NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Bortezomib is a proteasome inhibitor and antineoplastic agent that is used in treatment of refractory multiple myeloma and certain lymphomas. Bortezomib is associated with a low rate of serum enzyme elevations during treatment and to rare instances of clinically apparent, acute liver injury.
Background
Bortezomib (bor tez’ oh mib) is an orally available, small molecule inhibitor of the 26S proteasome, the intracellular complex that degrades proteins involved in cell signaling and cell cycle regulation. Blocking proteasome activity prevents activation of factors involved in cell growth and resistance to chemotherapy induced apoptosis, leading to cancer cell death. Preclinical studies in vitro and in vivo suggested that bortezomib had activity against several hematologic malignancies. Clinical trials of bortezomib in patients with multiple myeloma showed improvements in progression free survival. Bortezomib received approval for use in the United States in 2003 for therapy of multiple myeloma and mantle cell lymphoma when given in combination with other chemotherapeutic agents. Bortezomib is available in powdered form in vials of 3.5 mg under the brand name Velcade. The typical starting dose is 1.3 mg/m2 intravenously or subcutaneously given once or twice weekly, usually in combination with other agents such as melphalan and prednisone. The recommended dosage and dose regimen varies by indication, tolerance and hepatic function. Common side effects include nausea, diarrhea, constipation, anorexia, fatigue, thrombocytopenia, neutropenia, anemia peripheral neuropathy, rash and fever. Uncommon, but potentially severe side effects include peripheral neuropathy, cardiac and pulmonary toxicity, bone marrow suppression and tumor lysis syndrome.
Hepatotoxicity
In large clinical trials of bortezomib, elevations in serum aminotransferase levels were common, occurring in ~10% of patients. However, values greater than 5 times the upper limit of normal (ULN) were rare, occurring in <1% of recipients. Cases of clinically apparent liver injury including acute liver failure have been reported in patients receiving bortezomib; however, in many instances multiple concomitant medications were being taken and the specific role of bortezomib in causing the liver injury was not always clear. The onset of injury was typically during the first cycle of therapy and usually, but not always recurred with retreatment. Cases characterized by acute hepatic necrosis and others by cholestatic hepatitis have been published, some of which were fatal. Hepatotoxici15ty is listed as a warning in the product label for bortezomib and monitoring of serum enzymes during treatment is recommended.
Bortezomib is typically given with other chemotherapeutic agents including cyclophosphamide and dexamethasone which can cause reactivation of hepatitis B. However, there have been no reports of reactivation of hepatitis B specifically attributable to bortezomib alone.
Likelihood score: C (probable cause of clinically apparent drug induced liver injury).
Mechanism of Injury
The mechanisms of liver injury accounting for serum enzyme elevations and hepatic toxicity during bortezomib therapy are not known. Bortezomib is metabolized in the liver largely through the CYP 3A4 pathway and liver injury may be related to production of a toxic intermediate. Bortezomib is susceptible to drug-drug interactions with agents that inhibit or induce hepatic CYP 3A4 activity.
Outcome and Management
Serum aminotransferase elevations above 5 times the upper limit of normal (if confirmed) should lead to dose reduction or temporary cessation. Clinically apparent liver injury should prompt immediate interruption of bortezomib therapy. Cases of hepatic failure attributed to bortezomib have been described, but no instance of chronic hepatitis or vanishing bile duct syndrome. There is little information on cross reactivity in risk for hepatic injury between bortezomib and other cancer chemotherapeutic agents, including the tyrosine kinase inhibitors and other proteasome inhibitors such as carfilzomib, but, because of the differences in chemical structure, there is little reason to suggest that there might be.
Drug Class: Antineoplastic Agents, Protein Kinase Inhibitors
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Bortezomib – Velcade®
DRUG CLASS
Antineoplastic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Bortezomib | 179324-69-7 | C19-H25-B-N4-O4 |
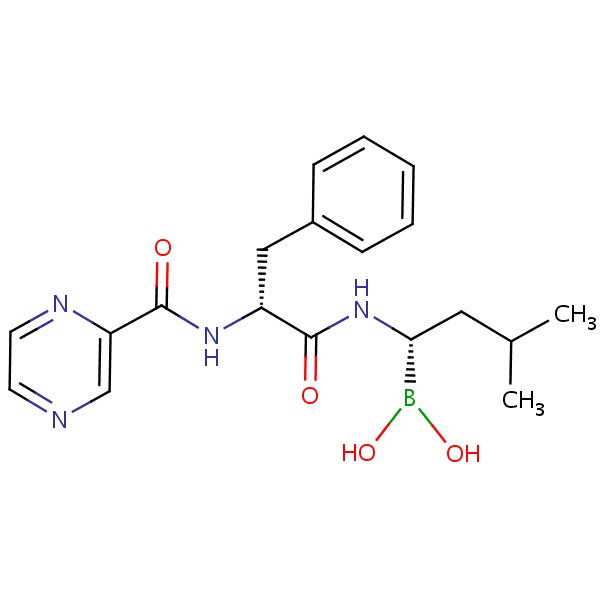 |
ANNOTATED BIBLIOGRAPHY
References updated: 30 September 2017
- Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999.(Review of hepatotoxicity published in 1999 before the availability of proteasome inhibitors such as bortezomib).
- DeLeve LD. Erlotinib. Cancer chemotherapy. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 556.(Review of hepatotoxicity of cancer chemotherapeutic agents published; bortezomib is listed as being implicated in causing hepatocellular injury).
- Chabner BA, Barnes J, Neal J, Olson E, Mujagic H, Sequist L, Wilson W, et al. Targeted therapies: tyrosine kinase inhibitors, monoclonal antibodies, and cytokines. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1731-54.(Textbook of pharmacology and therapeutics).
- Richardson PG, Barlogie B, Berenson J, Singhal S, Jagannath S, Irwin D, Rajkumar SV, et al. A phase 2 study of bortezomib in relapsed, refractory myeloma. N Engl J Med 2003; 348: 2609-17. [PubMed: 12826635](Among 193 patients with refractory multiple myeloma treated with bortezomib in cycles for up to 24 weeks, a clinical response occurred in 35% of patients and common side effects were nausea, diarrhea, fatigue, thrombocytopenia and neuropathy; no mention of ALT elevations or hepatotoxicity).
- Bortezomib (Velcade) for multiple myeloma. Med Lett Drugs Ther 2003; 45 (1161): 57-8. [PubMed: 12865865](Concise review of mechanism of action, efficacy, safety and cost of bortezomib shortly after its approval for use in the US; does not mention hepatotoxicity or serum enzyme elevations).
- Rosiñol L, Montoto S, Cibeira MT, Bladé. Bortezomib-induced severe hepatitis in multiple myeloma: a case report. Arch Intern Med 2005; 165: 464-5. [PubMed: 15738379](68 year old man with advanced refractory multiple myeloma developed septic shock on the 6th day of cycle 1 of therapy, with subsequent increase in liver enzymes [ALT 2865 U/L, LDH 6448 U/L] followed by rapid recovery, but recurrence with two subsequent cycles [peak bilirubin 2.8 mg/dL, ALT 2750 U/L, LDH 6129 U/L] and rapid recovery each time).
- Richardson PG, Sonneveld P, Schuster MW, Irwin D, Stadtmauer EA, Facon T, Harousseau JL, et al.; Assessment of Proteasome Inhibition for Extending Remissions (APEX) Investigators. Bortezomib or high-dose dexamethasone for relapsed multiple myeloma. N Engl J Med 2005; 352: 2487-98. [PubMed: 15958804](Among 669 patients with refractory multiple myeloma treated with multiple cycles of bortezomib or dexamethasone, response rates and survival were greater with bortezomib; common side effects were diarrhea, nausea, fatigue, constipation, peripheral neuropathy and thrombocytopenia; no mention of hepatotoxicity or ALT elevations).
- Cornelis T, Beckers EA, Driessen AL, van der Sande FM, Koek GH. Bortezomib-associated fatal liver failure in a haemodialysis patient with multiple myeloma. Clin Toxicol (Phila) 2012; 50: 444-5. [PubMed: 22462599](70 year old man with renal failure on hemodialysis and multiple myeloma developed jaundice ten days after the first dose of bortezomib and dexamethasone [bilirubin 8.0 mg/dL, ALT 114 U/L, Alk P 461 U/L], with progression to hepatic failure and death 2 months later).
- Paudice N, Farsetti S, Caroti L, Bandini S, Ciuti G, Tempestini A, Perfetto F, et al. [Severe recurrent intrahepatic cholestasis in systemic AL amyloidosis without obvious liver involvement: unexplained hepatic toxicity or a case of misdiagnosed liver amyloidosis?]. G Ital Nefrol 2012 Jan-Feb; 29 (1): 92-7. Italian.(50 year old woman with renal failure, multiple myeloma and amyloidosis developed jaundice 10 days after starting bortezomib and dexamethasone, which resolved despite continuing bortezomib, but recurred after stopping and was suspected to be due to amyloidosis).
- Kim GP, Mahoney MR, Szydlo D, Mok TS, Marshke R, Holen K, Picus J, et al. An international, multicenter phase II trial of bortezomib in patients with hepatocellular carcinoma. Invest New Drugs 2012; 30: 387-94. [PMC free article: PMC3896232] [PubMed: 20839030](Among 35 patients with hepatocellular carcinoma treated with 1 to 12 cycles of bortezomib, the confirmed response rate was only 4% and toxicity was common; ALT elevations above 5 times ULN occurred in 2 patients and one died to hepatic failure).
- Laubach J, Hideshima T, Richardson P, Anderson K. Clinical translation in multiple myeloma: from bench to bedside. Semin Oncol 2013; 40: 549-53. [PubMed: 24135399](Review of recent development of new agents to treat multiple myeloma, including bortezomib which showed activity against myeloma cell lines and was then evaluated clinically).
- Wang H, Guan F, Chen D, Dou QP, Yang H. An analysis of the safety profile of proteasome inhibitors for treating various cancers. Expert Opin Drug Saf 2014: 13: 1043-54. [PubMed: 25005844](Review of efficacy and safety of bortezomib and several second generation proteasome inhibitors including carfilzomib, marizomib, ixazomib and oprozomib; no discussion of hepatotoxicity or serum enzyme elevations).
- Till BG, Li H, Bernstein SH, Fisher RI, Burack WR, Rimsza LM, Floyd JD, DaSilva MA, et al. Phase II trial of R-CHOP plus bortezomib induction therapy followed by bortezomib maintenance for newly diagnosed mantle cell lymphoma: SWOG S0601. Br J Haematol 2016; 172: 208-18. [PMC free article: PMC4710555] [PubMed: 26492567](Among 65 patients with mantle cell lymphoma treated with 6 cycles of CHOP with bortezomib followed by bortezomib maintenance, during which adverse events included neuropathy in 72% of patients; no mention of ALT elevations or hepatotoxicity).
- Lu J, Chen WM, Geng CY, Durie BG, Huang XJ. Efficacy and safety of bortezomib in multiple myeloma patients with hepatitis B: a multicenter retrospective study. Chin Med J (Engl) 2016; 129: 274-8. [PMC free article: PMC4799569] [PubMed: 26831227](Retrospective review of outcome of bortezomib therapy in 25 HBsAg-positive patients with multiple myeloma [20 treated with nucleoside analogues for HBV] found no evidence of reactivation, ALT and HBV DNA levels remaining normal or negative).
- Jain A, Malhotra P, Suri V, Varma S, Das A, Mitra S. Cholestasis in a patient of multiple myeloma: a rare occurrence of bortezomib induced liver injury. Indian J Hematol Blood Transfus 2016; 32 (Suppl 1): 181-3. [PMC free article: PMC4925560] [PubMed: 27408386](A 54 year old man with multiple myeloma developed jaundice a few days into a second 4-week cycle of cyclosphosphamide, dexamethasone and bortezomib [bilirubin 15.5 mg/dL, ALT 367 U/L, Alk P 2456 U/L], recovering in 4 weeks and later tolerating cyclophosphamide and thalidomide).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Carfilzomib.[LiverTox: Clinical and Researc...]Review Carfilzomib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Ixazomib.[LiverTox: Clinical and Researc...]Review Ixazomib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Tumour lysis syndrome in multiple myeloma after bortezomib (VELCADE) administration.[J Cancer Res Clin Oncol. 2004]Tumour lysis syndrome in multiple myeloma after bortezomib (VELCADE) administration.Terpos E, Politou M, Rahemtulla A. J Cancer Res Clin Oncol. 2004 Oct; 130(10):623-5. Epub 2004 Jul 28.
- Treatment with the HIV protease inhibitor nelfinavir triggers the unfolded protein response and may overcome proteasome inhibitor resistance of multiple myeloma in combination with bortezomib: a phase I trial (SAKK 65/08).[Haematologica. 2016]Treatment with the HIV protease inhibitor nelfinavir triggers the unfolded protein response and may overcome proteasome inhibitor resistance of multiple myeloma in combination with bortezomib: a phase I trial (SAKK 65/08).Driessen C, Kraus M, Joerger M, Rosing H, Bader J, Hitz F, Berset C, Xyrafas A, Hawle H, Berthod G, et al. Haematologica. 2016 Mar; 101(3):346-55. Epub 2015 Dec 11.
- Resensitising proteasome inhibitor-resistant myeloma with sphingosine kinase 2 inhibition.[Neoplasia. 2022]Resensitising proteasome inhibitor-resistant myeloma with sphingosine kinase 2 inhibition.Bennett MK, Li M, Tea MN, Pitman MR, Toubia J, Wang PP, Anderson D, Creek DJ, Orlowski RZ, Gliddon BL, et al. Neoplasia. 2022 Jan; 24(1):1-11. Epub 2021 Nov 23.
- Bortezomib - LiverToxBortezomib - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...