomycin treated patients).
- Apodaca AA, Rakita RM. Linezolid-induced lactic acidosis. N Engl J Med 2003; 348: 86-7. [PubMed: 12510056](52 year old woman developed intractable nausea and vomiting 11 weeks after starting linezolid and was found to have lactic acidosis [9.9 μmol/L] which was reversed after stopping drug; no mention of hepatic abnormalities).
- Bernard L, Stern R, Lew D, Hoffmeyer P. Serotonin syndrome after concomitant treatment with linezolid and citalopram. Clin Infect Dis 2003; 36: 1197. [PubMed: 12715317](81 year old man developed severe lactic acidosis, thrombocytopenia and serotonin syndrome 3 weeks after starting linezolid while also taking citalopram [ALT 66 U/L, CPK 766 U/L, lactate 17.5 μmol/L, pH 6.9], leading to cardiac arrest and hepatic failure, but no information on liver function or histology were given).
- French G. Safety and tolerability of linezolid. J Antimicrob Chemother 2003; 51 (Suppl 2): ii45-53. [PubMed: 12730142](Review of adverse events reported in clinical trials of linezolid reported similar rates of adverse events to comparative drugs; diarrhea, nausea and headache in 1-5%: abnormal "liver tests" in 1.0% vs 0.3% of controls. In one study ALT elevations occurred in 2.5% with low- and 9.8% with high-dose linezolid, all elevations were mild and reversible, and similar in rate to comparative agents; overall ALT >2 times ULN occurred in 7.4% vs 7.2%; list of serious adverse events includes "hepatitis").
- Moellering RC. Linezolid: the first oxazolidinone antimicrobial. Ann Intern Med 2003; 138: 135-42. [PubMed: 12529096](Clinical review of linezolid use; no mention of hepatic injury).
- Rubinstein E, Isturiz R, Standiford HC, Smith LG, Oliphant TH, Cammarata S, et al. Worldwide assessment of linezolid's clinical safety and tolerability: comparator-controlled phase III studies. Antimicrob Agents Chemother 2003; 47: 1824-31. [PMC free article: PMC155822] [PubMed: 12760854](Safety assessment in 2046 patients who received linezolid vs 2001 on comparator drugs found similar rates of diarrhea [4.3 vs 3.2%], nausea [3.4 vs 2.3%], headache [2.2 vs 1.3%], liver test abnormalities [1.0 vs 0.3%], serious adverse events [11.4 vs 10.6%], and deaths [4.8 vs 4.9%]; two patients on oxacillin-dicloxacillin developed "hepatitis", but no cases described for linezolid cohort).
- Stalker DJ, Jungbluth GL, Hopkins NK, Batts DH. Pharmacokinetics and tolerance of single- and multiple-dose oral or intravenous linezolid, an oxazolidinone antibiotic, in healthy volunteers. J Antimicrob Chemother 2003; 51: 1239-46. [PubMed: 12668582](Healthy volunteers given linezolid for up to 18 days had no "clinically important" changes from baseline in laboratory values).
- Palenzuela L, Hahn NM, Nelson RP Jr, Arno JN, Schobert C, Bethel R, Ostrowski LA, et al. Does linezolid cause lactic acidosis by inhibiting mitochondrial protein synthesis? Clin Infect Dis 2005; 40: e113-6. [PubMed: 15909253](Three women, ages 49 to 74, developed lactic acidosis 7-12 weeks after starting linezolid [lactate 9.9 to 18.4 mmol/L] and 2 of the 3 were found to have an polymorphism in mitochondrial 16S rRNA [A2706G] at a site that was homologous to the bacterial 23S rRNA binding site of linezolid).
- Kopterides P, Papadomichelakis E, Armaganidis A. Linezolid use associated with lactic acidosis. Scand J Infect Dis 2005; 37: 153-4. [PubMed: 15764207](Elderly man with severe methicillin-resistant staphylococcus aureus infection developed rising lactate (2.0→12.5 μmol/L) over 7 days of linezolid therapy, resolved with discontinuation, no evidence of liver injury).
- Soriano A, Miró O, Mensa J. Mitochondrial toxicity associated with linezolid. N Engl J Med 2005; 353: 2305-6. [PubMed: 16306535](Three patients with asthenia and lactic acidosis after 1.5-3 months of linezolid therapy were studied for mitochondrial function in peripheral blood mononuclear cells; complex IV enzymatic activity was decreased).
- Bishop E, Melvani S, Howden BP, Charles PG, Grayson ML. Good clinical outcomes but high rates of adverse reactions during linezolid therapy for serious infections: a proposed protocol for monitoring therapy in complex patients. Antimicrob Agents Chemother 2006; 50: 1599-602. [PMC free article: PMC1426936] [PubMed: 16569895](Retrospective analysis of 44 patients treated with linezolid for more than 7 days (8-185 days) found cure in 73%, but adverse reactions in 64%, including 25% requiring ICU care: platelet decreases, anemia, gastrointestinal upset, and 10% with serious adverse events of neuropathy, serotonin syndrome and/or lactic acidosis; recommended prospective monitoring).
- De Vriese AS, Coster RV, Smet J, Seneca S, Lovering A, Van Haute LL, et al. Linezolid-induced inhibition of mitochondrial protein synthesis. Clin Infect Dis 2006; 42: 1111-7. [PubMed: 16575728](Patient treated with linezolid and rifampicin for 4 months developed loss of vision and lactic acidosis [24.5 μmol/L], renal failure and flaccid paralysis; muscle, liver, kidney and white cells were studied; liver showed micro- and macro-vesicular steatosis, decreased activity and protein of respiratory chain complexes I and IV in mitochondria, but normal mtDNA and morphology by electron microscopy).
- Jaksic B, Martinelli G, Perez-Oteyza J, Hartman CS, Leonard LB, Tack KJ. Efficacy and safety of linezolid compared with vancomycin in a randomized, double-blind study of febrile neutropenic patients with cancer. Clin Infect Dis 2006; 42: 597-607. [PubMed: 16447103](Controlled trial of linezolid vs vancomycin for an average of 11 days in 453 patients with cancer and febrile neutropenia found similar safety and efficacy; "the distribution of biochemical test results, including mean values, changes from baseline values and abnormal values, was similar between groups").
- McKee EE, Ferguson M, Bentley AT, Marks TA. Inhibition of mammalian mitochondrial protein synthesis by oxazolidinones. Antimicrob Agents Chemother 2006; 50: 2042-9. [PMC free article: PMC1479116] [PubMed: 16723564](Like chloramphenicol and tetracycline, the oxazolidinones bind to bacterial as well as mitochondrial ribosomes and inhibit protein synthesis, the binding site being conserved between mitochondrial and gram-positive bacteria).
- Pea F, Scudeller L, Lugano M, Baccarani U, Pavan F, Tavio M, et al. Hyperlactacidemia potentially due to linezolid overexposure in a liver transplant recipient. Clin Infect Dis 2006; 42: 434-5. [PubMed: 16392096](59 year old liver transplant recipient developed increased lactate levels after 11 days of linezolid therapy, returning to normal with discontinuation; no mention of other liver tests).
- Narita M, Tsuji BT, Yu VL. Linezolid-associated peripheral and optic neuropathy, lactic acidosis, and serotonin syndrome. Pharmacotherapy 2007; 27: 1189-97. [PubMed: 17655517](Review and summary of published literature on severe side effects of linezolid).
- Vardakas KZ, Ntziora F, Falagas ME. Linezolid: effectiveness and safety for approved and off-label indications. Expert Opin Pharmacother 2007; 8: 2381-400. [PubMed: 17927491](Review of pharmacokinetics, efficacy and safety of linezolid with no mention of hepatic abnormalities).
- Wiener M, Guo Y, Patel G, Fries BC. Lactic acidosis after treatment with linezolid. Infection. 2007; 35: 278-81. [PubMed: 17646908](80 year old woman presented with shortness of breath and lactic acidosis after 19 days of linezolid [pH 7.0, lactate 19 μmol/L], with rapid recovery upon switching to daptomycin).
- Carson J, Cerda J, Chae JH, Hirano M, Maggiore P. Severe lactic acidosis associated with linezolid use in a patient with the mitochondrial DNA A2706G polymorphism. Pharmacotherapy 2007; 27: 771-4. [PubMed: 17461714](35 year old woman with HIV/AIDS developed pancreatitis and lactic acidosis 35 days after starting linezolid [lactate 205 mg/dL, pH 7.16], and sequencing of mitochondrial rRNA showed the A2706G polymorphism described by Palenzuela [2005]).
- Metzxas EI, Falagas ME. Update on the safety of linezolid. Expt Opin Drug Saf 2009; 8: 485-91. [PubMed: 19538105](Summary of pooled results of clinical trials of linezolid in 2046 patients; severe side effects occurred in 0.4% including cytopenia, neurological side effects and lactic acidosis; ALT elevations also occurred, and "some patients had to discontinue treatment because of these abnormalities").
- Savard S, Desmeules S, Riopel J, Agharazii M. Linezolid-associated acute interstitial nephritis and drug rash with eosinophilia and systemic symptoms (DRESS) syndrome. Am J Kidney Dis 2009; 54: e17-20. [PubMed: 19733945](84 year old woman developed pruritus, rash, facial edema and eosinophilia on the 7th day of linezolid therapy with interstitial nephritis and mild hepatitis [AST ~90 U/L, GGT ~105 U/L], with rapid response to prednisone after stopping linezolid).
- De Bus L, Depuydt P, Libbrecht L, Vandekerckhove L, Nollet J, Benoit D, Vogelaers D, Van Vlierberghe H. Severe drug-induced liver injury associated with prolonged use of linezolid. J Med Toxicol 2010; 6: 322-6. [PMC free article: PMC3550492] [PubMed: 20358416](55 year old woman developed jaundice and lactic acidosis after 50 days of linezolid and meropenem therapy [bilirubin 12.1 mg/dL, ALT 113 U/L, Alk P 2486 U/L, pH 7.27, lactate 121 mg/dL], with signs of liver failure, but resolving spontaneously over next 3 months).
- Garazzino S, Tovo PA. Clinical experience with linezolid in infants and children. J Antimicrob Chemother 2011; 66 Suppl 4: iv23-iv41. [PubMed: 21521704](Linezolid has been approved for use in children in whom side effects appear to be less common; transient elevations in serum aminotransferase levels may occur during therapy).
- Gould FK. Linezolid: safety and efficacy in special populations. J Antimicrob Chemother 2011; 66 Suppl 4: iv3-iv6. [PubMed: 21521705](Review that states "Linezolid can induce hepatic transaminases and has been associated with cholestasis, but these abnormalities are infrequent, minor and rarely lead to therapy being truncated").
- Carson J, Cerda J, Chae JH, Hirano M, Maggiore P. Severe lactic acidosis associated with linezolid use in a patient with the mitochondrial DNA A2706G polymorphism. Pharmacotherapy 2007; 27: 771-4. [PubMed: 17461714](35 year old woman developed severe lactic acidosis 35 days after starting linezolid; had mitochondrial DNA polymorphism that may have predisposed her to injury).
- Scotton P, Fuser R, Torresan S, Carniato A, Giobbia M, Rossi C, Inojosa WO, Vaglia A. Early linezolid-associated lactic acidosis in a patient treated for tuberculous spondylodiscitis. Infection 2008; 36: 387-8. [PubMed: 18642110](81 year old woman developed acidosis 12 days after starting intravenous linezolid [pH 7.24, lactate 18.6 mmol/L], isoniazid, rifampin and ethambutol for atypical tuberculosis, recovering within a week of stopping and later tolerating isoniazid, pyrazinamide and rifampin).
- Lee YR, Powell N, Bonatti H, Sawyer RG, Barroso L, Pruett TL, Sifri CD, Volles D. Early development of lactic acidosis with short term linezolid treatment in a renal recipient. J Chemother 2008; 20: 766-7. [PubMed: 19129081](56 year old woman with urosepsis and renal transplant developed metabolic acidosis which worsened with linezolid therapy, but resolved once it was stopped).
- Boutoille D, Grossi O, Depatureaux A, Tattevin P. Fatal lactic acidosis after prolonged linezolid exposure for treatment of multidrug-resistant tuberculosis. Eur J Intern Med 2009; 20: e134-5. [PubMed: 19782904](48 year old man developed lactic acidosis 3 months after starting oral linezolid for resistant tuberculosis [pH 7.32, lactate 11.6 mmol/L], while linezolid was stopped, he was found dead 3 weeks later).
- Fernández de Orueta L, Díaz V, Ramírez M, Alvarez R. [Linezolid-induced lactic acidosis]. Enferm Infecc Microbiol Clin 2009; 27: 550-1. [PubMed: 19819595](72 year old woman developed lactic acidosis beginning 34 days after starting linezolid with severe distress by day 39 [pH 6.93, lactate 6.1 mmol/L], resolving rapidly upon stopping).
- Velez JC, Janech MG. A case of lactic acidosis induced by linezolid. Nat Rev Nephrol 2010; 6: 236-42. [PubMed: 20348931](36 year old man wtih end stage renal disease on dialysis developed lactic acidosis 6 weeks after starting oral linezolid for vancomycin resistant Enterococcus fecalis [pH 7.31, lactate 12.5 mmol/L, ALT 89 U/L], resolving within a week of stopping; ribsomal DNA polymorphism 2706A>G found, similar to two cases in the literature).
- De Bus L, Depuydt P, Libbrecht L, Vandekerckhove L, Nollet J, Benoit D, Vogelaers D, et al. Severe drug-induced liver injury associated with prolonged use of linezolid. J Med Toxicol 2010; 6: 322-6. [PMC free article: PMC3550492] [PubMed: 20358416](55 year old woman developed jaundice and itching 6-7 weeks after starting linezolid and merepenem [bilirubin 12.1 mg/dL, ALT 113 U/L, Alk P 2,486 U/L, pH 7.27, lactate 121 mg/dL], with biopsy showing microvesicular steatosis and slowly resolving after stopping antibiotics, the patient later dying of septic shock).
- Cope TE, McFarland R, Schaefer A. Rapid-onset, linezolid-induced lactic acidosis in MELAS. Mitochondrion 2011; 11: 992-3. [PubMed: 21907311](21 year old man with mitochrondrial encephalomyopathy, lactic acidosis and stroke-like episode syndrome [MELAS] developed tachypnea and rising lactate levels within a day of starting linezolid, returning to baseline rapidly upon stopping).
- Su E, Crowley K, Carcillo JA, Michaels MG. Linezolid and lactic acidosis: a role for lactate monitoring with long-term linezolid use in children. Pediatr Infect Dis J 2011; 30: 804-6. [PMC free article: PMC3158859] [PubMed: 21852764](Three children [0.5, 0.5 and 16 years old], two boys and one girl, with hepatic and or intestinal insufficiency developed lactic acidosis during extended therapy [53, 31 and 7 days] with oral linezolid, resolving rapidly upon stopping in two, but with progressive acidosis and death in 1 child).
- Contou D, Fichet J, Grimaldi D, Cariou A. Early life-threatening lactic acidosis following a single infusion of linezolid. Int J Antimicrob Agents 2011; 38: 84-5. [PubMed: 21482079](81 year old man with chronic hepatitis C on ventilatory support for pneumonia with Enterococcus fecalis superinfection developed lactic acidosis within hours of starting intravenous linezolid [pH 7.03, lactate 16 mmol/L], and resolving within hours of stopping).
- Leach KL, Brickner SJ, Noe MC, Miller PF. Linezolid, the first oxazolidinone antibacterial agent. Ann N Y Acad Sci 2011 Mar; 1222: 49-54. [PubMed: 21434942](Overview from the sponsor of the discovery, development, mechanism of action, pharmacology, and spectrum of activity of linezolid, the first of a new class of antibiotics).
- Garazzino S, Krzysztofiak A, Esposito S, Castagnola E, Plebani A, Galli L, Cellini M, et al. Use of linezolid in infants and children: a retrospective multicentre study of the Italian Society for Paediatric Infectious Diseases. J Antimicrob Chemother 2011; 66: 2393-7. [PubMed: 21764828](Retrospective analysis of 75 hospitalized children who received linezolid for an average of 26 days found that only 2 developed abnormal liver tests [>5 times ULN], but no details provided).
- Simon A, Müllenborn E, Prelog M, Schenk W, Holzapfel J, Ebinger F, Klabunde-Cherwon A, et al. Use of linezolid in neonatal and pediatric inpatient facilities--results of a retrospective multicenter survey. Eur J Clin Microbiol Infect Dis 2012; 31: 1435-42. [PubMed: 22048844](Retrospective analysis of 108 children treated with linezolid [126 courses] in 9 hospitals in Germany and Austria found transiently elevated liver enzymes occurred during 5 courses, but no mention of clinically apparent liver injury).
- Rose PC, Hallbauer UM, Seddon JA, Hesseling AC, Schaaf HS. Linezolid-containing regimens for the treatment of drug-resistant tuberculosis in South African children. Int J Tuberc Lung Dis 2012; 16: 1588-93. [PubMed: 23032215](Among 7 children with multidrug resistant tuberculosis treated with oral linezolid, 3 [all of whom were HIV infected and on antiretroviral therapy] had serious adverse events including 1 with pancreatitis [8 months], 1 with pancreatitis and lactic acidosis [7 months], and 1 with peripheral neuropathy and pancytopenia], 1 with lactic acidosis and 1 with bone marrow hypoplasia, resolving on stopping or lowering the dose of linezolid).
- Miyawaki A, Ueda T, Nakao A, Adachi M, Ohya M, Yamada I, Takesue Y, et al. Linezolid-induced lactic acidosis followed by severe hypophosphatemia after discontinuation of linezolid. Surg Infect (Larchmt) 2013; 14: 229-30. [PubMed: 23464676](75 year old man developed lactic acidosis 72 days after starting oral linezolid [pH 7.09, lactate >25 mmol/L], developing severe hypophosphatemia, but ultimately recoverying completely; no mention of liver injury).
- Kraleti S, Soultanova I. Pancytopenia and lactic acidosis associated with linezolid use in a patient with empyema. J Ark Med Soc 2013; 110: 62-3. [PubMed: 24079055](32 year old man developed pancytopenia, acidosis and enzyme elevations after a 14 day course of linezolid [bilirubin 1.5 mg/dL, ALT 29 U/L, Alk P 192 U/L, lactate 3.7 mmol/L], resolving within 10 days of stopping).
- Holmaas G, Lærum JH, Schjøtt J, Leiva RA. A man in his seventies with a long-term infection and severe acid-base imbalance. Tidsskr Nor Laegeforen 2014; 134: 315-9. [PubMed: 24518482](70 year old man developed lactic acidosis while on long term linezolid [bilirubin not given, ALT 1080 U/L, Alk P normal, INR >7.5, pH 7.03, lactate 27 mmol/L], with prompt improvement on stopping drug).
- Ozkaya-Parlakay A, Kara A, Celik M, Ozsurekci Y, Karadag Oncel E, Ceyhan M, Cengiz AB. Early lactic acidosis associated with linezolid therapy in paediatric patients. Int J Antimicrob Agents 2014; 44: 334-6. [PubMed: 25182713](Among 50 children treated with linezolid for severe infections for 3-93 days, 8 developed lactic acidosis [within 1-13 days] and 8 developed elevated lactate levels, but the elevations resolved despite continuation of therapy).
- Sawyer AJ, Haley HL, Baty SR, McGuffey GE, Eiland EH 3rd. Linezolid-induced lactic acidosis corrected with sustained low-efficiency dialysis: a case report. Am J Kidney Dis 2014; 64: 457-9. [PubMed: 24961626](63 year old man with nocardiosis developed weakness on intravenous linezolid and doxyclycline and was found to have lactic acidosis [pH 7.04, lactate >180 mg/dL], which responded to stopping linezolid and dialysis; no liver tests results provided).
- Del Pozo JL, Fernández-Ros N, Sáez E, Herrero JI, Yuste JR, Banales JM. Linezolid-induced lactic acidosis in two liver transplant patients with the mitochondrial DNA A2706G polymorphism. Antimicrob Agents Chemother 2014; 58: 4227-9. [PMC free article: PMC4068560] [PubMed: 24798272](Two liver transplant recipients [72 year old woman with nocardiosis and 43 year old man with tuberculosis] developed lactic acidosis 13 and 8 weeks after starting linezolid [pH 7.25 and 7.29, lactate 3.2 and 7.2 mmol/L, liver test results not provided], both responding to fluid resuscitation after stopping linezolid and both had the A2707G polymorphism in mitochondrial 16S rRNA).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 323 were attributed to antibiotics, but none to linezolid or other oxazolidinone).
- Blumenthal KG, Youngster I, Rabideau DJ, Parker RA, Manning KS, Walensky RP, Nelson SB. Peripheral blood eosinophilia and hypersensitivity reactions among patients receiving outpatient parenteral antibiotics. J Allergy Clin Immunol 2015; 136: 1288-94. [PMC free article: PMC4640981] [PubMed: 25981739](Among 824 patients receiving outpatient parenteral antibiotic therapy, 210 [25%] developed eosinophilia during treatment [median onset 15 days] inlcuding 10 of 31 recipients of linezolid, none of whom had DRESS syndrome or a serious cutaneous adverse reaction).
- Djibré M, Pham T, Denis M, Pras Landre V, Fartoukh M. Fatal lactic acidosis associated with linezolid therapy. Infection 2015; 43: 125-6. [PubMed: 25326668](70 year old man with cirrhosis and recurrent sepsis developed lactic acidosis and shock 15 days after starting intravenous linezolid [bilirubin 6.7 mg/dL, ALT 20 U/L, AST 117 U/L, Alk P 118 U/L, pH 6.89, lactate 23 mmol/L] and died of multiorgan failure within days of presentation).
- Johnson PC, Vaduganathan M, Phillips KM, O'Donnell WJ. A triad of linezolid toxicity: hypoglycemia, lactic acidosis, and acute pancreatitis. Proc (Bayl Univ Med Cent) 2015; 28: 466-8. [PMC free article: PMC4569226] [PubMed: 26424943](34 year old man with sickle cell disease developed pancreatitis and lactic acidosis 11 days after starting linezolid [lactate 23.5 mmol/L, pH 7.07, glucose 19 mg/dL, liver tests not provided], resolving rapidly upon stopping and administration of glucose; review of history demonstrated a previous episode of lactic acidosis after linezolid was given for 12 days, but not on 3 occasions when it was given for 1-6 days only).
- Hsu SN, Shih MF, Yang CW, Wu CC, Chen CC. Severe linezolid-induced lactic acidosis in a cirrhosis patient. Nephrology (Carlton) 2015; 20: 47-8. [PubMed: 25535870](38 year old woman with alcoholic cirrhosis and renal disease developed lactic acidosis 12 days after starting linezolid [bilirubin 12.4 mg/dL, ALT 23 U/L, AST 64 U/L, INR 3.0, lactate 24 mmol/L, pH 6.9], treated successfully with hemodialysis).
- Im JH, Baek JH, Kwon HY, Lee JS. Incidence and risk factors of linezolid-induced lactic acidosis. Int J Infect Dis 2015; 31: 47-52. [PubMed: 25499040](Among 144 patients with infections treated with either linezolid or telicoplatin in a retrospective, case-control analysis, definite or probable lactic acidosis arose in 5 receiving linezolid [vs none on telicoplatin] after 1-7 weeks, of whom 2 died; no mention of liver test abnormalities).
- Santini A, Ronchi D, Garbellini M, Piga D, Protti A. Linezolid-induced lactic acidosis: the thin line between bacterial and mitochondrial ribosomes. Expert Opin Drug Saf 2017; 16: 833-43. [PubMed: 28538105](Review of the epidemiology, pathophysiology and risk factors for linezolid induced lactic acidosis; mentions 90 cases reported to the FDA, 243 to the European Registry and 48 published cases in adults [9 deaths] and 9 in children [3 deaths]).
- Xiao B, Deng P, Jin H, Wang H, Cao Y. Lactic acidosis and thrombocytopenia associated with linezolid therapy: a case report. Am J Case Rep 2018; 19: 1117-20. [PMC free article: PMC6161563] [PubMed: 30232318](50 year old woman with endocarditis developed lactic acidosis 25 days after starting linezolid [bilirubin 8.3 mg/dL, lactate 19 mmol/L, pH 6.94], dying within weeks of multiorgan failure).
- Mao Y, Dai D, Jin H, Wang Y. The risk factors of linezolid-induced lactic acidosis: A case report and review. Medicine (Baltimore) 2018; 97: e12114. [PMC free article: PMC6133457] [PubMed: 30200095](57 year old man with polymicrobial pneumonia and respiratory failure developed lactic acidosis after 3 doses of linezolid [lactate 10 mmol/L] responding partially to dialysis but ultimately dying from multiorgan failure; literature review identified 47 cases of linezolid associated lactic acidosis with a mortality rate of 26%).
- Tobias PE, Varughese CA, Hanson AP, Gurnani PK. A case of linezolid induced toxicity. J Pharm Pract 2018 Jan 1: 897190018782787. [Epub ahead of print] [PubMed: 29911459](52 year old woman developed abdominal pain and confusion 6 weeks after starting linezolid and a carbapenem for a peritoneal abscess [bilirubin 1.1 mg/dL, ALT 82 U/L, Alk P 228 U/L, glucose 40 mg/dL, lactate 12.2 mmol/L, pH 7.33], resolving upon stopping linezolid, fluid resuscitation and hemodialysis).
- Belani K, Leibowitz A, Bose S. Linezolid-induced lactic acidosis sets stage for surgery to rule out mesenteric ischemia: a case report. A A Pract 2018; 11: 93-5. [PubMed: 29634533](81 year old woman developed lactic acidosis within 12 days of starting linezolid [bilirubin not given, ALT 11 U/L, Alk P 133 U/L, pH 6.89, lactate 14.2 mmol/L] which was initially attributed to intestinal ischemia leading to laparotomy, but then resolved spontaneously within a day of stopping linezolid).
- Cheng CN, Lin SW, Wu CC. Early linezolid-associated lactic acidosis in a patient with Child's class C liver cirrhosis and end stage renal disease. J Infect Chemother 2018; 24: 841-4. [PubMed: 29503228](63 year old man with Child's C cirrhosis developed lactic acidosis 2 weeks after starting linezolid, which resolved rapidly with stopping and did not recur on restarting at a lower dose).
- Mori N, Kamimura Y, Kimura Y, Hirose S, Aoki Y, Bito S. Comparative analysis of lactic acidosis induced by linezolid and vancomycin therapy using cohort and case-control studies of incidence and associated risk factors. Eur J Clin Pharmacol 2018; 74: 405-11. [PubMed: 29222713](Retrospective analyses identified lactic acidosis arising in 10 of 94 patients [11%] receiving linezolid vs 1 of 313 [0.3%] receiving vancomycin; risk factors were duration of therapy and chronic renal disease).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Early linezolid-associated lactic acidosis in a patient with Child's class C liver cirrhosis and end stage renal disease.[J Infect Chemother. 2018]Early linezolid-associated lactic acidosis in a patient with Child's class C liver cirrhosis and end stage renal disease.Cheng CN, Lin SW, Wu CC. J Infect Chemother. 2018 Oct; 24(10):841-844. Epub 2018 Mar 1.
- Review [Linezolid-induced lactic acidosis - a brief overview with a case report].[Klin Mikrobiol Infekc Lek. 2019]Review [Linezolid-induced lactic acidosis - a brief overview with a case report].Pazderkovák J, Kotora V, Dlouhý P, Bartoš H. Klin Mikrobiol Infekc Lek. 2019 Sep; 25(3):92-96.
- Early lactic acidosis associated with linezolid therapy in paediatric patients.[Int J Antimicrob Agents. 2014]Early lactic acidosis associated with linezolid therapy in paediatric patients.Ozkaya-Parlakay A, Kara A, Celik M, Ozsurekci Y, Karadag Oncel E, Ceyhan M, Cengiz AB. Int J Antimicrob Agents. 2014 Oct; 44(4):334-6. Epub 2014 Aug 9.
- Linezolid: a new antibiotic.[Drugs Today (Barc). 2000]Linezolid: a new antibiotic.Xiong YQ, Yeaman MR, Bayer AS. Drugs Today (Barc). 2000 Sep; 36(9):631-9.
- Review Linezolid: an oxazolidinone antimicrobial agent.[Clin Ther. 2001]Review Linezolid: an oxazolidinone antimicrobial agent.Fung HB, Kirschenbaum HL, Ojofeitimi BO. Clin Ther. 2001 Mar; 23(3):356-91.
- Linezolid - LiverToxLinezolid - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...