NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Dronabinol is an orally available cannabinoid agonist that is used to treat nausea and vomiting and to stimulate appetite, particularly in patients with wasting disease or cachexia. Dronabinol is associated with a minimal rate of serum enzyme elevations during therapy and has not been linked to cases of clinically apparent liver injury with jaundice.
Background
Dronabinol (droe nab’ i nol) is the main isomer of tetrahydrocannabinol, the principal psychoactive constituent of the marijuana plant (Cannabis sativa). Dronabinol is a partial agonist of the cannabinoid receptors which are found in the central nervous system (CB1 receptor), but also peripherally (largely CB2 receptors). Activation of CB receptors results in effects on appetite, mood, cognition, memory and perception. Dronabinol therapy has been shown to improve in patients with AIDS related weight loss and to decrease the nausea and vomiting associated with cancer chemotherapy. Dronabinol was approved for use in the United States in 1985 and current indications include treatment of anorexia associated with weight loss in patients with AIDS, and prevention of cancer chemotherapy associated nausea and vomiting. Dronabinol is available as 2.5, 5 and 10 mg capsules generically and under the brand name Marinol. The typical adult oral dose is 2.5 mg twice daily, which can be increased based upon tolerance and effect to a maximum of 20 mg/day. Common side effects include fatigue, somnolence, dizziness, euphoria, abnormal thinking, paranoid reactions, conjunctivitis, diarrhea, nausea, vomiting and abdominal pain. Rare side effects include hallucinations and seizures. Dronabinol is classified as a Schedule III drug, indicating that it has mild potential for physical and psychological dependency and abuse.
Hepatotoxicity
Serum aminotransferase elevations during dronabinol therapy were reported to occur in 6% of treated patients compared to 4.3% in controls who receiving cancer chemotherapy. The aminotransferase elevations were transient, mild-to-moderate in severity, and not associated with symptoms or jaundice. There have been no convincing cases of clinically apparent liver injury attributable to dronabinol published in the literature and, thus, significant liver injury from dronabinol must be exceeding rare, if it occurs at all.
Likelihood score: E (unlikely cause of clinically apparent liver injury).
Mechanism of Injury
Dronabinol is metabolized by the liver and undergoes extensive first-pass metabolism to both active and inactive metabolites. Despite its hepatic metabolism and high level of plasma protein binding, it has not been implicated in causing drug-drug interactions. The lack of reported cases of liver injury due to dronabinol may be due to the low doses of typical therapy.
Drug Class: Gastrointestinal Agents, Antiemetics
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Dronabinol – Generic, Marinol®
DRUG CLASS
Gastrointestinal Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
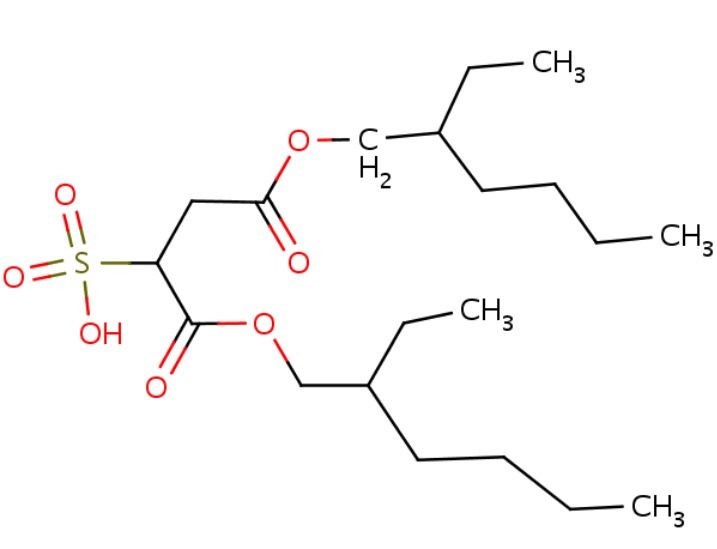
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Dronabinol | 1972-08-3 | C21-H30-O2 |
 |
REFERENCES
References updated: 15 January 2018
- Zimmerman HJ. Antiemetic and prokinetic compounds. Miscellaneous drugs and diagnostic chemicals. In, Zimmerman, HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999: pp. 721.(Expert review of hepatotoxicity published in 1999 does not discuss dronabinol).
- Sharkey KA, Wallace JL. Treatment of disorders of bowel motility and water flux: anti-emetics; agents used in biliary and pancreatic disease. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1323-50.(Textbook of pharmacology and therapeutics).
- Marijuana. In, PDR for Herbal Medicines. 4th ed. Montvale, New Jersey: Thomson Healthcare Inc. 2007: pp. 562-7.(Compilation of short monographs on herbal medications and dietary supplements).
- Fabre LF, McLendon D. The efficacy and safety of nabilone(a synthetic cannabinoid) in the treatment of anxiety. J Clin Pharmacol 1981; 21: 377S-382S. [PubMed: 6117575](Among 25 patients with anxiety disorders participating in dose finding studies of nabilone for up to 28 days, the most common side effects were dry mouth and eyes, drowsiness, headaches and insomnia; "nabilone did not alter any value in the clinical chemistry battery").
- Beal JE, Olson R, Laubenstein L, Morales JO, Bellman P, Yangco B, Lefkowitz L, et al. Dronabinol as a treatment for anorexia associated with weight loss in patients with AIDS. J Pain Symptom Manage 1995; 10: 89-97. [PubMed: 7730690](Among 139 patients with AIDS related anorexia and weight loss treated with dronabinol or placebo for up to 4 weeks, side effects included euphoria, dizziness, drowsiness and difficulty thinking and "no treatment-related toxicity was found on... laboratory tests").
- Beal JE, Olson R, Lefkowitz L, Laubenstein L, Bellman P, Yangco B, Morales JO, et al. Long-term efficacy and safety of dronabinol for acquired immunodeficiency syndrome-associated anorexia. J Pain Symptom Manage 1997; 14: 7-14. [PubMed: 9223837](Among 94 patients with late stage AIDS treated with dronabinol [2.5-5 mg daily] for up to 12 months, there were "no significant changes in hematology or blood chemistry parameters").
- Wissel J, Haydn T, Müller, Brenneis C, Berger T, Poewe W, Schelosky LD. Low dose treatment with the synthetic cannabinoid Nabilone significantly reduces spasticity-related pain: a double-blind placebo-controlled cross-over trial. J Neurol 2006; 253: 1337-41. [PubMed: 16988792](Among 13 patients with upper motor neuron disease and spasticity treated with nabilone [1 mg daily] for up to 9 weeks, pain and spasticity decreased and "no severe side effects were reported").
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J; Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008; 135: 1924-34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, no cases were attributed to cannabinoid agonists or antiemetics).
- Reuben A, Koch DG, Lee WM; Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology 2010; 52: 2065-76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, but none were attributed to antiemetic agents).
- Levin FR, Mariani JJ, Brooks DJ, Pavlicova M, Cheng W, Nunes EV. Dronabinol for the treatment of cannabis dependence: a randomized, double-blind, placebo-controlled trial. Drug Alcohol Depend 2011; 116: 142-50. [PMC free article: PMC3154755] [PubMed: 21310551](Among 156 cannabinoid dependent adults treated with dronabinol or placebo for up to 8 weeks, withdrawal symptoms were less with dronabinol therapy and there were no serious adverse events that could be linked to its use).
- Zajicek J, Ball S, Wright D, Vickery J, Nunn A, Miller D, Gomez Cano M, et al.; CUPID investigator group. Effect of dronabinol on progression in progressive multiple sclerosis (CUPID): a randomised, placebo-controlled trial. Lancet Neurol 2013; 12: 857-65. [PMC free article: PMC3744749] [PubMed: 23856559](In a study of 498 patients with multiple sclerosis treated with dronabinol or placebo for up to 3 years, dronabinol had no effect on disease progression and did not increase the rate of serious or nonserious side effects, except for drowsiness and dissociative thinking).
- Borgelt LM, Franson KL, Nussbaum AM, Wang GS. The pharmacologic and clinical effects of medical cannabis. Pharmacotherapy 2013; 33: 195-209. [PubMed: 23386598](Review of history and status of cannabis used for medical purposes including severe pain, muscle spasms, anorexia, nausea and vomiting, and glaucoma; adverse events are common, but usually mild and reversible, most frequently dry mouth, dizziness, drowsiness, and changes in cognition and mood).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 2013; 144: 1419-25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, but none were attributed to antiemetics).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol 2014; 13: 231-9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, the most common implicated agents being nimesulide [n=53: 30%], cyproterone [n=18], nitrofurantoin [n=17], antituberculosis drugs [n=13], and flutamide [n=12: 7%]; no antiemetic was listed).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52.e7. PubMed Citation. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, none were attributed to dronabinol or other canabinoids).
- van den Elsen GAH, Ahmed AIA, Verkes RJ, Feuth T, van der Marck MA, Olde Rikkert MGM. Tetrahydrocannabinol in behavioral disturbances in dementia: A crossover randomized controlled trial. Am J Geriatr Psychiatry 2015; 23: 1214-24. [PubMed: 26560511](Among 22 patients with dementia treated with tetrahydrocannabinol [THC] or placebo in a crossover controlled trial, THC did not reduce neuropsychiatric symptoms but was well tolerated; no mention of ALT levels or hepatotoxicity).
- van den Elsen GA, Ahmed AI, Verkes RJ, Kramers C, Feuth T, Rosenberg PB, van der Marck MA, et ak. Tetrahydrocannabinol for neuropsychiatric symptoms in dementia: A randomized controlled trial. Neurology 2015; 84: 2338-46. [PMC free article: PMC4464746] [PubMed: 25972490](Among 50 patients with dementia treated with tetrahydrocannabinol [THC] or placebo for 3 weeks, there were no differences in changes in neuropsychiatric symptom scores and adverse event rates were similar; no mention of ALT elevations or hepatotoxicity).
- Levin FR, Mariani JJ, Pavlicova M, Brooks D, Glass A, Mahony A, Nunes EV, et al. Dronabinol and lofexidine for cannabis use disorder: A randomized, double-blind, placebo-controlled trial. Drug Alcohol Depend 2016; 159: 53-60. [PMC free article: PMC4729291] [PubMed: 26711160](Among 156 patients with cannabis-dependency treated with dronabinol and lofexidine [alpha-2 agonist] vs placebo for 11 weeks, there were no differences in rates of abstinence and no liver related serious adverse events; changes in ALT levels were not reported).
- Schimrigk S, Marziniak M, Neubauer C, Kugler EM, Werner G, Abramov-Sommariva D. Dronabinol Is a safe long-term treatment option for neuropathic pain patients. Eur Neurol 2017; 78 (5-6): 320-9. [PMC free article: PMC5804828] [PubMed: 29073592](Among 240 patients with multiple sclerosis and neuropathic pain treated with dronabinol or placebo for 16 weeks, changes in pain intensity scores were similar in the 2 groups, but adverse events of dizziness, dry mouth and diarreha were more common with dronabinol; among 100 subjects continued on dronabinol for up to 69 weeks, adverse events decreased and there were no serious liver related adverse events).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Nabilone.[LiverTox: Clinical and Researc...]Review Nabilone.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- A 4-week pilot study with the cannabinoid receptor agonist dronabinol and its effect on metabolic parameters in a randomized trial.[Clin Ther. 2015]A 4-week pilot study with the cannabinoid receptor agonist dronabinol and its effect on metabolic parameters in a randomized trial.Reichenbach ZW, Sloan J, Rizvi-Toner A, Bayman L, Valestin J, Schey R. Clin Ther. 2015 Oct 1; 37(10):2267-74. Epub 2015 Aug 14.
- Urinary cannabinoid mass spectrometry profiles differentiate dronabinol from cannabis use.[Clin Chim Acta. 2020]Urinary cannabinoid mass spectrometry profiles differentiate dronabinol from cannabis use.Koch CD, Xu L, Curtis SA, Roberts JD, Bunch DR, El-Khoury JM. Clin Chim Acta. 2020 Nov; 510:515-521. Epub 2020 Aug 12.
- Review Dronabinol for chemotherapy-induced nausea and vomiting unresponsive to antiemetics.[Cancer Manag Res. 2016]Review Dronabinol for chemotherapy-induced nausea and vomiting unresponsive to antiemetics.May MB, Glode AE. Cancer Manag Res. 2016; 8:49-55. Epub 2016 May 12.
- Dronabinol and prochlorperazine in combination for treatment of cancer chemotherapy-induced nausea and vomiting.[J Pain Symptom Manage. 1991]Dronabinol and prochlorperazine in combination for treatment of cancer chemotherapy-induced nausea and vomiting.Lane M, Vogel CL, Ferguson J, Krasnow S, Saiers JL, Hamm J, Salva K, Wiernik PH, Holroyde CP, Hammill S. J Pain Symptom Manage. 1991 Aug; 6(6):352-9.
- Dronabinol - LiverToxDronabinol - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...