NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Ivabradine is a small molecule inhibitor of the If ion channel which is used to decrease the heart rate in patients with symptomatic heart failure who have a resting heart rate above 70 beats per minute despite optimal doses or intolerance of beta blockers. Ivabradine has not been associated with serum enzyme elevations during therapy or with instances of clinically apparent liver injury.
Background
Ivabradine (eye vab' ra deen) is a small molecule inhibitor of the If ion current, a mixed Na+-K+ inward current that is a major determinant of the sinoatrial pacemaker rate. Ivabradine inhibits the If ion current and lowers heart rate but, unlike beta blockers, does not affect cardiac contractility. In large clinical trials in patients with heart failure in normal sinus rhythm, ivabradine lowered heart rate and decreased episodes of worsening of heart failure and need for hospitalization. Ivabradine was approved for use in the United States in 2015, the indications limited to patients with symptomatic heart failure (ejection fraction 35% or less) in normal sinus rhythm with heart rate above 70 beats per minute despite maximal doses of beta blockers (or contraindications to their use). Ivabradine is available in tablets of 5 and 7.5 mg under the brand name Corlanor. The recommended dose is 5 to 7.5 mg twice daily. Common side effects include bradycardia, hypertension, atrial arrhythmias, dizziness, and blurred vision. Uncommon, but potentially more severe adverse reactions include atrial fibrillation, heart block, syncope, rash, angioedema and fetal toxicity.
Hepatotoxicity
In large preregistration clinical trials, similar proportions of patients taking ivabradine as taking placebo developed ALT elevations [15% vs 17%] while ALT elevations above 5 times the upper limit of normal were uncommon [<1%]. Since its approval and more widespread use, there have been no published cases of liver injury attributable to ivabradine. The product label for ivabradine does not mention hepatotoxicity, but cautions against its use in patients with severe, preexisting liver disease.
Likelihood score: E (unlikely cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism by which ivabradine might cause liver injury is not clear. It is extensively metabolized in the liver largely via CYP 3A4 and is susceptible to drug-drug interactions. Inhibitors of CYP 3A4 cause increase the ivabradine levels, while inducers (such as rifampin) cause reduced serum levels of ivabradine.
Outcome and Management
The serum enzyme elevations that have occurred during ivabradine therapy have been mild and rapidly reversible, often without withdrawal of the agent. Ivabradine has not been linked to cases of acute hepatitis, liver failure, chronic hepatitis or vanishing bile duct syndrome. There is no evidence that there is cross sensitivity to hepatic injury between ivabradine and other oral antiangina or antiarrhythmic agents.
Drug Class: Antiarrhythmic Agents
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Ivabradine – Corlanor®
DRUG CLASS
Antiarrhythmic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Ivabradine | 155974-00-8 | C19-H27-N3-O5-S2 |
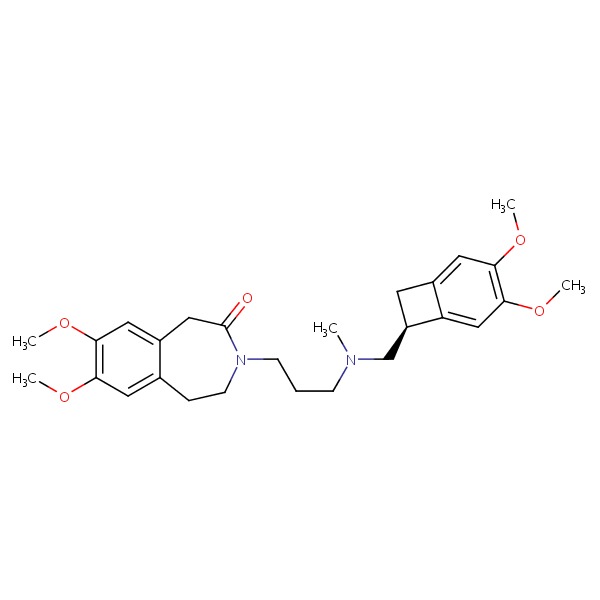 |
ANNOTATED BIBLIOGRAPHY
References updated: 20 April 2017
- Zimmerman HJ. Drugs used in cardiovascular disease. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 639-71.(Expert review of hepatotoxicity published in 1999 before the availability of ivabradine).
- De Marzio DH, Navarro VJ. Hepatotoxicity of cardiovascular and antidiabetic drugs. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 519-40.(Review of hepatotoxicity of cardiovascular drugs; ivabradine is not discussed).
- Maron BA, Rocco TP. Pharmacotherapy of congestive heart failure. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 789-813.(Textbook of pharmacology and therapeutics; ivabradine is not discussed).
- Fox K, Ford I, Steg PG, Tendera M, Ferrari R; BEAUTIFUL Investigators. Ivabradine for patients with stable coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a randomised, double-blind, placebo-controlled trial. Lancet 2008; 372 (9641): 807-16. [PubMed: 18757088](Among 10,917 patients with coronary heart disease and left ventricular ejection fractions less than 40% who were treated with ivabradine vs placebo for an average of 19 months, there were no differences in rates of the primary composite cardiovascular endpoint and no differences in serious adverse event rates between the two groups, while common adverse events from ivabradine were bradycardia and blurred vision; no mention of ALT elevations or hepatotoxicity).
- Swedberg K, Komajda M, Böhm M, Borer JS, Ford I, Dubost-Brama A, Lerebours G, et al.; SHIFT Investigators. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet 2010; 376 (9744): 875-85. [PubMed: 20801495](Among 6558 patients with chronic heart failure in normal sinus rhythm who were treated with ivabradine vs placebo, there were fewer cardiovascular deaths and admissions for heart failure in ivabradine treated patients, and serious adverse events overall were fewer, but side effects more frequent with ivabradine were bradycardia, dizziness and visual disturbances; no mention of ALT elevations or hepatotoxicity).
- Fox K, Ford I, Steg PG, Tardif JC, Tendera M, Ferrari R; SIGNIFY Investigators. Ivabradine in stable coronary artery disease without clinical heart failure. N Engl J Med 2014; 371: 1091-9. [PubMed: 25176136](Among 19,102 patients with stable coronary artery disease without heart failure who were treated with ivabradine or placebo for a median of 28 months, there were no differences in cardiovascular endpoints or mortality, and adverse events were more frequent with ivabradline including bradycardia, atrial fibrillation and "phosphenes" [seeing light without light actually entering the eye]; no mention of ALT elevations or hepatotoxicity).
- Ivabradine (Corlanor) for heart failure. Med Lett Drugs Ther 2015; 57 (1469): 75-6. [PubMed: 25989196](Concise review of the mechanism of action, clinical efficacy, safety and costs of ivabradine shortly after its approval for use in the US; mentions common adverse events and its potential for drug interactions with CYP 3A4 inhibitors or inducers, but does not mention ALT elevations or hepatotoxicity).
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review I(funny) Channel Inhibitors: An Emerging Option for Heart Failure.[CADTH Issues in Emerging Healt...]Review I(funny) Channel Inhibitors: An Emerging Option for Heart Failure.Kim Y, Boucher M, Argáez C. CADTH Issues in Emerging Health Technologies. 2016
- Review Combination Use of Ivabradine with Sacubitril/Valsartan: A Review of Clinical Effectiveness and Guidelines[ 2020]Review Combination Use of Ivabradine with Sacubitril/Valsartan: A Review of Clinical Effectiveness and GuidelinesPohar R, MacDougall D. 2020 Feb 13
- Complementary and Synergic Role of Combined Beta-blockers and Ivabradine in Patients with Chronic Heart Failure and Depressed Systolic Function: A New Therapeutic Option?[Card Fail Rev. 2016]Complementary and Synergic Role of Combined Beta-blockers and Ivabradine in Patients with Chronic Heart Failure and Depressed Systolic Function: A New Therapeutic Option?Volterrani M, Iellamo F. Card Fail Rev. 2016 Nov; 2(2):130-136.
- Ivabradine in stable coronary artery disease without clinical heart failure.[N Engl J Med. 2014]Ivabradine in stable coronary artery disease without clinical heart failure.Fox K, Ford I, Steg PG, Tardif JC, Tendera M, Ferrari R, SIGNIFY Investigators. N Engl J Med. 2014 Sep 18; 371(12):1091-9. Epub 2014 Aug 31.
- The Usefulness of Prioritization of Ivabradine Before Beta-Blockers in a Heart Failure Patient Suffering From Intra-hemodialysis Hypotension.[Cureus. 2023]The Usefulness of Prioritization of Ivabradine Before Beta-Blockers in a Heart Failure Patient Suffering From Intra-hemodialysis Hypotension.Yamaguchi S, Nadoyama N, Kinjo K, Yagi N, Ishimori H, Shimabukuro M. Cureus. 2023 Jun; 15(6):e40609. Epub 2023 Jun 18.
- Ivabradine - LiverToxIvabradine - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...