NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Levetiracetam is a relatively unique anticonvulsant that is typically used in combination with other antiepileptic medications for partial onset seizures. Levetiracetam has been linked to rare instances of serum aminotransferase and alkaline phosphatase elevations during treatment and to rare cases of clinically apparent drug induced liver disease.
Background
Levetiracetam (lee" ve tre ra' se tam) is a pyrrolidine derivative unrelated in structure to other anticonvulsant medications. Its mechanism of action is not known, but it is believed to act by preventing secondary spread of focal seizure activity and to decrease simultaneous neuronal firing. Levetiracetam was approved for use in epilepsy in 1999 and current indications are as adjunctive therapy for partial onset seizures, generalized tonic-clonic seizures and myoclonic seizures in both children and adults. Levetiracetam is available as tablets of 250, 500, 750 and 1000 mg generically and under the brand name Keppra. Extended release tablets, liquid oral formulations and injectable solutions are also available. The recommended initial dose in adults is 500 mg twice daily with dose escalation based upon tolerance and effect to a maximum of 1500 mg twice daily or 3000 mg of extented release formulations once daily. Dosing in children is based upon body weight. Common side effects include dizziness, somnolence, weakness, fatigue, irritability and headache. Rare but potentially serious adverse events include hypersensitivity reactions, rash and cognitive effects including suicidal ideation and behavior.
Hepatotoxicity
Prospective studies reported that chronic levetiracetam therapy was not accompanied by significant elevations in serum aminotransferase levels and clinically apparent liver injury was not observed. Since its approval for use and wide spread availability, however, levetiracetam has been linked to rare instances of serum enzyme elevations and occasional cases of clinically apparent liver injury. The time to onset of liver injury after starting levetiracetam has ranged from 1 week to 5 months and the usual pattern of injury has been hepatocellular. Immunoallergic features and autoantibodies were rare. At least one case of acute liver failure attributed to levetiracetam has been published, but the number of reported cases clinically apparent cases of liver injury has been few. In addition, levetiracetam is usually considered a reasonable alternative therapy in patients who develop anticonvulsant hypersensitivity (DRESS) syndrome after aromatic anticonvulsant use despite the fact that it has been implicated in rare instances of DRESS and Stevens Johnson syndrome.
Likelihood score: C (probable rare cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism of levetiracetam hepatotoxicity is unknown, but is likely to be hypersensitivity. Levetiracetam has minimal hepatic metabolism and does not affect CYP 450 isoenzyme activity.
Outcome and Management
A single case of acute liver failure attributed to levetiracetam has been published. The liver injury recurred rapidly with reexposure. Chronic injury from levetiracetam therapy has not been reported. There is no evidence for cross sensitivity to hepatic injury between levetiracetam and other anticonvulsants.
Drug Class: Anticonvulsants
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Levetiracetam – Generic, Keppra®
DRUG CLASS
Anticonvulsants
COMPLETE LABELING
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Levetiracetam | 102767-28-2 | C8-H14-N2-O2 |
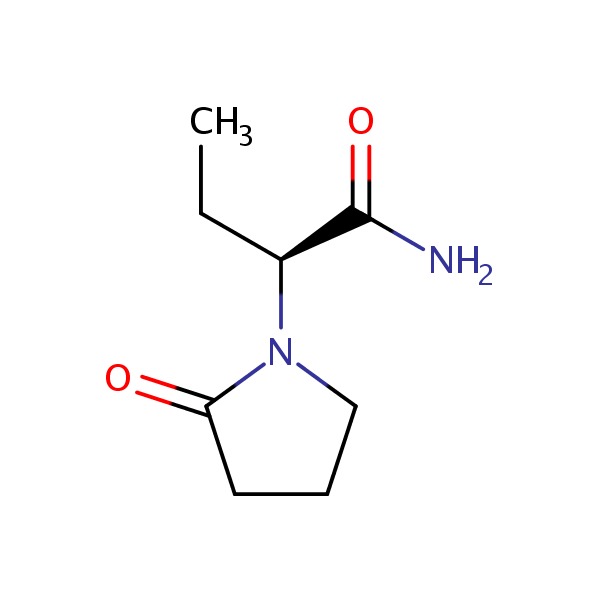 |
ANNOTATED BIBLIOGRAPHY
References updated: 18 April 2019
- Zimmerman HJ. Anticonvulsants. In, Zimmerman, HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999: pp. 498-516.(Expert review of anticonvulsants and liver injury published in 1999; levetiracetam is not discussed).
- Pirmohamed M, Leeder SJ. Anticonvulsant agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013: pp 423-41.(Review of anticonvulsant induced liver injury published in 2013; levetiracetam is not mentioned).
- Smith MD, Metcalf CS, Wilcox KS. Pharmacotherapy of the epilepsies. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 303-26.(Textbook of pharmacology and therapeutics).
- Knowles SR, Shapiro LE, Shear NH. Anticonvulsant hypersensitivity syndrome: incidence, prevention and management. Drug Saf 1999; 21: 489-501. [PubMed: 10612272](Review of anticonvulsant hypersensitivity syndrome: triad of fever, rash and internal organ injury occurring 1-8 weeks after exposure to anticonvulsant; liver being most common internal organ involved. Occurs in 1:1000-1:10,000 initial exposures to phenytoin, carbamazepine, phenobarbital or lamotrigine, unrelated to dose, perhaps predisposed by valproate; liver injury arises 1-4 weeks after onset of rash and ranges in severity from asymptomatic ALT elevations to icteric hepatitis to acute liver failure. High mortality rate with jaundice; other organs involved include muscle, kidney, brain, heart and lung. Pseudolymphoma syndrome and serum sickness like syndrome are separate complications of anticonvulsants. Role of corticosteroids is uncertain; cross reactivity among the agents should be assumed).
- Hamer HM, Morris HH. Hypersensitivity syndrome to antiepileptic drugs: a review including new anticonvulsants. Clevel Clin J Med 1999; 66: 239-45. [PubMed: 10199060](Clinical review of anticonvulsant hypersensitivity syndrome: occurs in 1-5/10,000 users, higher risk in African Americans and affected siblings; liver involvement common, but most cases anicteric; other manifestations include facial edema, lymphadenopathy, bone marrow aplasia, pseudolymphoma, thyroiditis, interstitial nephritis, switching to valproate and benzodiazepines is safe, levetiracetam is also an option).
- Betts T, Waegemans T, Crawford P. A multicentre, double-blind, randomized, parallel group study to evaluate the tolerability and efficacy of two oral doses of levetiracetam, 2000 mg daily and 4000 mg daily, without titration in patients with refractory epilepsy. Seizure 2000; 9: 80-7. [PubMed: 10845730](Comparison of levetiracetam–2000 or 4000 mg daily–compared to placebo as add-on treatment for 24 weeks in 119 patients with refractory seizures; “there were no significant changes in clinical laboratory parameters…” and no specific mention of ALT levels).
- Nash EM, Sangha KS. Levetiracetam. Am J Health Syst Pharm 2000; 58: 1195-9. [PubMed: 11449876](Review of pharmacology and efficacy of levetiracetam, a new anticonvulsant that received rapid approval and is used as adjunctive therapy only; no hepatic metabolism; no mention of hepatic side effects or ALT elevations during therapy).
- Jain KK. An assessment of levetiracetam as an anti-epileptic drug. Exp Opin Invest Drugs 2000; 9: 1611-24. [PubMed: 11060765](Review of levetiracetam use in both partial epilepsy and generalized seizures; no mention of hepatic side effects).
- Partap S, Fisher PG. Levetiracetam for seizures in children with brain tumors and other cancers. Pediatr Blood Cancer 2009; 52: 288-9. [PubMed: 18831033](Extensive review of chemistry, pharmacology, metabolism and pharmacokinetics of levetiracetam; it does not undergo hepatic metabolism, no interaction with CYP 450 isoenzymes and no significant drug-drug interactions).
- Abou-Khalil B. Levetiracetam in the treatment of epilepsy. Neuropsychiatr Dis Treat 2008; 4: 507-23. [PMC free article: PMC2526377] [PubMed: 18830435](Review on use of levetiracetam in epilepsy; serious adverse events are rare; allergic rash in <1%; no mention of hepatic toxicity or ALT elevations).
- Tan TC, de Boer BW, Mitchell A, Delriviere L, Adams LA, Jeffrey GP, Macquillan G. Levetiracetam as a possible cause of fulminant liver failure. Neurology 2008; 71: 685-6. [PubMed: 18725594](Patient developed acute liver failure 1 month after being switched from oxcarbazepine to levetiracetam [bilirubin 34.6 mg/dL, ALT 1610 U/L, Alk P 246 U/L], which recurred on restarting levetiracetam post liver transplant [bilirubin rising to 4.5 mg/dL, ALT 350 U/L, Alk P 650 U/L], resolving within 2 weeks of stopping).
- Skopp G, Schmitt HP, Pedal I. [Fulminant liver failure in a patient on carbamazepine and levetiracetam treatment associated with status epilepticus]. Arch Kriminol 2006; 217: 161-75. German. [PubMed: 16910300](Patient on long term carbamazepine and levetiracetam developed acute liver failure after a period of status epilepticus and mild but prolonged hypotension; autopsy was more compatible with ischemic hepatitis than drug induced liver injury and no routine liver tests [bilirubin, ALT, Alk P, LDH, CPK, protime] provided).
- Briggs DE, French JA. Levetiracetam safety profiles and tolerability in epilepsy patients. Expert Opin Drug Saf 2004; 3: 415-24. [PubMed: 15335297](Analysis of safety in phase II and III prelicensure trials of levetiracetam; adverse events in 15%, most commonly somnolence, asthenia, headache and infection, little change in weight and no reports of hepatotoxicity or ALT elevations).
- Patsalos PN. Clinical pharmacokinetics of levetiracetam. Clin Pharmacokinet 2004; 43: 707-24. [PubMed: 15301575](Review of chemical properties, pharmacokinetics, and pharmacology of levetiracetam which is a pyrrolidone derivative, structurally unrelated to other anticonvulsants, rapid absorption and little hepatic metabolism or effects of CYP isoenzymes).
- LaRoche SM. A new look at the second-generation antiepileptic drugs: a decade of experience. Neurologist 2007; 13: 133-9. [PubMed: 17495757](Review of second generation anticonvulsants approved since 1994 including felbamate, gabapentin, lamotrigine, topiramate, tiagabine, levetiracetam, oxcarbazepine, zonisamide and pregabalin; no mention of liver toxicity from levetiracetam).
- Björnsson E. Hepatotoxicity associated with antiepileptic drugs. Acta Neurol Scan 2008; 118: 281-90. [PubMed: 18341684](Review of all anticonvulsants; suggests that clinically significant hepatotoxicity has not been reported with levetiracetam).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J; Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008; 135: 1924-34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, no case was attributed to levetiracetam).
- Gallerani M, Mari E, Boari B, Carletti R, Marra A, Cavallo M. Pancytopenia associated with levetiracetam treatment. Clin Drug Investig 2009; 29: 747-51. [PubMed: 19813778](65 year old woman developed pancytopenia 9 days after starting levetiracetam followed by pneumonia, gallstone obstruction and multiple liver abscesses [bilirubin 5.4 mg/dL, ALT 127 U/L, Alk P 1169 U/L], ultimately resolving after antibiotic therapy and stopping levetiracetam).
- Broli M, Provini F, Naldi I, Bisulli F, Sama C, Baruzzi A, Tinuper P, Riva R. Unexpected gamma glutamyltransferase rise increase during levetiracetam monotherapy. Epileptic Disord 2010; 12: 81-2. [PubMed: 20159672]PubMed Citation (58 year old woman developed persistent mild and asymptomatic elevations in GGT [initially 29 rising to 157 U/L, ALT normal] 4 months after being switched from valproate to levetiracetam, and resolving within 2 months of switching to lamotrigine).
- Müller CA, Schäfer M, Schneider S, Heimann HM, Hinzpeter A, Volkmar K, Förg A, et al. Efficacy and safety of levetiracetam for outpatient alcohol detoxification. Pharmacopsychiatry 2010; 43: 184-9. PubMed Citation (Controlled trial of 7 days of levetiracetam versus placebo in 131 patients with alcohol dependence during withdrawal; “There were 3 cases of worsening of pre-existing liver parameter elevations”, but no details given). [PubMed: 20503149]
- Richter C, Hinzpeter A, Schmidt F, Kienast T, Preuss UW, Plenge T, Heinz A, et al. Levetiracetam for the treatment of alcohol withdrawal syndrome: a multicenter, prospective, randomized, placebo-controlled trial. J Clin Psychopharmacol 2010; 30: 720-5. PubMed Citation. [PubMed: 21105289](Controlled trial of 7 days of levetiracetam versus placebo in 106 patients with alcohol dependence during withdrawal found no difference in withdrawal symptoms and no “negative influence on laboratory parameters including liver enzymes”).
- Xiong N, Hou L, Lu N, Mohamed AA, Wang T, Huang Y. Probable levetiracetam-related serum alkaline phosphatase elevation. BMC Neurol 2012; 12: 97. [PMC free article: PMC3517503] [PubMed: 22994584](One year old Chinese girl with brain injury was found to have rising levels of Alk P 5 months after starting levetiracetam [Alk P 162 rising to 1613 and then 4557 U/L with normal levels of bilirubin, ALT and GGT], resolving within 6 months of stopping).
- Gómez-Zorrilla S, Ferraz AV, Pedrós C, Lemus M, Peña C. Levetiracetam-induced drug reaction with eosinophilia and systemic symptoms syndrome. Ann Pharmacother 2012; 46: e20. [PubMed: 22764327](31 year old man with brain tumor developed fever, rash and interstitial pneumonitis 49 days after starting levetiracetam, improving with dexamethasone therapy, but recurring [ALT 60 U/L] and resolving only after stopping levetiracetam and switching to phenytoin).
- Sethi NK, Sethi PK, Torgovnick J, Arsura E, Cukierwar F. Asymptomatic elevation of liver enzymes due to levetiracetam: a case report. Drug Metabol Drug Interact 2013; 28: 123-4. [PubMed: 23420283](62 year old woman was found to have serum enzyme elevations without symptoms 10 days after starting levetiracetam therapy [bilirubin not given, ALT 289 U/L, Alk P 567 U/L], which fell to near normal levels within a week of stopping and did not rise with subsequent topiramate therapy).
- Drugs for epilepsy. Treat Guidel Med Lett 2013; 11: 9-18. [PubMed: 23348233](Concise review of the efficacy and safety of drugs used to treat epilepsy; levetiracetam can cause Stevens Johnson syndrome and toxic epidermal necrolysis, but liver adverse events were not mentioned).
- Gutiérrez-Grobe Y, Bahena-Gonzalez JA, Herrera-Gomar M, Mendoza-Diaz P, García-López S, González-Chon O. Acute liver failure associated with levetiracetam and lacosamide combination treatment for unspecified epileptic disorder. Case Rep Emerg Med 2013; 2013: 634174. [PMC free article: PMC3762071] [PubMed: 24027645](22 year old woman with status epilepticus 2 months after starting lacosamide and levetiracetam had markedly abnormal serum enzymes [bilirubin 2.1 mg/dL, ALT 4341 U/L, Alk P 74 U/L, CPK 2989 U/L, myoglobin in serum], falling to normal within 12 days of stopping both drugs).
- Azar NJ, Aune P. Acute pancreatitis and elevated liver transaminases after rapid titration of oral levetiracetam. J Clin Neurosci 2014; 21: 1054-4. [PubMed: 24291473](25 year old woman developed fever, abdominal pain and fatigue within a week of starting levetiracetam [bilirubin 2.7 mg/dL, ALT 1083 U/L, Alk P 250 U/L, amylase 439 U/L], resolving within 7 days of stopping and not recurring with pregabalin).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol 2014; 13: 231-9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, 7 [4%] of which were attributed to anticonvulsants but none to levetiracetam).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-1352.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 40 [4.5%] were due to anticonvulsants but none were attributed to levetiracetam).
- İşgüder R, Güzel O, Ceylan G, Yılmaz Ü, Ağın H. A comparison of intravenous levetiracetam and valproate for the treatment of refractory status epilepticus in children. J Child Neurol 2016; 31: 1120-6. [PubMed: 27080042](Among 78 children with status epilepticus admitted to a Turkish pediatric ICU between 2011 and 2014, liver test abnormalities arose in 4 of 32 receiving intravenous [iv] valproate [peak ALT 4 times ULN] vs none of 46 given iv levetiracetam).
- Selvaraj V, Madabushi JS, Gunasekar P, Singh SP. Levetiracetam associated acute hepatic failure requiring liver transplantation: case report. J Neurol 2016; 263: 814-5. [PubMed: 26902232](50 year old man with epilepsy developed elevated liver tests 8 weeks after starting levetiracetam and olanzapine [bilirubin <1.0 rising to 20.4 mg/dL, ALT 1456 rising to 4300 IU, INR 11], with progressive worsening requiring emergency liver transplantation).
- Rachamallu V, Song MM, Reed JM, Aligeti M. Levetiracetam-induced transaminitis in a young male with traumatic brain injury. Oxf Med Case Reports 2017; 2017 (11): 29744119. [PMC free article: PMC5934633] [PubMed: 29744119](18 year old man with traumatic brain injury developed persistent ALT elevations after starting levetiracetam [61 rising to 311 U/L, no mention of bilirubin or Alk P], which fell to near normal when it was stopped).
- Khoury T, Chen S, Abu Rmeileh A, Daher S, Yaari S, Benson AA, Cohen J, Mizrahi M. Acute liver injury induced by levetiracetam and temozolomide co-treatment. Dig Liver Dis 2017; 49: 297-300. [PubMed: 28034663](A retrospective analysis of 94 patients with brain cancer treated with temozolomide with or without levetireacetam found that liver test abnormalities were more frequent with combination therapy [ALT elevations in 73% vs 10%, Alk P 19% vs 7%, bilirubin in 27% vs 1.5%] and one patient on the combination died of acute liver failure).
- Bunchorntavakul C, Reddy KR. Drug hepatotoxicity: newer agents. Clin Liver Dis 2017; 21: 115-34. [PubMed: 27842767](Review of recently approved drugs that have been associated with liver injury mentions that levetiracetam has little hepatic metabolism but has been associated with transient serum ALT elevations and at least one case of acute liver failure [Tan 2008]).
- Vidaurre J, Gedela S, Yarosz S. Antiepileptic drugs and liver disease. Pediatr Neurol 2017; 77: 23-36. (Review of the use of anticonvulsants in patients with liver disease recommends use of agents that have little hepatic metabolism such as levetiracetam, lacosamide, topiramate, gabapentin and pregabalin, levetiracetam being an "ideal" first line therapy for patients with liver disease because of its safety and lack of pharmacokinetic interactions). [PubMed: 29097018]
- Drugs for epilepsy. Med Lett Drugs Ther 2017; 59 (1526): 121-30. [PubMed: 28746301](Concise review of the drugs available for therapy of epilepsy lists levetiracetam as a drug of choice for partial and generalized seizures as well as for atypical absence, myoclonic and atonic seizures and mentions Stevens Johnson syndrome as a rare adverse event but does not mention ALT elevations or liver injury due to levetiracetam).
- Comparison table: some oral antiepileptic drugs. Med Lett Drugs Ther 2017; 59 (1521): e130-e136. [PubMed: 28746302](Table of oral antiepileptic drugs with listing of oral formulations, usual maintenance dosages, adverse effects, drug interactions, indications and costs; does not mention adverse events of liver injury or ALT elevations for levetiracetam).
- Attilakos A, Dinopoulos A, Paschalidou M, Tsirouda M, Prasouli A, Siafakas N, Garoufi A. Effect of levetiracetam monotherapy on liver enzymes and creatine kinase concentrations in children with epilepsy: a prospective study. J Clin Neurol 2018; 14: 594-595. [PMC free article: PMC6172492] [PubMed: 30284772](Among 26 Korean children with new onset epilepsy started on levetiracetam monotherapy and monitored prospectively for liver test abnormalities, there were minor rises in serum Alk P and GGT but none in ALT, AST or CPK).
- Jayashankar S, Munakomi S, Sayeerajan V, Kafle P, Chaudhary P, Thingujam J, Poudel D, et al. Case report: levetiracetam causing acute liver failure complicating post-operative management in a neurosurgical patient. F1000Res 2019; 8: 187. [PMC free article: PMC6446496] [PubMed: 30984385](55 year old man developed jaundice 3 days after emergency craniotomy for an intra-cerebellar bleed while on levetiracetam [bilirubin 9.4 mg/dL, ALT 926 U/L, Alk P 298 U/L, INR 1.09], resolving within 5 days of stopping).
- Haznedar P, Doğan Ö, Albayrak P, Öz Tunçer G, Teber S, Deda G, Eminoglu FT. Effects of levetiracetam and valproic acid treatment on liver function tests, plasma free carnitine and lipid peroxidation in childhood epilepsies. Epilepsy Res 2019; 153: 7-13. [PubMed: 30925397](In a cross-sectional analysis of 51 children with epilepsy treated with valproate or levetiracetam, serum ALT, AST and GGT levels were in the normal range in all and did not differ from a group of healthy controls).
- Han XD, Koh MJ, Wong SMY. Drug reaction with eosinophilia and systemic symptoms in a cohort of Asian children. Pediatr Dermatol 2019 Mar 28. [Epub ahead of print] [PubMed: 30920020](Among 10 children with DRESS syndrome seen at a single, Singapore referral center between 2006 and 2016, 3 cases were attributed to SMZ/TMP, 2 to carbamazepine, 1 sulfasalazine, 2 phenobarbital and 1 to levetiracetam [latency 28 days]; all had ALT elevations [88 to 1172 U/L], bilirubin was elevated in 7, but none had acute liver failure and none were fatal).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Brivaracetam.[LiverTox: Clinical and Researc...]Review Brivaracetam.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Zonisamide.[LiverTox: Clinical and Researc...]Review Zonisamide.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Safety and efficacy of levetiracetam for the treatment of partial onset seizures in children from one month of age.[Neuropsychiatr Dis Treat. 2013]Safety and efficacy of levetiracetam for the treatment of partial onset seizures in children from one month of age.Cormier J, Chu CJ. Neuropsychiatr Dis Treat. 2013; 9:295-306. Epub 2013 Feb 21.
- Review Antiepileptic drug monotherapy for epilepsy: a network meta-analysis of individual participant data.[Cochrane Database Syst Rev. 2017]Review Antiepileptic drug monotherapy for epilepsy: a network meta-analysis of individual participant data.Nevitt SJ, Sudell M, Weston J, Tudur Smith C, Marson AG. Cochrane Database Syst Rev. 2017 Dec 15; 12(12):CD011412. Epub 2017 Dec 15.
- Review Antiepileptic drug monotherapy for epilepsy: a network meta-analysis of individual participant data.[Cochrane Database Syst Rev. 2017]Review Antiepileptic drug monotherapy for epilepsy: a network meta-analysis of individual participant data.Nevitt SJ, Sudell M, Weston J, Tudur Smith C, Marson AG. Cochrane Database Syst Rev. 2017 Jun 29; 6(6):CD011412. Epub 2017 Jun 29.
- Levetiracetam - LiverToxLevetiracetam - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...