NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Barbiturates are structurally related compounds with sedative and hypnotic activities, some of which (phenobarbital and mephobarital) are also used as anticonvulsants. Phenobarbital has been clearly linked to cases of idiosyncratic acute liver injury, resembling the immunoallergic hepatotoxicity of other aromatic anticonvulsants such as phenytoin and carbamazepine. In contrast, the other conventional sedative barbiturates have not been linked to serum enzyme elevations during therapy and clinically apparent acute liver injury due to the sedative barbiturates is extremely rare, if it occurs at all.
Background
Barbiturates are a family of compounds that have sedative and hypnotic activities and act as nonselective central nervous system (CNS) depressants. The barbiturates were introduced into medical practice in the early 20th century, used as a sleeping aid and in treatment of schizophrenia. However, with chronic use they often cause psychological and physical dependence and have serious adverse effects, including agitation, respiratory depression and daytime somnolence. Phenobarbital (fee" noe bar' bi tal) given in lower doses was found to have anticonvulsant activity and has been used extensively as an anticonvulsant, particularly in children. Phenobarbital appears to act by suppression of spread of seizure activity by enhancing the effect of gamma aminobutyric acid (GABA). Phenobarbital has been linked to instances of acute liver injury and is discussed separately as an anticonvulsant. The barbiturates that are used as sedatives and hypnotics, in contrast, have not been linked to cases of acute or chronic liver injury and are discussed together below.
Amobarbital, pentobarbital and secobarbital are used as sedatives and hypnotics and not as anticonvulsants. These and many other synthetic barbiturates were introduced into medical use in the United States in the early part of the 20th century as sedatives, hypnotics (short term treatment of insomnia) and preanesthetic agents. They are now rarely used, having been replaced by more effective and better tolerated sedatives and hypnotics such as the benzodiazepines and benzodiazepine receptor agonists. Amobarbital (am" oh bar' bi tal) and pentobarbital (pen” toe bar’ bi tal) are currently available, but only as solutions for parenteral administration, being used largely as preanesthetic agents. Secobarbital is available as a 100 mg capsule generically and under the brand name Seconal. Current indications for the barbiturates include short term treatment of insomnia and as a preanesthetic agent or sedative for a minor procedure or imaging study. The recommended dose of secobarbital in adults is 100 mg at bedtime or 200 to 300 mg 1 to 2 hours before surgery. Barbiturates that are no longer available in the United States include butalbital, butabarbital, mephobarbital, methohexital, and thiopental. Secobarbital, amobarbital and pentobarbital are classified as a Schedule II substances, indicating that they have definite potential for physical and psychological dependence and abuse. Frequent side effects include drowsiness, sedation, impairment of mental and physical abilities, hypotension, bradycardia, syncope, nausea, vomiting, headache, and skin rash. When given chronically, the barbiturates can cause psychological and physical dependence and their withdrawal can be associated with agitation, irritability, confusion, insomnia, and vivid dreams.
Hepatotoxicity
Despite wide scale previous use, there is little evidence that the conventional barbiturates used as sedatives or preanesthetic agents can cause liver injury, either serum enzyme elevations during therapy or clinically apparent acute liver disease. There have been no reports of liver injury associated with secobarbital, butabarbital or amobarbital. The barbiturates can cause allergic reactions and skin rashes, which may be accompanied by mild liver injury. Paradoxically, phenobarbital has been linked to many instances of hypersensitivity reactions with accompanying liver disease that can be severe, including drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome, Stevens Johnson syndrome [SJS] and toxic epidermal necrolysis [TEN], while the other barbiturates have not. The barbiturates are also potent inducers of many hepatic enzymes. In animal models, phenobarbital causes enlargement of hepatocytes with marked increases in protein and lipid content of the endoplasmic reticulum, causing an increased granularity to the hepatocyte cytoplasm. Hepatic enzymes that are induced with chronic barbiturate use include multiple microsomal enzymes such as CYP 1A2, 2C9, 2C19 and 3A4 as well as glucuronyl transferase, delta-aminolevulinic acid, and aldehyde dehydrogenase. Thus, chronic use of barbiturates may increase the metabolism of many drugs and endogenous substances including steroid hormones, cholesterol, bile salts and vitamins.
Likelihood score for amobarbital, pentobarbital and secobarbital: E (unlikely causes of clinically apparent liver injury).
Mechanism of Injury
The reason why phenobarbital, but not amobarbital, butabarbital or secobarbital has been linked to hepatotoxicity is not known, but may merely be that the conventional barbiturates are infrequently used and used in relatively low doses for short periods only. The mechanism of phenobarbital hepatotoxicity is thought to be hypersensitivity and it commonly presents with DRESS syndrome. Hypersensitivity reactions can occur with other barbiturates, but hepatic involvement has not been described in the literature.
Drug Class: Sedatives and Hypnotics
Drugs in the Subclass, Barbiturates: Amobarbital, Butabarbital, Phenobarbital, Secobarbital
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Amobarbital – Generic, Amytal®
Phenobarbital – Generic
Secobarbital – Generic, Seconal®
DRUG CLASS
Sedatives and Hypnotics
Product labeling at DailyMed, National Library of Medicine, NIH
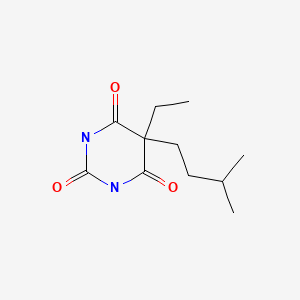
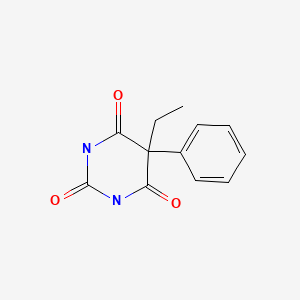
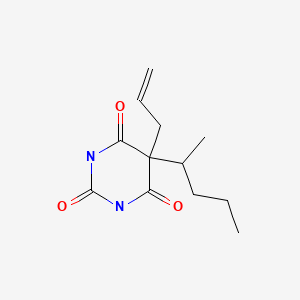
CHEMICAL FORMULAS AND STRUCTURES
ANNOTATED BIBLIOGRAPHY
References updated: 03 October 2021
- Zimmerman HJ. Anticonvulsants. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp.498-516.(Expert review of anticonvulsants and liver injury published in 1999; mentions that liver injury from phenobarbital is rare, but it has been implicated in at least 15 cases of clinically apparent injury, both hepatocellular and cholestatic; potential hepatotoxicity of other barbiturates is not discussed).
- Pirmohamed M, Leeder SJ. Anticonvulsant agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013: pp 423-442.(Review of anticonvulsant induced liver injury mentions that phenobarbital is the oldest aromatic anticonvulsant and can cause elevations in serum GGT and Alk P but is a rare cause of liver injury, reported cases usually associated with hypersensitivity reactions).
- Smith MD, Metcalf CS, Wilcox KS. Pharmacology of the epilepsies. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 303-26.(Textbook of pharmacology and therapeutics).
- Mihic J, Mayfield J, Harris RA. Barbiturates. Hypnotics and sedatives. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 339-54.(Textbook of pharmacology and therapeutics mentions that the barbiturates were once used extensively, but have been replaced by the much safer benzodiazepines).
- Welton DG. Exfoliative dermatitis and hepatitis due to phenobarbital. J Am Med Assoc. 1950;143(3):232–4. [PubMed: 15415251](25 year old pregnant woman developed rash, followed by facial and peripheral edema, itching, erythema and exfoliation, fever to 104oC after 6 weeks of phenobarbital [white blood count 73,000, 32% eosinophils], jaundiced for a few weeks but ultimately recovered).
- McGeachy TE, Bloomer WE. The phenobarbital sensitivity syndrome. Am J Med. 1953;14:600–4. [PubMed: 13040367](3 cases of severe phenobarbital reactions seen between 1933 and 1947; two men and one woman, ages 27 to 41 years, developing rash, desquamation, fever, delirium and jaundice within 1-2 weeks of starting drug; one instance was fatal).
- Pagliaro L, Campesi G, Aguglia F. Barbiturate jaundice. Report of a case due to a barbital-containing drug, with positive rechallenge to phenobarbital. Gastroenterology. 1969;56:938–43. [PubMed: 4238546](31 year old woman developed rash, fever, facial edema after 2 doses of "barbital" by 7 days developed jaundice [bilirubin 24.1 mg/dL, ALT 200 U/L, ALk P 15 BU], with prolonged jaundice; rechallenge with phenobarbital caused recurrence of fever, rash and jaundice [19 mg/dL]; three biopsies were done, but vanishing bile duct syndrome was evidently not present).
- Weisburst M, Self T, Peace R, Cooper J. Jaundice and rash associated with the use of phenobarbital and hydrochlorothiazide. South Med J. 1976;69:126–7. [PubMed: 128822](18 year old woman developed rash followed by fever, anorexia, lymphadenopathy and jaundice 6 weeks after starting phenobarbital for hypertension [bilirubin 7.2 mg/dL, AST 250 U/L, Alk P 350 U/L], resolving rapidly although no mention of drug being stopped).
- Shapiro PA, Antonioli DA, Peppercorn MA. Barbiturate-induced submassive hepatic necrosis. Am J Gastroenterol. 1980;74:270–3. [PubMed: 7468565](71 year old woman developed rash on phenytoin and was switched to mephobarbital and 3 months later developed anorexia, fatigue persisting for 6 weeks to onset of jaundice [bilirubin 5.3 mg/dL, ALT 837 U/L, Alk P 320 U/L], improved slowly but relapsed with restarting phenobarbital; biopsy showed submassive necrosis, ultimately recovering completely; no features of hypersensitivity).
- Lane T, Peterson EA. Hepatitis as a manifestation of phenobarbital hypersensitivity. South Med J. 1984;77:94. [PubMed: 6695234](4 year old boy developed fever and rash about 1 week after starting phenobarbital and 1 week later found to have ALT 273 U/L [no bilirubin reported], rapid improvement with stopping).
- Knutsen AP, Anderson J, Satayaviboon S, Slavin RG. Immunologic aspects of phenobarbital hypersensitivity. J Pediatr. 1984;105:558–63. [PubMed: 6332892](Seven patients with onset of hypersensitivity 2 to 23 days after starting phenobarbital with fever, pruritic skin rash becoming confluent and desquamating; 2 patients had abnormal liver tests, but without jaundice; 3 had eosinophilia, 3 IgE elevations; 2 decreased C4 levels; several had positive lymphocyte stimulation tests to phenytoin or phenobarbital).
- Roberts EA, Spielberg SP, Goldbach M, Phillips MJ. Phenobarbital hepatotoxicity in an 8-month-old infant. J Hepatol. 1990;10:235–9. [PubMed: 2332596](8 month old boy with seizures given phenobarbital for 2 weeks developed rash followed by fever with eosinophilia, atypical lymphocytes [bilirubin 2.9 mg/dL, ALT 430 U/L, Alk P 135 U/L], slow recovery, positive lymphocyte cytotoxicity test).
- Dayrell-Hart B, Steinberg SA, VanWinkle TJ, Farnbach GC. Hepatotoxicity of phenobarbital in dogs: 18 cases (1985-1989). J Am Vet Med Assoc. 1991;199:1060–6. [PubMed: 1748613](Description of 18 dogs with phenobarbital induced liver injury, all had sedation and ataxia, 3 were icteric [bilirubin 0.2-4.9 mg/dL, ALT 38-1,830 U/L, Alk P 301-5,240 U/L], liver biopsies showing variable degrees of necrosis, inflammation and fibrosis; 9 dogs died or were euthanized, whereas the others appeared to recover completely).
- Di Martino V, Mallat A, Duvoux C, Zafrani ES, Dhumeaux D. Gastroenterol Clin Biol. 1994;18:904–5. [Severe hepatitis caused by phenobarbital] [PubMed: 7875406](Patient on phenobarbital for 1 month developed fever and rash followed by adenopathy and jaundice [bilirubin 8.7 mg/dL, ALT 22 times ULN, elevated prothrombin time], treated with prednisone and recovered within 1 month).
- Wallace SJ. A comparative review of the adverse effects of anticonvulsants in children with epilepsy. Drug Saf. 1996;15:378–93. [PubMed: 8968693](Systematic review; ALT elevations occur in 4% of children on phenytoin, 6% on valproate, 1% on carbamazepine, but not with phenobarbital; skin rash and Stevens-Johnson syndrome discussed related to phenobarbital).
- Foster SF, Church DB, Watson AD. Effects of phenobarbitone on serum biochemical tests in dogs. Aust Vet J. 2000;78:23–6. [PubMed: 10736679](Comparison of 10 dogs receiving phenobarbital for seizures with 10 control dogs found slightly higher levels of alkaline phosphatase in treated dogs, with no differences in GGT or bilirubin and mild increases in ALT).
- Müller PB, Taboada J, Hosgood G, Partington BP, VanSteenhouse JL, Taylor HW, Wolfsheimer KJ. Effects of long-term phenobarbital treatment on the liver in dogs. J Vet Intern Med. 2000;14:165–71. [PMC free article: PMC7197517] [PubMed: 10772488](12 normal dogs who were given phenobarbital for 29 weeks developed slight rise in Alk P [~50 to 270 U/L] and ALT [27 to 65 U/L], with no change in serum bilirubin, and biopsy showing increase in hepatocyte size and cytoplasmic granularity compatible with enzyme induction, rather than injury or necrosis).
- Gaskill CL, Miller LM, Mattoon JS, Hoffmann WE, Burton SA, Gelens HC, Ihle SL, et al. Liver histopathology and liver and serum alanine aminotransferase and alkaline phosphatase activities in epileptic dogs receiving phenobarbital. Vet Pathol. 2005 Mar;42:147–60. [PubMed: 15753468](Liver biopsies from dogs receiving phenobarbital showed increase in hepatocyte size, granularity and mild injury, but similar although milder changes were found in control dogs; serum enzymes were mildly increased in phenobarbital treated dogs as was CYP 2B activity in liver).
- Lachgar T, Touil Y. Allerg Immunol (Paris). 2001;33:173–5. [The drug hypersensitivity syndrome or DRESS syndrome to phenobarbital] [PubMed: 11434197](78 year old woman developed rash and fever 3 weeks after starting phenobarbital [ALT 3 times ULN, eosinophilia], resolving within a month of stopping).
- Autret-Leca E, Norbert K, Bensouda-Grimaldi L, Jonville-Béra AP, Saliba E, Bentata J, Barthez-Carpentier MA. Arch Pediatr. 2007;14:1439–41. [DRESS syndrome, a drug reaction which remains bad known from paediatricians] [PubMed: 17997290](6 year old girl with epilepsy developed rash and fever 3 weeks after starting phenobarbital, with eosinophilia [ALT 5 times ULN, Alk P 1.5 times ULN], improving clinically with corticosteroid therapy; switched to topiramate and valproate without recurrence).
- Björnsson E. Hepatotoxicity associated with antiepileptic drugs. Acta Neurol Scand. 2008;118:281–90. [PubMed: 18341684](Review of all anticonvulsants; phenytoin hepatotoxicity usually occurs as a part of a hypersensitivity syndrome, in 1:10,000 to 1:50,000 persons, 100 published cases, mean onset at 4 weeks, 13% mortality; in contrast, phenobarbital has only rarely been reported to cause liver injury).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, 18 cases were attributed to anticonvulsants, no case was attributed to phenobarbital or other barbiturates).
- Ferrajolo C, Capuano A, Verhamme KM, Schuemie M, Rossi F, Stricker BH, Sturkenboom MC. Drug-induced hepatic injury in children: a case/non-case study of suspected adverse drug reactions in VigiBase. Br J Clin Pharmacol. 2010;70:721–8. [PMC free article: PMC2997312] [PubMed: 21039766](Worldwide pharmacovigilance database contained 9036 hepatic adverse drug reactions in children, phenobarbital accounting for 41 cases [0.4%] for an adjusted odds ratio of 6.6; no other barbiturate listed among the 41 most frequently implicated agents).
- Molleston JP, Fontana RJ, Lopez MJ, Kleiner DE, Gu J, Chalasani N., Drug-Induced Liver Injury Network. Characteristics of idiosyncratic drug-induced liver injury in children: results from the DILIN Prospective Study. J Pediatr Gastroenterol Nutr. 2011;53:182–9. [PMC free article: PMC3634369] [PubMed: 21788760](Among 30 children with drug induced liver injury enrolled in a prospective US database between 2004 and 2008, 8 were due to anticonvulsants [lamotrigine in 3, valproate in 3, phenytoin in 1 and carbamazepine in 1], none were attributed to phenobarbital or other barbiturates).
- Sedky K, Nazir R, Joshi A, Kaur G, Lippmann S. Which psychotropic medications induce hepatotoxicity? Gen Hosp Psychiatry. 2012;34:53–61. [PubMed: 22133982](Review of the hepatotoxicity of psychotropic medications; barbiturates are not discussed).
- Gaur S, Agnihotri R. Phenobarbital induced Stevens-Johnson syndrome in a child. Indian J Pharmacol. 2012;44:531–2. [PMC free article: PMC3469965] [PubMed: 23087523](12 year old boy developed fever and rash 7 days after switching from phenytoin to phenobarbital [bilirubin 3.1 mg/dL, ALT 187 U/L, Alk P 400 U/L], resolving rapidly upon stopping).
- Ruggiero A, Buonuomo PS, Maurizi P, Cefalo MG, Corsello M, Riccardi R. Stevens-Johnson syndrome in children receiving phenobarbital therapy and cranial radiotherapy. J Neurooncol. 2007;85:213–5. [PubMed: 17589805](Two children, one boy and one girl, ages 6 and 7 developed rash [SJS/TEN] 26 and 28 days after starting phenobarbital after cranial radiotherapy for brain tumors; liver test results not provided).
- Manuyakorn W, Siripool K, Kamchaisatian W, Pakakasama S, Visudtibhan A, Vilaiyuk S, Rujirawat T, et al. Phenobarbital-induced severe cutaneous adverse drug reactions are associated with CYP2C19*2 in Thai children. Pediatr Allergy Immunol. 2013;24:299–303. [PubMed: 23551241](Among 40 cases of drug induced severe cutaneous reactions [DRESS or SJS/TEN] seen over 20 years at a single referral hospital in Thailand, 20 were due to phenobarbital, 17 to phenytoin and 3 to carbamazepine; among cases due to phenobarbital, ALT levels average 71 U/L [range 26-4243], weak association found with a CYP2C19*2 variant).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, none were attributed to a barbiturate).
- Mason KP, Zurakowski D, Connor L, Karian VE, Fontaine PJ, Sanborn PA, Burrows PE. Infant sedation for MR imaging and CT: oral versus intravenous pentobarbital. Radiology. 2004;233:723–8. [PubMed: 15516603](Retrospective review of 2164 infants undergoing 2419 magnetic resonance imaging sessions requiring sedation and given either oral or iv pentobarbital, found that time to onset was faster with iv drug [7 vs 18 min], but quality of sedation and time to recovery were similar as were adverse events [1.3% vs 0.8%; none were liver related], the general findings favoring oral administration).
- López-Muñoz F, Ucha-Udabe R, Alamo C. The history of barbiturates a century after their clinical introduction. Neuropsychiatr Dis Treat. 2005;1:329–43. [PMC free article: PMC2424120] [PubMed: 18568113](History of the discovery of the barbiturates and development of synthetic formulations, about 50 of which came to market starting with phenobarbital [Luminol] in 1912, pentobarbital [Neonal] in 1922, most being used as sleeping aids and as therapy of schizophrenia, and later found to have anticonvulsant activity and to be useful in sedation and preanesthesia, but more recently replaced with safer and less addictive therapies).
- McCleary K, Barrash J, Granner M, Manzel K, Greider A, Jones R. The safety and efficacy of propofol as a replacement for amobarbital in intracarotid Wada testing of presurgical patients with epilepsy. Epilepsy Behav. 2018;78:25–29. [PubMed: 29169082](The difficulty in obtaining amobarbital led to its replacement with propofol in mild sedation, and comparison of efficacy and safety using historical controls suggested similar rates of successful anesthesia and similar rates of adverse events; no mention of liver-related symptoms).
- Schlatter J, Kabiche S, Sellier N, Fontan JE. Oral pentobarbital suspension for children sedation during MR imaging. Ann Pharm Fr. 2018;76:286–290. [PubMed: 29655484](Among 81 children undergoing magnetic resonance imaging given oral pentobarbital for sedation, the success of obtaining imaging varied by age, being 100% below age 1 but only 42% in 4 to 8 year olds; adverse events were rare but [from a literature review] could include oxygen desaturation, prolonged sedation, paradoxical excitement, and vomiting; no mention of liver injury).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Anticonvulsants.[LiverTox: Clinical and Researc...]Review Anticonvulsants.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Carbamazepine replacement of phenytoin, phenobarbital and primidone in a rehabilitation setting: effects on seizure control.[Brain Inj. 1989]Carbamazepine replacement of phenytoin, phenobarbital and primidone in a rehabilitation setting: effects on seizure control.Wroblewski BA, Glenn MB, Whyte J, Singer WD. Brain Inj. 1989 Apr-Jun; 3(2):149-56.
- Quantitation of amobarbital, butalbital, pentobarbital, phenobarbital, and secobarbital in urine, serum, and plasma using gas chromatography-mass spectrometry (GC-MS).[Methods Mol Biol. 2010]Quantitation of amobarbital, butalbital, pentobarbital, phenobarbital, and secobarbital in urine, serum, and plasma using gas chromatography-mass spectrometry (GC-MS).Johnson LL, Garg U. Methods Mol Biol. 2010; 603:65-74.
- [On the history of barbiturates].[Dan Medicinhist Arbog. 2015][On the history of barbiturates].Norn S, Permin H, Kruse E, Kruse PR. Dan Medicinhist Arbog. 2015; 43:133-51.
- Review Established antiepileptic drugs.[Baillieres Clin Neurol. 1996]Review Established antiepileptic drugs.Perucca E. Baillieres Clin Neurol. 1996 Dec; 5(4):693-722.
- Barbiturates - LiverToxBarbiturates - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...