NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Crizotinib is a selective tyrosine kinase receptor inhibitor used in the therapy of selected cases of advanced non-small cell lung cancer. Crizotinib is associated with transient elevations in serum aminotransferase levels during treatment and rare instances of clinically apparent acute liver injury that can be severe and even fatal.
Background
Crizotinib (kriz oh’ ti nib) is an orally available, small molecule inhibitor of the tyrosine kinase receptor of mutated anaplastic lymphoma kinase (ALK), which is the result of a chromosomal translocation found in about 5% of lung cancers. Patients with non-small cell lung cancer with the ALK mutation often respond to crizotinib therapy with shrinkage of the tumor and apparent improvement in survival. Crizotinib received accelerated approval for use in the United States in 2011 for the treatment of advanced non-small cell lung cancer with the ALK translocation (a test for this genetic rearrangement was also approved). Crizotinib is available in capsules of 200 and 250 mg under the brand name Xalkori. The recommended dose is 250 mg by mouth twice daily, with dose modification based upon tolerance. Side effects are common and include diarrhea, nausea, vomiting, anorexia, fatigue, constipation, visual disturbances and edema. Uncommon, but potentially serious side effects include interstitial lung disease, QTc interval prolongation and bradycardia.
Hepatotoxicity
In large early clinical trials, elevations in serum aminotransferase levels occurred in up to 57% of patients treated with standard doses of crizotinib, were greater than 5 times ULN in 6% of patients, and led to early discontinuation of therapy in 2% to 4% of patients. Serum aminotransferase elevations typically arose after 4 to 12 weeks of treatment, but usually without jaundice or alkaline phosphatase elevations. Restarting crizotinib after resolution of the aminotransferase abnormalities can be done starting with a reduced dose. Most cases of liver injury due to crizotinib have been minimally or not symptomatic, and the injury resolved within 1 to 2 months of stopping the drug (Case 1). However, cases with jaundice and symptoms during crizotinib therapy have been reported which were fatal in 0.1% of treated patients (Case 2). The severe cases of liver injury due to crizotinib typically arose within 2 to 6 weeks of starting therapy and presented with marked elevations in serum aminotransferase levels followed by jaundice, progressive hepatic dysfunction, coagulopathy, encephalopathy and death. For these reasons, routine periodic monitoring of liver tests at 2 to 4 week intervals during therapy is recommended.
Likelihood score: C (probable cause of clinically apparent acute liver injury).
Mechanism of Injury
The cause of the liver injury due to crizotinib is unknown. Crizotinib is metabolized in the liver largely via CYP 3A4, and liver injury may be due to accumulation of a toxic or immunogenic intermediate. Crizotinib is susceptible to drug-drug interactions with medications that inhibit or induce CYP 3A4.
Outcome and Management
Routine monitoring of liver tests are recommended for patients starting crizotinib, including serum ALT, AST and bilirubin every 2 weeks for the first 2 months and monthly thereafter and as clinically indicated. Serum aminotransferase elevations above 5 times the upper limit of normal (if confirmed) should lead to dose interruption. If changes persist, are severe, or reoccur on restarting, crizotinib should be discontinued. There have been reports of acute liver failure, but not of chronic hepatitis or vanishing bile duct syndrome due to crizotinib. Patients with liver abnormalities during crizotinib therapy may tolerate other kinase inhibitors active against non-small cell lung cancer such as erlotinib or gefitinib.
Drug Class: Antineoplastic Agents, Protein Kinase Inhibitors
CASE REPORTS
Case 1. Serum aminotransferase elevations during crizotinib therapy.
[Modified from: Ripault MP, Pinzani V, Fayolle V, Pageaux GP, Larrey D. Crizotinib-induced acute hepatitis: first case with relapse after reintroduction with reduced dose. Clin Res Hepatol Gastroenterol 2013; 37: e21-3. PubMed Citation]
A 69 year old woman with metastatic non-small cell lung cancer developed fatigue 2 months after starting crizotinib (500 mg daily). She had no history of liver disease, risk factors for viral hepatitis or alcohol abuse. Her only other medications were low doses of aspirin (75 mg daily). Physical examination was normal. Laboratory tests showed normal serum bilirubin, but ALT 159 U/L (4.8 times ULN), AST 98 U/L (3 times ULN), but normal alkaline phosphatase, GGT and prothrombin time. Her liver tests had been normal before starting crizotinib (Table). Tests for hepatitis A, B, C and E, CMV, Epstein Barr virus and herpes simplex virus were negative and autoantibodies were not present. Imaging of the liver was normal. Crizotinib was stopped and liver tests improved and were near normal one month later when crizotinib was restarted. Two weeks later, serum aminotransferase levels were again elevated and crizotinib was permanently discontinued.
Key Points
| Medication: | Crizotinib (500 mg daily) |
| Pattern: | Hepatocellular (R=~5) |
| Severity: | 1+ (serum enzyme elevations without jaundice) |
| Latency: | 8 weeks |
| Recovery: | 6 weeks |
| Other medications: | Aspirin |
Laboratory Values
| Time After Starting* | Time After Stopping | ALT (x ULN) | Alk P | Bilirubin (mg/dL) | Other |
|---|---|---|---|---|---|
| 0 | Pre | <1 | Normal | Normal | |
| 3 weeks | Pre | 1.2 | Normal | Normal | |
| 8 weeks | 0 | 4.8 | Normal | Normal | Crizotinib stopped |
| 10 weeks | 2 weeks | 3.2 | Normal | Normal | |
| 13 weeks | 5 weeks | 1.3 | Normal | Normal | Crizotinib restarted |
| 15 [2] weeks | 0 | 5.3 | Normal | Normal | Crizotinib restopped |
| 16 [3] weeks | 1 week | 2.7 | Normal | Normal | |
| 17 [4] weeks | 2 weeks | 1.4 | Normal | Normal | |
| 22 [9] weeks | 7 weeks | <1 | Normal | Normal | |
| Normal Values | <1 | ||||
*Values in brackets represent number of weeks after restarting crizotinib.
Comment
Elevations in serum aminotransferase levels occur in up to 57% of patients treated with crizotinib, but they are usually mild and self-limited. Elevations above 5 times the upper limit (approximately 200 U/L) arise in 5% to 17% of patients and even then may not require drug discontinuation. In this patient, the serum aminotransferase elevations were mild-to-moderate in severity (ALT never rose above 200 U/L), but were associated with symptoms of fatigue. The elevations resolved rapidly upon stopping therapy, but then reappeared with restarting even at a lower dose. The patient was never jaundiced, and alkaline phosphatase and GGT levels were normal. The symptoms were not clearly described and may not have been due to the liver injury, as crizotinib can cause fatigue independent of liver injury. In most patients (but not this one), serum ALT elevations resolve spontaneously either with continuation of therapy or with stopping and restarting at a lower dose.
Case 2. Fatal liver injury during crizotinib therapy.
[Modified from: van Geel RM, Hendrikx JJ, Vahl JE, van Leerdam ME, van den Broek D, Huitema AD, Beijnen JH,et al. Crizotinib-induced fatal fulminant liver failure. Lung Cancer 2016; 93: 17-9. PubMed Citation]
A 62 year old woman with metastatic non-small cell lung cancer [NSCLC] developed abnormal ALT levels 17 days after starting crizotinib [250 mg twice daily], but was continued on therapy until one week later when liver test results were found to have worsened (Table). Crizotinib was stopped but she developed diarrhea, fatigue and jaundice one week later and was admitted. She had no history of liver disease, did not drink alcohol and was taking no other potentially hepatoxic medications. Tests for hepatitis A, B, C and E were negative and ultrasound of the abdomen showed no evidence of biliary obstruction or hepatic masses. She was treated for hepatic failure but devleoped coma, multiorgan failure and died 40 days after starting and 16 days after stopping crizotinib.
Key Points
| Medication: | Crizotinib (250 mg twice daily) |
| Pattern: | Hepatocellular (estimated R=~100) |
| Severity: | 5+ (hepatic failure and death) |
| Latency: | 2 weeks |
| Recovery: | None |
| Other medications: | Not listed |
Laboratory Values
| Time After Starting* | Time After Stopping | ALT* (U/L) | Alk P (U/L) | Bilirubin* (mg/dL) | Other |
|---|---|---|---|---|---|
| 0 | 19 | 184 | 1.0 | Crizotinib started | |
| 7 days | 44 | 0.2 | |||
| 17 days | 2062 | 0.3 | Asymptomatic | ||
| 24 days | 0 | 6194 | 1.5 | Crizotinib stopped | |
| 31 days | 7 days | ~980 | 16.8 | Symptomatic | |
| 33 days | 9 days | ~600 | ~20.0 | Admitted | |
| 35 days | 11 days | ~400 | ~19.4 | Coma | |
| 40 days | 16 days | ~100 | ~25.9 | Died | |
| Normal Values | <40 | <130 | <1.2 | ||
*Some values estimated from Figure 1.
Comment
This patient developed marked serum aminotransferase elevations within 2 to 3 weeks of starting crizotinib, but was asymptomatic and therapy was not stopped until values were found to continue to rise. Despite stopping, she became jaundiced and rapidly developed hepatic failure, coagulopathy, liver coma and died. The abruptness of onset and severe course suggests a direct hepatotoxicity, but is also compatible with idiosyncracy. Routine monitoring was performed, but the results were not obtained until retrospectively from the critical 17 day time point. Listing of other medications, even if not known to be hepatoxic, would be helpful as crizotinib has extensive hepatic metabolism, largely via CYP 3A4 and is susceptible to drug-drug interactions. Use of potent CYP3A inhibitors or inducers should be avoided during crizotinib therapy.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Crizotinib – Xalkori®
DRUG CLASS
Antineoplastic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Crizotinib | 877399-52-5 | C21-H22-Cl2-F-N5-O |
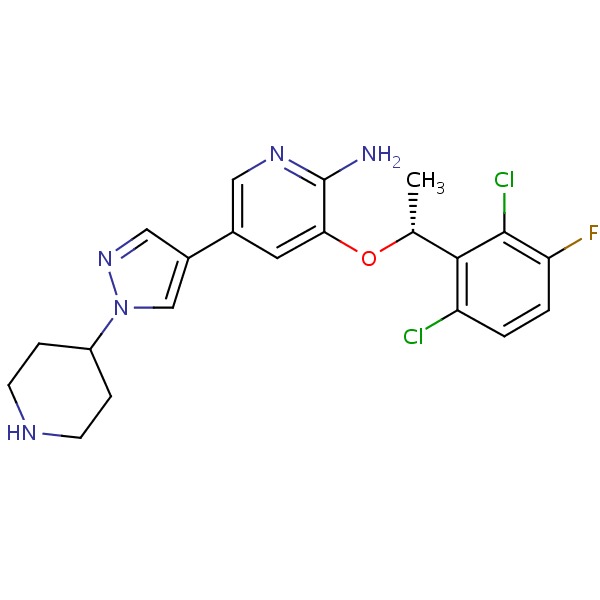 |
ANNOTATED BIBLIOGRAPHY
References updated: 30 October 2017
Abbreviations used: NSCLC, non-small cell lung cancer; ALK, anaplastic lymphoma kinase.
- Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999.(Review of hepatotoxicity published in 1999 before the availability of tyrosine kinase receptor inhibitors).
- DeLeve LD. Kinase inhibitors. Gefitinib. Cancer chemotherapy. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, p. 556.(Review of hepatotoxicity of cancer chemotherapeutic agents; crizotinib is listed as causing moderate-to-severe aminotransferase elevations in 4-7% of patients and as having caused fatal hepatotoxicity in some instances).
- Chabner BA, Barnes J, Neal J, Olson E, Mujagic H, Sequist L, Wilson W, et al. Targeted therapies: tyrosine kinase inhibitors, monoclonal antibodies, and cytokines. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1731-54.(Textbook of pharmacology and therapeutics).
- Kwak EL, Bang YJ, Camidge DR, Shaw AT, Solomon B, Maki RG, Ou SH, et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med 2010; 363: 1693-703. [PMC free article: PMC3014291] [PubMed: 20979469](Screening 1500 patients identified 82 with ALK-positive non-small cell lung cancer [NSCLC], 47 of whom responded at least partially to crizotinib; common side effects were nausea, diarrhea, visual blurring, constipation and fatigue; ALT or AST elevations of above 5 times ULN occurred in 5 patients [5%], all except one of whom could restart the drug at a lower dose without recurrence).
- Camidge DR, Bang YJ, Kwak EL, Iafrate AJ, Varella-Garcia M, Fox SB, Riely GJ, et al. Activity and safety of crizotinib in patients with ALK-positive non-small-cell lung cancer: updated results from a phase 1 study. Lancet Oncol 2012; 13: 1011-9. [PMC free article: PMC3936578] [PubMed: 22954507](Among 149 patients with NSCLC with ALK mutations treated with crizotinib, 61% had an objective response and 97% had at least one adverse event, the most common being visual effects [64%], nausea [56%] and diarrhea [50%], with ALT elevations occurring in 10% and being above 5 times ULN in 3%; among 46 deaths, none were considered drug related).
- Girard N. Crizotinib in ALK-positive lung cancer. Lancet Oncol 2012; 13: 962-3. [PubMed: 22954506](Editorial in response to Camidge [2012] with no discussion of potential for hepatotoxicity or ALT elevations).
- Crizotinib (Xalkori) for non-small cell lung cancer. Med Lett Drugs Ther 2012; 54 (1383): 11-2. [PubMed: 22354221](Concise review of mechanism of action, efficacy, safety and costs of crizotinib shortly after its accelerated approval in the US; mentions rare, but sometimes severe adverse effects of pneumonitis and QTc prolongation, but does not mention hepatotoxicity).
- Ripault MP, Pinzani V, Fayolle V, Pageaux GP, Larrey D. Crizotinib-induced acute hepatitis: first case with relapse after reintroduction with reduced dose. Clin Res Hepatol Gastroenterol 2013; 37: e21-3. [PubMed: 23182672](69 year old woman with NSCLC developed fatigue and ALT elevations 8 weeks after starting crizotinib [ALT 159 U/L, bilirubin and Alk P normal], resolving within 6 weeks of stopping and recurring [ALT 175 U/L] with restarting: Case 1).
- Shaw AT, Engelman JA. ALK in lung cancer: past, present, and future. J Clin Oncol 2013; 31: 1105-11. [PMC free article: PMC4209068] [PubMed: 23401436](Review of the history of discovery of ALK mutations and development of crizotinib as therapy of NSCLC patients with this mutation; no discussion of hepatotoxicity or ALT elevations).
- Shah RR, Morganroth J, Shah DR. Hepatotoxicity of tyrosine kinase inhibitors: clinical and regulatory perspectives. Drug Saf 2013; 36: 491-503. [PubMed: 23620168](Review of the hepatotoxicity of 18 tyrosine kinase inhibitors approved for use in cancer in the US as of 2013; crizotinib is listed as causing liver enzyme elevations in up to 57% of patients [above 5 times ULN in 6%] and having been linked to cases of hepatitis and fatal hepatic failure).
- Timm A, Kolesar JM. Crizotinib for the treatment of non-small-cell lung cancer. Am J Health Syst Pharm 2013; 70: 943-7. [PubMed: 23686600](Review of role of crizotinib in therapy of NSCLC mentions that ALT elevations above 5 times ULN occur in 6.7% of patients).
- Shaw AT, Kim DW, Nakagawa K, Seto T, Crinó L, Ahn MJ, De Pas T, et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med 2013; 368: 2385-94. [PubMed: 23724913](Among 347 adults with refractory, advanced, ALK-positive lung cancer treated with crizotinib [250 mg twice daily] or conventional chemotherapy [pemetrexed or docetaxel intravenously every 3 weeks], progression free survival was longer with crizotinib [7.7 vs 3 months] and adverse events included ALT or AST elevations in 38% vs 15%, which were above 5 times ULN in 16% vs 2%, and one patient [0.5%] died of liver failure).
- Mossé YP, Lim MS, Voss SD, Wilner K, Ruffner K, Laliberte J, Rolland D, et al. Safety and activity of crizotinib for paediatric patients with refractory solid tumours or anaplastic large-cell lymphoma: a Children's Oncology Group phase 1 consortium study. Lancet Oncol 2013; 14: 472-80. [PMC free article: PMC3730818] [PubMed: 23598171](Among 79 children with various forms of refractory solid tumors or lymphomas treated with one of 6 doses of crizotinib, ALT elevations occurred in 62% of patients with the first cycle and were above 5 times ULN in 4%; no mention of clinically apparent lier injury).
- Sato Y, Fujimoto D, Shibata Y, Seo R, Suginoshita Y, Imai Y, Tomii K. Fulminant hepatitis following crizotinib administration for ALK-positive non-small-cell lung carcinoma. Jpn J Clin Oncol 2014; 44: 872-5. [PubMed: 24966207](54 year old woman with advanced, ALK-positive lung cancer developed malaise 29 days after starting crizotinib [bilirubin 2.7 rising to 4.7 mg/dL, ALT 5201 U/L, Alk P 506 U/L, prothrombin index less than 10%], with progressive liver failure and death 6 days after presentation).
- Tsukita Y, Fukuhara T, Kobayashi M, Morita M, Suzuki A, Watanabe K, Noguchi T, et al. Alternate-day treatment with crizotinib for drug-induced esophagitis and liver damage in a patient with EML4-ALK fusion gene-positive lung adenocarcinoma. Intern Med 2015; 54: 3185-8. [PubMed: 26666609](44 year old woman with refractory, metastatic ALK-positive lung cancer developed esophagitis and ALT elevation shortly after starting crizotinib, which improved upon stopping and did not recur on restarting at a reduced dose [alternative day, actual dose not given]).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 49 cases [6%] were attributed to antineoplastic agents, including 9 due to kinase inhibitors such as imatinib and lapatinib, but none were attributed to crizotinib).
- van Geel RM, Hendrikx JJ, Vahl JE, van Leerdam ME, van den Broek D, Huitema AD, Beijnen JH, et al. Crizotinib-induced fatal fulminant liver failure. Lung Cancer 2016; 93: 17-9. [PubMed: 26898609](62 year old woman with advanced, ALK-positive NSCLC developed liver test abnormalities [ALT 2062 U/L] followed by jaundice one week later [bilirubin 1.5 rising to 26.3 mg/dl], hepatic failure and death 40 days after starting and 2 weeks after stopping crizotinib: Case 2).
- Zhang Q, Qin N, Wang J, Lv J, Yang X, Li X, Nong J, et al. Crizotinib versus platinum-based double-agent chemotherapy as the first line treatment in advanced anaplastic lymphoma kinase-positive lung adenocarcinoma. Thorac Cancer 2016; 7: 3-8. [PMC free article: PMC4718131] [PubMed: 26816533](Among 19 patients with previously-untreated, advanced, ALK-positive lung cancer treated with crizotinib compared to 12 patients given conventional chemotherapy, overall response rates were higher with crizotinib [83% vs 25%], but side effects were greater including visual disturbances, diarrhea and abnormal "liver function" in 28% vs 8%; no mention of clinically apparent liver injury).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Lorlatinib.[LiverTox: Clinical and Researc...]Review Lorlatinib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Alectinib.[LiverTox: Clinical and Researc...]Review Alectinib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Gefitinib.[LiverTox: Clinical and Researc...]Review Gefitinib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Erlotinib.[LiverTox: Clinical and Researc...]Review Erlotinib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Brigatinib.[LiverTox: Clinical and Researc...]Review Brigatinib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Crizotinib - LiverToxCrizotinib - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...